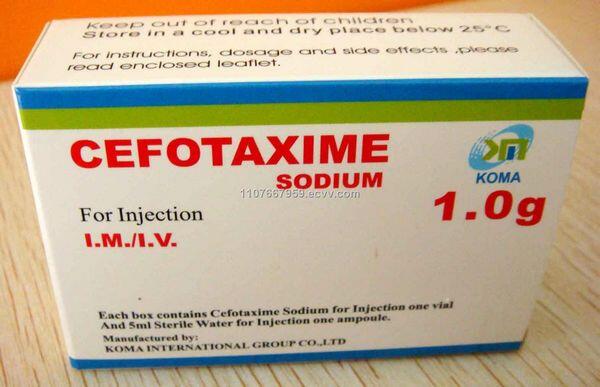
Cefotaxime is a semisynthetic, third generation cephalosporin antibiotic.
Uses
Cefotaxime is used for the treatment of serious bone and joint infections, serious intra-abdominal and gynecologic infections (including peritonitis, endometritis, pelvic inflammatory disease, pelvic cellulitis), meningitis and other CNS infections, serious lower respiratory tract infections (including pneumonia), bacteremia/septicemia, serious skin and skin structure infections, and serious urinary tract infections caused by susceptible bacteria.
The drug also is used in the treatment of gonorrhea, typhoid fever and other infections caused by Salmonella, infections caused by Vibrio parahaemolyticus or V. vulnificus, and Lyme disease.
Cefotaxime also has been used for perioperative prophylaxis.
Prior to initiation of cefotaxime therapy, appropriate specimens should be obtained for identification of the causative organism and in vitro susceptibility tests. If cefotaxime therapy is started pending results of susceptibility tests, it should be discontinued if the causative organism is found to be resistant to the drug.
Because resistant strains of some organisms, especially Enterobacter, Ps. aeruginosa, and Serratia, have developed during cefotaxime therapy, it is important that appropriate specimens be obtained periodically until the infection is eradicated and cefotaxime is discontinued.
The manufacturer states that in certain cases of confirmed or suspected gram-positive or gram-negative sepsis or in the empiric treatment of other serious infections when the causative organism has not been identified, cefotaxime may be used concomitantly with an aminoglycoside pending results of in vitro susceptibility tests.
In infections which fail to respond to cefotaxime although in vitro tests indicate that the causative organism is susceptible to the drug, the presence of undrained abscesses or vascular infections should be suspected.
The possibility that the organism may be tolerant to cefotaxime should also be considered. (See Resistance.) Use of cefotaxime does not replace surgical procedures such as incision and drainage when indicated.
Gram-positive Aerobic Bacterial Infections
Cefotaxime is used in the treatment of lower respiratory tract infections caused by susceptible Streptococcus pneumoniae, S. pyogenes (group A b-hemolytic streptococci), other streptococci (except enterococci), or Staphylococcus aureus (penicillinase-producing and nonpenicillinase-producing strains); genitourinary tract infections caused by susceptible S. aureus, S. epidermidis, or enterococci; gynecologic infections caused by susceptible S. epidermidis or streptococci (including enterococci); skin and skin structure infections caused by susceptible S. aureus, S. epidermidis, group A b-hemolytic streptococci, or other streptococci (including enterococci); intra-abdominal infections caused by susceptible streptococci; or bone and joint infections caused by susceptible S. aureus, group A b-hemolytic streptococci, or other streptococci.
Cefotaxime generally should not be used in the treatment of infections caused by gram-positive bacteria when a penicillin or a first generation cephalosporin could be used. Although cefotaxime has been effective in the treatment of cellulitis, wound infections, septicemia, and lower respiratory tract infections caused by susceptible staphylococci or streptococci, treatment failures have been reported when the drug was used in the treatment of osteomyelitis caused by S. aureus.
Gram-negative Aerobic Bacterial Infections
Cefotaxime is used in the treatment of lower respiratory tract infections caused by susceptible Escherichia coli, Klebsiella, Haemophilus influenzae (including ampicillin-resistant strains), H. parainfluenzae, Proteus mirabilis, indole-positive Proteus, Serratia marcescens, or Enterobacter; genitourinary tract infections caused by susceptible Citrobacter, Enterobacter, E. coli, Klebsiella, P. mirabilis, Providencia stuartii (formerly group B Proteus inconstans), Pseudomonas, Morganella morganii, Providencia rettgeri, P. vulgaris, S. marcescens, or Neisseria gonorrhoeae; intra-abdominal and gynecologic infections caused by susceptible E. coli, Enterobacter, Klebsiella, or P. mirabilis; bacteremia or septicemia caused by susceptible E. coli, Klebsiella, or S. marcescens; skin and skin structure infections caused by susceptible E. coli, Enterobacter, Klebsiella, P. mirabilis, M. morganii, P. rettgeri, P. vulgaris, Pseudomonas, or S. marcescens; or bone and joint infections caused by susceptible P. mirabilis.
It has been suggested that certain parenteral cephalosporins (i.e., cefepime, cefotaxime, ceftizoxime, ceftriaxone, ceftazidime) may be drugs of choice for the treatment of many infections caused by susceptible Enterobacteriaceae, including susceptible strains of E. coli, K. pneumoniae, P. rettgeri, M. morganii, P. vulgaris, P. stuartii, or Serratia; an aminoglycoside (amikacin, gentamicin, tobramycin) usually is used concomitantly in severe infections. Although cefotaxime has been effective when used in the treatment of infections caused by susceptible Ps. aeruginosa, other anti-infectives generally are preferred for the treatment of pseudomonal infections.
Because most strains of Ps. aeruginosa require high concentrations of the drug for in vitro inhibition and resistant strains have developed during cefotaxime therapy, an aminoglycoside should be used concomitantly if cefotaxime is used in any infection where Ps. aeruginosa may be present.
Anaerobic and Mixed Aerobic-Anaerobic Bacterial Infections
Cefotaxime has been used in the treatment of skin and skin structure infections, intra-abdominal infections, or gynecologic infections caused by susceptible Bacteroides (including B. fragilis), Clostridium, Fusobacterium (including F. nucleatum), or anaerobic gram-positive cocci (including Peptococcus and Peptostreptococcus); however, cefotaxime is not considered a drug of choice for these infections. Cefotaxime has been effective when used in the treatment of mixed aerobic-anaerobic infections, including intra-abdominal and gynecologic infections (see Uses: Pelvic Inflammatory Disease). Because many strains of B. fragilisare resistant to cefotaxime, some clinicians recommend that cefotaxime not be used alone for the treatment of serious intra-abdominal infections when B. fragilis may be present.
Meningitis and Other CNS Infections
Cefotaxime is used in neonates, children, or adults for the treatment of meningitis and ventriculitis caused by susceptible strains of H. influenzae, N. meningitidis, or S. pneumoniae. The drug also has been used for the treatment of meningitis and other CNS infections caused by susceptible Enterobacteriaceae (e.g., Escherichia coli, Klebsiella pneumoniae). Cefotaxime is ineffective in and should not be used alone for empiric treatment of meningitis when Listeria monocytogenes, enterococci, staphylococci, or Pseudomonas aeruginosa may be involved.
Empiric Treatment of Meningitis
Pending results of CSF culture and in vitro susceptibility testing, the most appropriate anti-infective regimen for empiric treatment of suspected bacterial meningitis should be selected based on results of CSF Gram stain and antigen tests, age of the patient, the most likely pathogen(s) and source of infection, and current patterns of bacterial resistance within the hospital and local community. When results of culture and susceptibility tests become available and the pathogen is identified, the empiric anti-infective regimen should be modified (if necessary) to ensure that the most effective regimen is being administered.
There is some evidence that short-term adjunctive therapy with IV dexamethasone may decrease the incidence of audiologic and/or neurologic sequelae in infants and children with H. influenzae meningitis and possibly may provide some benefit in patients with S. pneumoniae meningitis. While such therapy is controversial, the American Academy of Pediatrics (AAP) and other clinicians suggest that use of adjunctive dexamethasone therapy be considered during the initial 2-4 days of anti-infective therapy in infants and children 6-8 weeks of age or older with known or suspected bacterial meningitis, especially in those with suspected or proven H. influenzae infection. (See Uses: Bacterial Meningitis in the Corticosteroids General Statement 68:04 and see Dexamethasone 68:04.)
Bacterial meningitis in neonates usually is caused by S. agalactiae (group B streptococci), L. monocytogenes, or aerobic gram-negative bacilli (e.g., E. coli, K. pneumoniae). The AAP recommends that neonates 4 weeks of age or younger with suspected bacterial meningitis receive an empiric regimen of IV ampicillin and an aminoglycoside pending results of CSF culture and susceptibility testing. Alternatively, neonates can receive an empiric regimen of IV ampicillin and IV cefotaxime or IV ceftazidime (with or without gentamicin). Because frequent use of cephalosporins in neonatal units may result in rapid emergence of resistant strains of some gram-negative bacilli (e.g., Enterobacter cloacae, Klebsiella, Serratia), the AAP cautions that cephalosporins should be used for empiric treatment of meningitis in neonates only if gram-negative bacterial meningitis is strongly suspected. Consideration should be given to including IV vancomycin in the initial empiric regimen if S. pneumoniae, enterococci, or staphylococci is suspected.
Because ceftriaxone should be used with caution in neonates who are hyperbilirubinemic (especially those born prematurely), cefotaxime may be the preferred cephalosporin in neonates.
Alternatively, because premature, low-birthweight neonates are at increased risk for nosocomial infection caused by staphylococci or gram-negative bacilli, some clinicians suggest that these neonates receive an empiric regimen of IV ceftazidime and IV vancomycin. In infants beyond the neonatal stage who are younger than 3 months of age, bacterial meningitis may be caused by S. agalactiae, L. monocytogenes, Haemophilus influenzae, S. pneumoniae, N. meningitidis, or aerobic gram-negative bacilli (e.g., E. coli, K. pneumoniae).
The empiric regimen recommended for infants in this age group is IV ampicillin and either IV cefotaxime or IV ceftriaxone. Consideration should be given to including IV vancomycin in the initial empiric regimen if S. pneumoniae is suspected, especially when there are gram-positive diplococci on the CSF gram stain characteristic of pneumococci or positive bacterial antigen test results. In children 3 months through 17 years of age, bacterial meningitis usually is caused by N. meningitidis, S. pneumoniae, or H. influenzae, and the most common cause of bacterial meningitis in adults 18-50 years of age is N. meningitidis or S. pneumoniae.
Most clinicians recommend that children 3 months through 17 years of age and adults 18-50 years of age receive IV cefotaxime or IV ceftriaxone for empiric therapy of suspected bacterial meningitis; an alternative regimen in children 3 months through 17 years of age is IV ampicillin and IV chloramphenicol. In addition, because of the increasing incidence of penicillin-resistant S. pneumoniae with reduced susceptibility to cephalosporins, the AAP and others suggest that the initial empiric regimen can include IV vancomycin (with or without rifampin) pending results of in vitro susceptibility tests; vancomycin and rifampin should be discontinued if the causative organism is found to be susceptible to cephalosporins.
The Centers for Disease Control and Prevention (CDC) and some clinicians have recommended that vancomycin be added to the empiric regimen in areas where there have been reports of highly penicillin-resistant strains of S. pneumoniae, but other clinicians suggest that use of cefotaxime or ceftriaxone in conjunction with vancomycin provides the optimal initial empiric regimen. While L. monocytogenesmeningitis is relatively rare in this age group, the empiric regimen should include ampicillin if L. monocytogenes is suspected. In adults older than 50 years of age, bacterial meningitis usually is caused by S. pneumoniae, L. monocytogenes, N. meningitidis, or aerobic gram-negative bacilli, and the empiric regimen recommended for this age group is IV ampicillin given in conjunction with IV cefotaxime or IV ceftriaxone. If S. pneumoniae is suspected, the empiric regimen also should include IV vancomycin (with or without rifampin); vancomycin and rifampin should be discontinued if the causative organism is found to be susceptible to the cephalosporin.
Meningitis Caused by Streptococcus pneumoniae
IV cefotaxime and IV ceftriaxone are considered drugs of choice for the treatment of meningitis caused by S. pneumoniae. While cefotaxime and ceftriaxone generally have been considered the drugs of choice for the treatment of meningitis caused by penicillin-resistant S. pneumoniae, treatment failures have been reported when the drugs were used alone for the treatment of meningitis caused by strains of S. pneumoniae with intermediate or high-level penicillin resistance (i.e., penicillin MIC 0.1 mcg/mL or greater).
In addition, strains of S. pneumoniae with reduced susceptibility to cephalosporins have been reported with increasing frequency, and use of cefotaxime or ceftriaxone alone may be ineffective for the treatment of meningitis caused by these strains. The prevalence of S. pneumoniae with reduced susceptibility to penicillin and/or cephalosporins varies geographically, and clinicians should be aware of the prevalence and pattern of S. pneumoniae drug resistance in the local community to optimize empiric regimens and initial therapy for serious pneumococcal infections.
Because susceptibility can no longer be assumed, S. pneumoniae isolates should be routinely tested for in vitro susceptibility. If anti-infective therapy in a patient with meningitis is initiated with an empiric regimen of IV cefotaxime and IV vancomycin (with or without rifampin) and results of culture and in vitro susceptibility testing indicate that the pathogen involved is a strain of S. pneumoniae susceptible to cefotaxime and susceptible or resistant to penicillin, vancomycin can be discontinued and therapy completed using cefotaxime alone. If the isolate is found to have reduced susceptibility to cefotaxime and penicillin, both IV cefotaxime and IV vancomycin (with or without rifampin) usually are continued.
If the patient’s condition does not improve or worsens or results of a second repeat lumber puncture (performed 24-36 hours after initiation of anti-infective therapy) indicate that the anti-infective regimen has not eradicated or reduced the number of pneumococci in CSF, rifampin probably should be added to the regimen or vancomycin discontinued and replaced with rifampin. If meningitis is caused by S. pneumoniae highly resistant to cefotaxime (i.e., MIC 2-4 mcg/mL or greater), consultation with an infectious disease expert is recommended.
Meningitis Caused by Haemophilus influenzae
IV cefotaxime and IV ceftriaxone are considered drugs of choice for the treatment of meningitis caused by susceptible H. influenzae (including penicillinase-producing strains). The AAP suggests that children with meningitis possibly caused by H. influenzae receive an initial treatment regimen of cefotaxime, ceftriaxone, or a regimen of ampicillin given in conjunction with chloramphenicol; some clinicians prefer cefotaxime or ceftriaxone for the initial treatment of meningitis caused by H. influenzae since the drugs are active against both b-lactamase-producing and non-b-lactamase-producing strains. The incidence of H. influenzae meningitis in the US has decreased considerably since H. influenzae type b conjugate vaccines became available for immunization of infants.
Meningitis Caused by Neisseria meningitidis
Although IV penicillin G generally is considered the drug of choice for the treatment of meningitis caused by N. meningitidis, IV cefotaxime and IV ceftriaxone are acceptable alternatives.
Meningitis Caused by Enterobacteriaceae
Some clinicians recommend that meningitis caused by Enterobacteriaceae (e.g., E. coli, K. pneumoniae) be treated with a third generation cephalosporins (i.e., cefotaxime, ceftazidime, ceftriaxone) with or without an aminoglycoside. Because ceftazidime (but not cefotaxime or ceftriaxone) is effective for the treatment of meningitis caused by Ps. aeruginosa, some clinicians suggest that a regimen of ceftazidime and an aminoglycoside may be preferred for the treatment of meningitis caused by gram-negative bacilli pending results of culture and susceptibility testing.
Brain Abscess and Other CNS Infections
IV cefotaxime has been effective when used in conjunction with metronidazole for empiric treatment of brain abscess in patients 6 months of age or older. Bacterial brain abscesses and other CNS infections (e.g., subdural empyema, intracranial epidural abscesses) often are polymicrobial and can be caused by gram-positive aerobic cocci, Enterobacteriaceae (e.g., E. coli, Haemophilus, Klebsiella), and/or anaerobic bacteria (e.g., Bacteroides, Fusobacterium).
The choice of anti-infectives for empiric therapy of these infections should be based on the predisposing condition and site of primary infection. Some clinicians suggest that the empiric anti-infective regimen in patients who develop the CNS infections after respiratory tract infection (e.g., otitis media, mastoiditis, paranasal sinusitis, pyogenic lung disease) should consist of an appropriate IV third generation cephalosporin (e.g., cefotaxime) given in conjunction with metronidazole, employing the cephalosporin rather than a penicillin to extend coverage to Haemophilus and facultative anaerobic gram-negative bacteria; if presence of staphylococci is suspected, a penicillinase-resistant penicillin (e.g., nafcillin, oxacillin) or vancomycin should be added to the empiric regimen. In patients who develop brain abscess, subdural empyema, or intracranial epidural abscess after trauma or neurosurgery, the empiric regimen should consist of an appropriate IV third generation cephalosporin (e.g., cefotaxime) given in conjunction with a penicillinase-resistant penicillin or vancomycin. Prolonged anti-infective therapy (e.g., 3-6 weeks or longer) usually is required for these CNS infections.
Gonorrhea and Associated Infections
Gonococcal Infections in Adults and Adolescents
Cefotaxime is used for the treatment of uncomplicated cervical, urethral, or rectal gonorrhea caused by penicillinase-producing Neisseria gonorrhoeae (PPNG) or nonpenicillinase-producing strains of the organism.
The US Centers for Disease Control and Prevention (CDC) and most clinicians currently recommend that uncomplicated cervical, urethral, or rectal gonorrhea in adults and adolescents be treated with a single IM dose of ceftriaxone, a single oral dose of cefixime, or a single oral dose of certain fluoroquinolones (ciprofloxacin, ofloxacin, levofloxacin) given in conjunction with an anti-infective regimen effective for presumptive treatment of chlamydia (e.g., a single dose of oral azithromycin or a 7-day regimen of oral doxycycline).
However, fluoroquinolones should not be used for the treatment of gonorrhea acquired in Asia or the pacific islands (including Hawaii) and may be inadvisable for infections acquired in other areas when N. gonorrhoeae with quinolone resistance have been reported (including California). (See Uses: Gonorrhea and Associated Infections, in Ciprofloxacin 8:12.18.)
Alternative regimens that are recommended by the CDC for the treatment of uncomplicated cervical, urethral, or rectal gonorrhea in adults and adolescents include a single IM dose of spectinomycin, a single IM dose of certain cephalosporins (cefotaxime, cefoxitin, ceftizoxime), or a single oral dose of certain fluoroquinolones (gatifloxacin, lomefloxacin, norfloxacin) given in conjunction with an anti-infective regimen effective for presumptive treatment of chlamydia.
Although a single 500-mg IM dose of cefotaxime may be effective in the treatment of uncomplicated gonorrhea, the CDC states that the drug does not appear to offer any advantage over ceftriaxone for the treatment of gonorrhea. IV cefotaxime is recommended by the CDC and AAP as one of several acceptable alternative regimens for the initial treatment of disseminated gonococcal infections in adults and adolescents.
The CDC and AAP currently recommend that treatment of disseminated gonococcal infections in adults and adolescents be initiated with a multiple-dose regimen of IM or IV ceftriaxone. Alternative regimens recommended by the CDC for disseminated gonococcal infections include multiple-dose parenteral regimens of certain IV cephalosporins (cefotaxime, ceftizoxime), certain IV fluoroquinolones (ciprofloxacin, levofloxacin), or IM spectinomycin.
The initial parenteral regimen should be continued for 24-48 hours after improvement begins; therapy can then be switched to oral cefixime, oral ciprofloxacin, oral ofloxacin, or oral levofloxacin and continued to complete at least 1 week of therapy. The CDC recommends that the patient be hospitalized for initial treatment, especially when compliance may be a problem, when the diagnosis is uncertain, or when the patient has purulent synovial effusions or other complications.
Patients should be examined for clinical evidence of endocarditis and meningitis; the recommended regimen for these infections is IV ceftriaxone. Unless the presence of coexisting chlamydial infection has been excluded by appropriate testing, treatment of disseminated gonococcal infections should be administered in conjunction with an anti-infective regimen effective for presumptive treatment of chlamydia.
Gonococcal Infections in Neonates and Infants
Cefotaxime is used for the treatment of N. gonorrhoeae infections in neonates, including disseminated gonococcal infections and gonococcal scalp abscesses and gonococcal ophthalmia neonatorum. Gonococcal infections in neonates usually occur as the result of exposure to the mother’s infected cervical exudate and are apparent 2-5 days after birth. The most serious manifestations of N. gonorrhoeae infection in neonates are ophthalmia neonatorum and sepsis, arthritis, and meningitis; less serious manifestations include rhinitis, vaginitis, urethritis, and inflammation at sites of fetal monitoring (e.g., scalp).
Because a neonate with gonococcal infection usually has acquired the organism from its mother, both the mother and her sexual partner(s) should be evaluated and treated for gonorrhea if indicated. While universal topical prophylaxis using 0.5% erythromycin ophthalmic ointment, silver nitrate 1% topical solution, 1% tetracycline ophthalmic ointment (no longer commercially available in the US) is recommended for all neonates as soon as possible after birth to prevent gonococcal ophthalmia neonatorum, these topical anti-infectives are inadequate for prophylaxis of gonococcal infections at other sites, and may be ineffective in preventing chlamydial ocular infections.
Because neonates born to mothers with untreated gonorrhea are at high risk of infection with N. gonorrhoeae, the CDC and AAP recommend that, in addition to topical prophylaxis, these neonates should receive parenteral prophylaxis against the disease. The CDC and AAP currently recommend that neonates born to mothers with documented peripartum gonococcal infection receive parenteral prophylaxis with a single IM or IV dose of ceftriaxone (25-50 mg/kg not to exceed 125 mg). Alternatively, the AAP states that a single IM or IV dose of cefotaxime (100 mg/kg) can be used for parenteral prophylaxis in these neonates.
For the treatment of ophthalmia neonatorum caused by N. gonorrhoeae, the CDC and AAP recommend that neonates receive a single IM or IV dose of ceftriaxone (25-50 mg/kg not to exceed 125 mg).
Alternatively, the AAP states that a single IM or IV dose of cefotaxime (100 mg/kg) can be used for the treatment of neonatal gonococcal ophthalmia. As an adjunct to parenteral therapy in the treatment of gonococcal ophthalmia neonatorum, the AAP recommends that the neonate’s eyes should be irrigated with sterile sodium chloride solution immediately and at frequent intervals until the discharge is eliminated. Topical anti-infectives used for universaltopical prophylaxis of gonococcal ophthalmia neonatorum are inadequate for the treatment of gonococcal ophthalmia neonatorum and are unnecessary when appropriate parenteral anti-infective therapy is given.
Neonates and infants with a documented gonococcal infection at any site (including the eyes or scalp) should be evaluated for the possibility of disseminated infection (e.g., sepsis, arthritis, meningitis). If gonococcal scalp abscesses or disseminated gonococcal infection is present, the CDC and AAP currently recommend a multidose regimen of IV or IM ceftriaxone or IV or IM cefotaxime; the regimen should be continued for 7 days for the treatment of gonococcal bacteremia, arthritis, or scalp infection or for 10-14 days if meningitis is documented. While either ceftriaxone or cefotaxime can be used for the treatment of disseminated gonococcal infections in neonates, ceftriaxone should be used with caution in neonates who are hyperbilirubinemic (especially those born prematurely) and the AAP suggests that cefotaxime may be preferred in these neonates.
For additional information on current recommendations for the treatment of gonorrhea and associated infections, see Uses: Gonorrhea and Associated Infections, in Ceftriaxone 8:12.06..
Lyme Disease
Cefotaxime is recommended by the Infectious Diseases Society of America (IDSA) and other clinicians as an alternative to ceftriaxone for the treatment of severe forms or late complications of Lyme disease, a spirochetal disease caused by tick-borne Borrelia burgdorferi.
For information on the manifestations of Lyme disease and details about the efficacy of various anti-infective regimens in early or late Lyme disease, see Lyme Disease in Uses: Spirochetal Infections, in the Tetracyclines General Statement 8:12.24. Although oral anti-infectives (e.g., doxycycline, amoxicillin) generally are effective for the treatment of the early stages of Lyme disease (e.g., erythema migrans, isolated facial nerve palsy, mild arthritis or carditis), more serious manifestations associated with early disseminated or late disease (e.g., severe carditis, meningitis, radiculoneuritis) generally require higher dosage, more prolonged therapy, and/or parenteral anti-infectives (e.g., IV ceftriaxone, cefotaxime, or penicillin G). (See Lyme Disease in Uses: Spirochetal Infections, in the Cephalosporins General Statement 8:12.06 and see Lyme Disease in Uses: Spirochetal Infections, in the Natural Penicillins General Statement 8:12..04).
The IDSA states that IV cefotaxime is an effective alternative to ceftriaxone or IV penicillin G in patients requiring parenteral anti-infective therapy for Lyme disease.
While cefotaxime must be administered 3-4 times daily (compared with once-daily administration of ceftriaxone), cefotaxime has not been associated with the biliary complications reported with IV ceftriaxone. Limited data suggest that IV cefotaxime (6 g daily in divided doses for 10 days) is at least as effective as IV penicillin G (20 million units daily for 10 days) in patients with late complications of Lyme disease (e.g., severe radiculitis and/or meningitis, peripheral neuropathy, arthritis).
The IDSA and other clinicians recommend ceftriaxone in patients with early Lyme disease who have acute neurologic disease manifested by meningitis or radiculopathy; alternatively, IV cefotaxime or IV penicillin G may be used. 351, 354, 361 Some clinicians suggest that oral or IV doxycycline for 14-28 days may be adequate therapy in adults with acute neurologic manifestations who are intolerant of cephalosporins and penicillin, although experience in the US with such a regimen for Lyme meningitis is limited. Most clinicians recommend that patients with severe cardiac involvement (e.g., third-degree AV block) be hospitalized for cardiac monitoring and receive IV ceftriaxone or alternatively, IV penicillin G or cefotaxime; however, evidence supporting the superiority of IV versus oral therapy in these patients currently is lacking.
Some clinicians also recommend use of these IV regimens in patients with first-degree AV block and a PR-interval greater than 0.3 seconds. Patients with third-degree AV block may require a temporary pacemaker. While patients with uncomplicated Lyme arthritis generally can be treated with a prolonged course (e.g., 28 days) of oral anti-infectives (e.g., doxycycline or amoxicillin), the IDSA and other clinicians recommend that patients with Lyme arthritis and concomitant neurologic disease documented by CSF analysis should receive IV ceftriaxone; IV cefotaxime or IV penicillin G are recommended as alternative therapy.
Comparative studies evaluating different antibiotic regimens in patients with late Lyme disease generally are lacking. The IDSA and other clinicians recommend 14-28 days of therapy with IV ceftriaxone or a 28-day course of a recommended oral antibiotic in patients who have persistent or recurrent joint swelling after receiving an initial recommended antibiotic regimen.
However, clinicians should consider allowing several months for joint inflammation to resolve after initial treatment before an additional course of antibiotic therapy is given.
Patients with late neurologic disease affecting the CNS or peripheral nervous system (e.g., encephalopathy, neuropathy) should receive 14-28 days of IV ceftriaxone; alternative therapy is IV cefotaxime or IV penicillin G. For additional details on antibiotic therapy in patients with late Lyme disease, see Treatment of Late or Persistent Manifestations of Lyme Disease under Spirochetal Infections: Lyme Disease, in Uses in the Tetracyclines General Statement 8:12..
After receiving recommended antibiotic therapy for Lyme disease, some patients manifest a post-infectious syndrome, which some clinicians have referred to as chronic Lyme disease or post-Lyme disease syndrome. Many patients with positive antibody test results but without classic Lyme disease manifestations (e.g., erythema migrans) reportedly have received empiric IV antibiotic therapy for suspected, late-stage Lyme disease.
However, the IDSA and other clinicians state that currently available evidence is insufficient to consider chronic Lyme disease a separate diagnostic entity and that no controlled clinical studies currently support the efficacy of repeated or prolonged courses or oral and/or IV antibiotics in patients who remain symptomatic after receiving appropriate therapy for Lyme disease (e.g., 2-4 weeks of recommended antibiotic treatment). (See Chronic Lyme Disease or Post-Lyme Disease Syndrome under Spirochetal Infections: Lyme Disease, in Uses in the Tetracyclines General Statement 8:12.24.) In addition, serious complications, including at least one death, have occurred in patients receiving prolonged empiric therapy with IV antibiotics. (See Lyme Disease in Uses: Spirochetal Infections, in Ceftriaxone 8:12.06.12.)
The American College of Rheumatology and IDSA state that the risks and costs of treating suspected Lyme disease empirically with IV antibiotics exceed the benefits in patients with a positive antibody titer for B. burgdorferi and only nonspecific complaints of myalgia or fatigue; such patients are best managed symptomatically rather than with prolonged courses of antibiotics.
Pelvic Inflammatory Disease
Cefotaxime has been used for the treatment of pelvic inflammatory disease (PID), but experience with the drug is limited compared with some other anti-infective agents (e.g., cefoxitin, cefotetan). Because cefotaxime (like other cephalosporins) has no activity against Chlamydia trachomatis, it should be given in conjunction with an anti-infective active against this organism (e.g., doxycycline) whenever it is used in the treatment of PID.
PID is an acute or chronic inflammatory disorder in the upper female genital tract and can include any combination of endometritis, salpingitis, tubo-ovarian abscess, and pelvic peritonitis.
PID generally is a polymicrobial infection most frequently caused by N. gonorrhoeae and/or Chlamydia trachomatis; however, organisms that are part of the normal vaginal flora (e.g., anaerobic bacteria, Gardnerella vaginalis, H. influenzae, enteric gram-negative bacilli, S. agalactiae) or mycoplasma (e.g., Mycoplasma hominis, Ureaplasma urealyticum) also may be involved.
PID is treated with an empiric regimen that provides broad-spectrum coverage. The regimen should be effective against N. gonorrhoeae and C. trachomatis and also probably should be effective against anaerobes, gram-negative facultative bacteria, and streptococci. T
he optimum empiric regimen for the treatment of PID has not been identified. A wide variety of parenteral and oral regimens have been shown to achieve clinical and microbiologic cure in randomized studies with short-term follow-up; however, only limited data are available to date regarding elimination of infection in the endometrium and fallopian tubes or intermediate or long-term outcomes, including the impact of these regimens on the incidence of long-term sequelae of PID (e.g., tubal infertility, ectopic pregnancy, pain).
When a parenteral regimen is indicated for the treatment of PID, the CDC and other clinicians generally recommend a 2-drug regimen of cefotetan (2 g IV every 12 hours) or cefoxitin (2 g IV every 6 hours) given in conjunction with doxycycline (100 mg IV or orally every 12 hours) or a 2-drug regimen of clindamycin (900 mg IV every 8 hours) and gentamicin (usually a 2-mg/kg IV or IM loading dose followed by 1.5 mg/kg every 8 hours).
While there is some evidence that other parenteral cephalosporins (e.g., cefotaxime, ceftizoxime, ceftriaxone) also may be effective for the treatment of PID, the CDC states that there is less experience with use of these cephalosporins in patients with PID and these drugs may be less active than cefotetan or cefoxitin against anaerobic bacteria. Traditionally, parenteral regimens for the treatment of PID have been continued for at least 48 hours after the patient demonstrates substantial clinical improvement and then an oral regimen is continued to complete a total of 14 days of therapy; however, the CDC states that a transition to oral therapy may occur within 24 hours after the patient demonstrates clinical improvement and that decisions regarding such a transition should be guided by clinical experience.
Most clinicians recommend at least 24 hours of direct inpatient observation for patients with tubo-ovarian abscesses after which time anti-infective therapy at home is adequate. When PID is treated with an oral regimen, the CDC recommends a 14-day oral regimen that consists of ofloxacin (400 mg twice daily) or oral levofloxacin (500 mg once daily) with or without oral metronidazole (500 mg twice daily) or a regimen that consists of a single dose of a parenteral cephalosporin (e.g., ceftizoxime, cefotaxime, cefoxitin, ceftriaxone) and a 14-day regimen of oral doxycycline with or without oral metronidazole (500 mg twice daily for 14 days).
The optimal cephalosporin for the second regimen is unclear, although cefoxitin or ceftriaxone usually is preferred. There is limited evidence suggesting that use of oral doxycycline and oral metronidazole after primary parenteral therapy is safe and effective. For additional information on treatment of PID, including information on follow-up and management of sexual partners, see Uses: Pelvic Inflammatory Disease, in the Cephalosporins General Statement 8:12.06.
Respiratory Tract Infections
Community-acquired Pneumonia
Cefotaxime is used for the treatment of community-acquired pneumonia (CAP). The American Thoracic Society (ATS) and Infectious Diseases Society of America (IDSA) suggest that certain parenteral cephalosporins (cefotaxime, ceftriaxone) can be used in inpatient regimens for the treatment of CAP. Initial treatment of CAP generally involves use of an empiric anti-infective regimen based on the most likely pathogens; therapy may then be changed (if possible) to a pathogen-specific regimen based on results of in vitro culture and susceptibility testing, especially in hospitalized patients. T
he most appropriate empiric regimen varies depending on the severity of illness at the time of presentation and whether outpatient treatment or hospitalization in or out of an intensive care unit (ICU) is indicated and the presence or absence of cardiopulmonary disease and other modifying factors that increase the risk of certain pathogens (e.g., penicillin- or multidrug-resistant S. pneumoniae, enteric gram-negative bacilli, Ps. aeruginosa).
Most experts recommend that an empiric regimen for the inpatient treatment of CAP include an anti-infective active against S. pneumoniae since this organism is the most commonly identified cause of bacterial pneumonia and causes more severe disease than many other common CAP pathogens; some other pathogens often involved in inpatient CAP are H. influenzae, enteric gram-negative bacilli, S. aureus, Legionella, Mycoplasma pneumoniae, Chlamydia pneumoniae, and viruses.
Patients with severe CAP admitted into the ICU may have Ps. aeruginosa infections (especially those with underlying bronchiectasis or cystic fibrosis) and Enterobacteriaceae often are involved. In addition, anaerobic infection should be suspected in patients with aspiration pneumonia or lung abscess. Inpatient treatment of CAP is initiated with a parenteral regimen, although therapy may be changed to an oral regimen if the patient is improving clinically, is hemodynamically stable, and able to ingest drugs.
CAP patients usually have a clinical response within 3-5 days after initiation of therapy and failure to respond to the initial empiric regimen generally indicates an incorrect diagnosis, host failure, inappropriate anti-infective regimen (drug selection, dosage, route), unusual pathogen, adverse drug reaction, or complication (e.g., pulmonary superinfection, empyema).
For empiric inpatient treatment of CAP in immunocompetent adults who require hospitalization in a general patient-care setting (not an ICU), the IDSA recommends a 2-drug regimen consisting of a parenteral b-lactam anti-infective (e.g., cefotaxime, ceftriaxone, ampicillin and sulbactam, piperacillin and tazobactam) and a macrolide (e.g., azithromycin, clarithromycin, erythromycin) or monotherapy with a fluoroquinolone active against S. pneumoniae (e.g., gatifloxacin, gemifloxacin, levofloxacin, moxifloxacin).
For empiric inpatient treatment of CAP in immunocompetent adults who are hospitalized in a general patient-care setting and have cardiopulmonary disease (congestive heart failure or chronic obstructive pulmonary disease [COPD]) and/or other modifying factors that increase the risk for multidrug-resistant S. pneumoniae or gram-negative bacteria, the ATS recommends a 2-drug regimen consisting of a parenteral b-lactam anti-infective (cefotaxime, ceftriaxone, ampicillin and sulbactam, high-dose ampicillin) and an oral or IV macrolide (azithromycin or clarithromycin; doxycycline can be used in those with macrolide sensitivity or intolerance) or, alternatively, monotherapy with an IV fluoroquinolone active against S. pneumoniae.
If anaerobes are documented or lung abscess is present, clindamycin or metronidazole should be added to the regimen. For CAP patients admitted to a general patient-care setting who do not have cardiopulmonary disease or other modifying factors, the ATS suggests an empiric regimen of monotherapy with IV azithromycin; for those with macrolide sensitivity or intolerance, a 2-drug regimen of doxycycline and a b-lactam or monotherapy with a fluoroquinolone active against S. pneumoniae can be used.
For inpatient treatment of CAP in immunocompetent adults who require hospitalization in an ICU, the IDSA recommends an empiric 2-drug regimen consisting of a b-lactam anti-infective (cefotaxime, ceftriaxone, ampicillin and sulbactam, piperacillin and tazobactam) and either a macrolide or a fluoroquinolone.
For inpatient treatment of severe CAP in patients hospitalized in an ICU, the ATS recommends that those not at risk for Ps. aeruginosa infection receive a 2-drug empiric regimen consisting of an IV b-lactam anti-infective (cefotaxime, ceftriaxone) and either an IV macrolide (azithromycin) or IV fluoroquinolone. If risk factors for Ps. aeruginosa are present in patients with severe CAP admitted to an ICU, the ATS recommends an empiric regimen that includes 2 antipseudomonal agents and provides coverage for multidrug-resistant S. pneumonia and Legionella. Therefore, the ATS recommends that these patients receive a 2-drug empiric regimen that includes an IV antipseudomonal b-lactam anti-infective (e.g., cefepime, piperacillin and tazobactam, imipenem, meropenem) and an IV antipseudomonal fluoroquinolone (e.g., ciprofloxacin) or, alternatively, a 3-drug empiric regimen that includes one of the IV antipseudomonal β-lactams, an IV aminoglycoside, and either an IV macrolide (e.g., azithromycin) or an IV nonpseudomonal quinolone.
Septicemia
Cefotaxime is used for the treatment of bacteremia/septicemia caused by E. coli, Klebsiella, S. marcescens, S. aureus, and streptococci (including S. pneumoniae). The choice of anti-infective agent for the treatment of sepsis syndrome should be based on the probable source of infection, gram-stained smears of appropriate clinical specimens, the immune status of the patient, and current patterns of bacterial resistance within the hospital and local community.
Certain parenteral cephalosporins (i.e., cefepime, cefotaxime, ceftizoxime, ceftazidime, ceftriaxone) are good choices for the treatment of gram-negative sepsis. Ceftazidime is less active against gram-positive cocci, and most cephalosporins (except cefepime and ceftazidime) have limited activity against Ps. aeruginosa.
For the initial treatment of life-threatening sepsis in adults (unless presence of anaerobic bacteria, oxacillin-resistant staphylococci [ORSA; previously known as methicillin-resistant staphylococci, MRSA], or bacterial endocarditis is suspected), some clinicians suggest the use of a parenteral cephalosporin (i.e., cefepime, cefotaxime, ceftriaxone) given in conjunction with an aminoglycoside (amikacin, gentamicin, tobramycin) is one of several preferred regimens.
Some clinicians recommend use of vancomycin (alone or in conjunction with gentamicin and/or rifampin) when oxacillin-resistant staphylococci are a possible cause of sepsis; when bacterial endocarditis is suspected and therapy must be initiated before results of in vitro testing are available to identify the pathogen, a regimen of vancomycin and gentamicin can be used.
Typhoid Fever and Other Salmonella Infections
Typhoid Fever
Cefotaxime has been used in adults or children for the treatment of typhoid fever (enteric fever) or septicemia caused by Salmonella typhi or S. paratyphi, including multidrug-resistant strains.
Multidrug-resistant strains of S. typhi (i.e., strains resistant to ampicillin, chloramphenicol, and/or co-trimoxazole) have been reported with increasing frequency, and third generation cephalosporins (e.g., cefotaxime, ceftriaxone) and fluoroquinolones (e.g., ciprofloxacin, ofloxacin) are considered the agents of first choice for the treatment of typhoid fever or other severe infections known or suspected to be caused by these strains.
Cefotaxime also has been used in the treatment of infections caused by nontyphi Salmonella, including bacteremia, osteomyelitis, and meningitis caused by S. typhimurium.
Salmonella Gastroenteritis
Anti-infective therapy generally is not indicated in otherwise healthy individuals with uncomplicated (noninvasive) gastroenteritis caused by non-typhi Salmonella (e.g., S. enteritidis, S. typhimurium) since such therapy may prolong the duration of fecal excretion of the organism and there is no evidence that it shortens the duration of the disease; however, the CDC, AAP, IDSA, and others recommend anti-infective therapy in individuals with severe Salmonella gastroenteritis and in those who are at increased risk of invasive disease.
These individuals at increased risk include infants younger than 3-6 months of age; individuals older than 50 years of age; individuals with hemoglobinopathies, severe atherosclerosis or valvular heart disease, prostheses, uremia, chronic GI disease, or severe colitis; and individuals who are immunocompromised because of malignancy, immunosuppressive therapy, HIV infection, or other immunosuppressive illness.
When an anti-infective agent is considered necessary in an individual with Salmonella gastroenteritis, the CDC, AAP, IDSA, and others recommend use of ceftriaxone, cefotaxime, a fluoroquinolone (should be used in children only if the benefits outweigh the risks and no alternative exists), ampicillin, amoxicillin, co-trimoxazole, or chloramphenicol, depending on the susceptibility of the causative organism.
HIV-Infected Individuals
While no controlled study has demonstrated a beneficial effect of such treatment and there is evidence from some studies in immunocompetent individuals that anti-infective agent therapy may prolong the duration of fecal excretion of the organism, the Prevention of Opportunistic Infections Working Group of the US Public Health Service and the Infectious Disease Society of America (USPHS/IDSA) suggest that HIV-infected adults, severely immunosuppressed HIV-infected children, and HIV-exposed infants younger than 3 months of age who have Salmonella gastroenteritis receive anti-infective therapy to prevent extraintestinal spread of the infection.
The USPHS/IDSA recommends that HIV-infected adults receive ciprofloxacin; however, pregnant HIV-infected women with Salmonella gastroenteritis should receive ampicillin, cefotaxime, ceftriaxone, or co-trimoxazole. The USPHS/IDSA recommends that HIV-infected children receive co-trimoxazole, ampicillin, cefotaxime, ceftriaxone, or chloramphenicol for prevention of extraintestinal spread of the infection; fluoroquinolones should be used in children with caution and only if no alternative exists. In HIV-infected individuals who have been treated for bacteremia caused by Salmonella, the USPHS/IDSA recommends use of long-term suppressive or maintenance anti-infective therapy (secondary prophylaxis) to prevent recurrence or relapse.
The choice of anti-infective agent for such prophylaxis should be based on results of in vitro susceptibility testing of the causative organism. The USPHS/IDSA suggests use of a fluoroquinolone (usually ciprofloxacin) in HIV-infected adults and co-trimoxazole or, alternatively, ampicillin, or chloramphenicol for HIV-infected children. In addition, the USPHS/IDSA recommends that household contacts of HIV-infected individuals treated for salmonellosis be evaluated for asymptomatic carriage ofSalmonella so that strict hygienic measures and/or anti-infective prophylaxis can be instituted to prevent recurrent transmission to the HIV-infected individual.
Capnocytophaga Infections
Based on results of in vitro susceptibility tests that indicate that Capnocytophaga generally are inhibited by cefotaxime, some clinicians suggest that cefotaxime can be used in the treatment of infections caused by Capnocytophage. Capnocytophaga is a gram-negative bacilli that can cause life-threatening septicemia, meningitis, and/or endocarditis and often is associated with disseminated intravascular coagulation; splenectomized and immunocompromised individuals are at particularly high risk for serious infections caused by the organism. C. canimorsus infection usually occurs as the result of a dog bite. The optimum regimen for the treatment of infections caused by Capnocytophaga has not been identified but some clinicians recommend use of penicillin G or, alternatively, a third generation cephalosporin (cefotaxime, ceftizoxime, ceftriaxone), a carbapenem (imipenem, meropenem), vancomycin, a fluoroquinolone, or clindamycin.
Vibrio Infections
Vibrio parahaemolyticus Infections
Cefotaxime is one of several alternatives recommended for the treatment of severe cases of Vibrio parahaemolyticus infection when anti-infective therapy is indicated in addition to supportive care. V. parahaemolyticus infection is a relatively rare foodborne illness that can occur as the result of ingestion of undercooked or raw fish or shellfish; the incubation period usually is 2-48 hours. The signs and symptoms of V. parahaemolyticus infection are watery diarrhea, abdominal cramps, and nausea and vomiting lasting 2-5 days. Although supportive care usually is sufficient, some clinicians recommend use of tetracycline, doxycycline, gentamicin, or cefotaxime in severe cases.
Vibrio vulnificus Infections
Some clinicians suggest that cefotaxime is a drug of choice for the treatment of infections caused by V. vulnificus. V. vulnificus can cause potentially fatal septicemia, wound infections, or gastroenteritis and generally is transmitted through ingestion of contaminated raw or undercooked seafood (especially raw oysters) or through contamination of a wound with seawater or seafood drippings.
V. vulnificus is naturally present in marine environments, thrives in warm ocean water, and frequently is isolated from oysters and other shellfish harvested from the Gulf of Mexico and from US coastal waters along the Pacific and Atlantic ocean. Individuals with preexisting liver disease are at high risk for developing fatal septicemia following ingestion of seafood contaminated with V. vulnificus and debilitated or immunocompromised individuals (e.g., those with chronic renal impairment, cancer, diabetes mellitus, steroid-dependent asthma, chronic GI disease) or individuals with iron overload states (e.g., thalassemia, hemochromatosis) also are at increased risk for fatal infections.
The incubation period for V. vulnificus infection reportedly is 1-7 days and the duration of illness usually is 2-8 days. In immunocompromised individuals, fever, nausea, myalgia, and abdominal cramps may occur as soon as 24-48 hours after ingestion of seafood contaminated with V. vulnificus and sepsis and cutaneous bullae may be present within 36 hours of the onset of symptoms.
Because the case fatality rate for V. vulnificus septicemia exceeds 50% in immunocompromised individuals and those with preexisting liver disease, these individuals should be informed about the health hazards of ingesting raw or undercooked seafood (especially oysters), the need to avoid contact with seawater during the warm months, and the importance of using protective clothing (e.g., gloves) when handling shellfish. V. vulnificus infection should be considered in the differential diagnosis of fever of unknown etiology, and individuals who present with fever (especially when bullae, cellulitis, or wound infection is present) and who have preexisting liver disease or are immunocompromised should be questioned regarding a history of raw oyster ingestion or seawater contact. While optimum anti-infective therapy for the treatment of V. vulnificus infections has not been identified, use of a tetracycline or third generation cephalosporin (e.g., cefotaxime, ceftazidime) is recommended. Because of the high fatality rate associated with V. vulnificus infections, anti-infective therapy should be initiated promptly if indicated.
Yersinia Infections
Although GI infections caused by Yersinia enterocolitica or Y. pseudotuberculosis usually are self-limited and anti-infective therapy unnecessary, the AAP, IDSA, and others recommend use of anti-infectives in immunocompromised individuals or for the treatment of severe infections or when septicemia or other invasive disease occurs. GI infections caused by Y. enterocolitica or Y. pseudotuberculosis can occur as the result of ingesting undercooked pork, unpasteurized milk, or contaminated water; infection has occurred in infants whose caregivers handled contaminated chitterlings (raw pork intestines) or tofu. Use of co-trimoxazole, an aminoglycoside (e.g., amikacin, gentamicin, tobramycin), a fluoroquinolone (e.g., ciprofloxacin), doxycycline, cefotaxime, or ceftizoxime has been recommended when treatment is considered necessary; combination therapy may be necessary. Some clinicians suggest that, while cefotaxime may be effective in the treatment of Y. enterocolitica bacteremia, the role of anti-infectives, including oral anti-infectives, in the management of enterocolitis, pseudoappendicitis syndrome, or mesenteric adenitis caused by Yersinia needs further evaluation.
Perioperative Prophylaxis
Cefotaxime has been used perioperatively to reduce the incidence of infection in patients undergoing contaminated or potentially contaminated surgery (e.g., GI and genitourinary surgery, abdominal or vaginal hysterectomy) and in patients undergoing cesarean section. However, other anti-infectives (e.g., cefazolin, cefotetan, cefoxitin) usually are the preferred drugs for perioperative prophylaxis. Some clinicians state that third generation cephalosporins (e.g., cefoperazone, cefotaxime, ceftazidime, ceftizoxime, ceftriaxone) and fourth generation cephalosporins (e.g., cefepime) should not be used for perioperative prophylaxis since they are expensive, some are less active than cefazolin against staphylococci, they have a spectrum of activity that is wider than necessary for organisms encountered in elective surgery, and their use for prophylaxis promotes emergence of resistant organisms. (See Uses: Perioperative Prophylaxis in the Cephalosporins General Statement 8:12.06.)
Dosage and Administration
Reconstitution and Administration
Cefotaxime sodium is administered IV or by deep IM injection. The drug should be given IV rather than IM in patients with septicemia, bacteremia, peritonitis, meningitis, or other severe or life-threatening infections or in patients with lowered resistance resulting from debilitating conditions (e.g., malnutrition, trauma, surgery, diabetes, heart failure, malignancy), particularly if shock is present.
Intermittent IV Injection
For direct intermittent IV administration, 10 mL of sterile water for injection should be added to a vial labeled as containing 500 mg, 1 g, or 2 g of cefotaxime to provide a solution containing approximately 50, 95, or 180 mg of cefotaxime per mL, respectively. A solution of 1 g of cefotaxime per 14 mL of sterile water for injection is isotonic. The appropriate dose may then be injected directly into a vein over a 3- to 5-minute period or slowly into the tubing of a freely flowing compatible IV solution. Cefotaxime should not be injected IV over less than 3 minutes since rapid (over less than 1 minute) injection was consistently associated with potentially life-threatening arrhythmias during postmarketing surveillance.
Intermittent or Continuous IV Infusion
For intermittent or continuous IV infusion, 50 or 100 mL of 0.9% sodium chloride injection or 5% dextrose injection should be added to an infusion bottle labeled as containing 1 or 2 g of cefotaxime or, alternatively, reconstituted solutions of cefotaxime may be further diluted with 50 mL to 1 L of a compatible IV solution. ADD-Vantage® vials or infusion bottles labeled as containing 1 or 2 g of cefotaxime or the 10-g pharmacy bulk package of cefotaxime should be reconstituted according to the manufacturer’s directions.
The cefotaxime bulk package is not intended for direct IV infusion; doses of the drug from the reconstituted bulk package must be further diluted in a compatible IV infusion solution prior to administration.
Thawed solutions of the commercially available frozen cefotaxime sodium injection should be administered only by intermittent or continuous IV infusion. The commercially available frozen cefotaxime sodium in dextrose injections should not be thawed by warming them in a water bath or by exposure to microwave radiation. A precipitate may form while the commercially available injection in dextrose is frozen; however, this usually will dissolve with little or no agitation upon reaching room temperature, and the potency of ceftazidime sodium frozen injection is not affected.
After thawing at room temperature or under refrigeration at 5°C, the container should be checked for minute leaks by firmly squeezing the bag. The injection should be discarded if the container seal or outlet ports are not intact or leaks are found or if the solution is cloudy or contains a precipitate. Additives should not be introduced into the injection container. The injection should not be used in series connections with other plastic containers, since such use could result in air embolism from residual air being drawn from the primary container before administration of fluid from the secondary container is complete. Intermittent IV infusions of cefotaxime are generally infused over 20-30 minutes; solutions should preferably be infused via butterfly or scalp vein-type needles.
Other IV solutions flowing through a common administration tubing or site should be discontinued while cefotaxime is being infused unless the solutions are known to be compatible and the flow-rate is adequately controlled.
IM Injection
IM injections of cefotaxime are prepared by adding 2, 3, or 5 mL of sterile or bacteriostatic water for injection to a vial labeled as containing 500 mg, 1 g, or 2 g of the drug. Resultant solutions contain approximately 230, 300, or 330 mg of cefotaxime per mL, respectively. IM injections should be made deeply into a large muscle mass such as the upper outer quadrant of the gluteus maximus; aspiration should be performed to avoid inadvertent injection into a blood vessel. The manufacturer states that if an IM dose of 2 g of cefotaxime is indicated, the dose should be divided and administered at 2 different injection sites. However, because large IM doses of cefotaxime may be painful, some clinicians recommend that large doses of the drug be given IV.
Dosage
Dosage of cefotaxime sodium is expressed in terms of cefotaxime and is identical for IM or IV administration.
Adult Dosage
The usual adult dosage of cefotaxime for the treatment of uncomplicated infections is 1 g IM or IV every 12 hours. Moderate to severe infections usually respond to 1-2 g IM or IV every 8 hours, but some infections (e.g., septicemia) should be treated with 2 g IV every 6-8 hours. Severe or life-threatening infections may require 2 g IV every 4 hours. The maximum adult dosage recommended by the manufacturer is 12 g daily.
Meningitis and Other CNS Infections For the treatment of meningitis or other CNS infections caused by susceptible bacteria, the usual adult dosage of cefotaxime is 2 g IV every 6 hours for 7-21 days. Some clinicians recommend that patients with meningitis known or suspected to be caused by S. pneumoniae receive an initial cefotaxime dosage of 350 mg/kg daily given in 4 divided doses; if results of in vitro susceptibility testing indicate that the organism is susceptible to penicillin, dosage can be reduced to 225 mg/kg daily given in 3 divided doses.
While 7 days of cefotaxime therapy may be adequate for the treatment of uncomplicated meningitis caused by susceptible Haemophilus influenzae or Neisseria meningitidis, at least 10-14 days of therapy is recommended for complicated cases or meningitis caused by Streptococcus pneumoniae and at least 21 days of therapy is recommended for meningitis caused by susceptible Enterobacteriaceae (e.g., Escherichia coli, Klebsiella).
Gonorrhea and Associated Infections
For the treatment of uncomplicated urethral, cervical, or rectal gonorrhea caused by penicillinase-producing strains of N. gonorrhoeae (PPNG) or nonpenicillinase-producing strains of the organism, adults and adolescents should receive a single 500-mg IM dose of cefotaxime; however, the manufacturer recommends a single 1-g IM dose for the treatment of rectal gonorrhea in males.
For the treatment of disseminated gonorrhea, adults and adolescents should receive 1 g of cefotaxime IV every 8 hours. The CDC states that adults and adolescents should receive cefotaxime for 24-48 hours after improvement begins; therapy can then be switched to oral cefixime or certain oral fluoroquinolones (ciprofloxacin, ofloxacin, oral levofloxacin) to complete at least 1 week of therapy.
Unless the presence of coexisting chlamydial infection has been excluded by appropriate testing, cefotaxime therapy for uncomplicated or disseminated gonococcal infections should be administered in conjunction with an anti-infective regimen effective for presumptive treatment of chlamydia (e.g., a single dose of oral azithromycin or a 7-day regimen of oral doxycycline).
Lyme Disease
For the treatment of serious neurologic, cardiac, and/or arthritic manifestations of early disseminated or late Lyme disease in adults, many clinicians recommend a cefotaxime dosage of 2 g IV every 8 hours for 14-28 days. Additional courses of antibiotic therapy generally are not recommended unless relapse of neurologic disease is documented with reliable objective measures.
Respiratory Tract Infections
For the treatment of community-acquired pneumoniae (CAP) in adults who are hospitalized for inpatient treatment, cefotaxime usually is given in a dosage of 1 g every 6-8 hours in conjunction with other anti-infectives. (See Community-acquired Pneumonia under Uses: Respiratory Tract Infections.) The duration of CAP therapy depends on the causative pathogen, illness severity at the onset of anti-infective therapy, response to treatment, comorbid illness, and complications. CAP secondary to S. pneumoniae generally can be treated for 7-10 days or 72 hours after the patient becomes afebrile. CAP caused by bacteria that can necrose pulmonary parenchyma generally should be treated for at least 2 weeks.
Patients chronically treated with corticosteroids also may require at least 2 weeks of therapy.
Perioperative Prophylaxis
Although not considered a drug of choice for perioperative prophylaxis (see Uses: Perioperative Prophylaxis), cefotaxime should usually be given 30-90 minutes prior to surgery to ensure adequate cefotaxime tissue concentrations at the time of surgery.
Continuation of the drug for more than 24 hours after surgery appears to be of no additional value and may increase the risk of toxicity and bacterial superinfection. If signs of infection occur following surgery, specimens should be obtained for identification of the causative organism and appropriate therapy instituted. If cefotaxime is used for perioperative prophylaxis in contaminated or potentially contaminated surgery, the manufacturer recommends that adults receive 1 g IM or IV 30-90 minutes prior to surgery.
For patients undergoing GI surgery, the manufacturer recommends preoperative bowel preparation using mechanical cleansing and a nonabsorbable anti-infective (e.g., neomycin) in addition to prophylactic administration of cefotaxime.
If cefotaxime is used prophylactically in patients undergoing cesarean section, the manufacturer recommends 1 g given IV as soon as the umbilical cord is clamped, followed by 1 g IM or IV 6 and 12 hours after the first dose. Pediatric Dosage The usual dosage of cefotaxime recommended by the manufacturer for premature or full-term neonates less than 1 week of age is 50 mg/kg every 12 hours and the usual dosage for neonates 1-4 weeks of age is 50 mg/kg every 8 hours.
Alternatively, for neonates younger than 1 week of age, the American Academy of Pediatrics (AAP) recommends a cefotaxime dosage of 50 mg/kg every 12 hours for those who weigh 2 kg or less and 50 mg/kg every 8 or 12 hours for those who weigh more than 2 kg. For neonates 1-4 week of age, the AAP recommends a dosage of 50 mg/kg every 8 hours for those who weigh 2 kg or less and 50 mg/kg every 6 or 8 hours for those who weigh more than 2 kg.
The manufacturer recommends that children 1 month to 12 years of age weighing less than 50 kg receive 50-180 mg/kg daily given in 4-6 equally divided doses; the higher dosages should be used for more severe or serious infections, including meningitis. The AAP recommends that children older than 1 month of age receive a cefotaxime dosage of 75-100 mg/kg daily given in 3 or 4 equally divided doses for the treatment of mild to moderate infections and a dosage of 150-200 mg/kg daily given in 3 or 4 equally divided doses for the treatment of severe infections.
The AAP also states that a dosage of 300 mg/kg daily given in 3 or 4 divided doses can be used for the treatment of meningitis in this age group. Children weighing 50 kg or more should receive the usual daily adult dosage, but dosage should not exceed 12 g daily.
Meningitis and Other CNS Infections
For the treatment of meningitis caused by susceptible bacteria, the manufacturer recommends that children 1 month to 12 years of age who weigh less than 50 kg receive a cefotaxime dosage at the high end of the range of 50-180 mg/kg daily.
Some clinicians recommend that infants and children younger than 18 years of age with meningitis receive cefotaxime in a dosage of 50 mg/kg IV every 6 hours. The AAP states that a cefotaxime dosage of 75 mg/kg 3 times daily has been effective for the treatment of meningitis in infants and children 1 month of age or older; however, if meningitis is known or suspected to be caused by S. pneumoniae, these children should receive cefotaxime in a dosage of 225-300 mg/kg daily given IV in divided doses ever 6-8 hours.
While 7 days of therapy may be adequate for the treatment of uncomplicated meningitis caused by susceptible H. influenzae or N. meningitidis, at least 10-14 days of therapy is recommended for complicated cases or for meningitis caused by S. pneumoniae and at least 21 days is recommended for meningitis caused by susceptible Enterobacteriaceae (e.g., E. coli, Klebsiella).
Gonorrhea and Associated Infections
The usual dosage of cefotaxime for the treatment of disseminated gonococcal infection (e.g., sepsis, arthritis, meningitis) or gonococcal scalp abscesses in neonates is 25-50 mg/kg IV or IM every 12 hours for 7 days; if meningitis is documented, the drug should be continued for 10-14 days. If cefotaxime is used as an alternative to ceftriaxone for parenteral prophylaxis in neonates at increased risk for gonococcal infection, the AAP recommends that a single 100-mg/kg dose be given IV or IM at birth. If cefotaxime is used as an alternative to ceftriaxone for the treatment of gonococcal ophthalmia neonatorum, the AAP recommends that neonates receive a single 100-mg/kg IV or IM dose. Although a single dose is adequate therapy for gonococcal conjunctivitis, some clinicians prefer to continue parenteral anti-infective therapy until ocular cultures are negative at 48-72 hours.
As an adjunct to parenteral therapy in the treatment of gonococcal ophthalmia neonatorum, the neonate’s eyes should be irrigated with sterile sodium chloride solution immediately and at frequent intervals until the discharge is eliminated.
Lyme Disease
For the treatment of serious neurologic, cardiac, and/or arthritic manifestations of early disseminated or late Lyme disease in children, many clinicians recommend a cefotaxime dosage of 150 mg/kg (maximum daily dosage: 6 g) IV every 6-8 hours for 14-28 days. Additional courses of antibiotic therapy generally are not recommended unless relapse of neurologic disease is documented with reliable objective measures.
Duration of Therapy
The duration of cefotaxime therapy depends on the type of infection but should generally be continued for at least 48-72 hours after the patient becomes afebrile or evidence of eradication of the infection is obtained.
Although other drugs generally are preferred, if cefotaxime is used in infections caused by group A b-hemolytic streptococci, therapy should be continued for at least 10 days to decrease the risk of rheumatic fever or glomerulonephritis.
Chronic urinary tract infections may require several weeks of therapy, and bacteriologic and clinical assessments should be made frequently during therapy and for several months after therapy is discontinued.
Dosage in Renal and Hepatic Impairment
Modification of the usual dosage of cefotaxime is unnecessary in patients with creatinine clearances of 20 mL/minute or greater per 1.73 m. However, in patients with creatinine clearances less than 20 mL/minute per 1.73 m, doses and/or frequency of administration should be modified in response to the degree of renal impairment. The manufacturer recommends that these patients receive half the usual dose of cefotaxime at the usual time interval.
In patients undergoing hemodialysis, some clinicians recommend that 0.5-2 g be given as single daily doses and that a supplemental dose of cefotaxime be given after each dialysis period.
Although serum half-life and clearance of cefotaxime and its major metabolite may be prolonged in patients with impaired hepatic function, dosage adjustments are not necessary in such patients unless renal function also is impaired.
Cautions
Dermatologic and Sensitivity Reactions
Hypersensitivity reactions have been reported to occur in approximately 2% of patients receiving cefotaxime. These reactions include rash (maculopapular or erythematous), pruritus, fever, and eosinophilia. Urticaria, anaphylaxis, erythema multiforme, Stevens-Johnson syndrome, and toxic epidermal necrolysis have occurred rarely. If a severe hypersensitivity reaction occurs during cefotaxime therapy, the drug should be discontinued and the patient given appropriate therapy (e.g., epinephrine, corticosteroids, maintenance of an adequate airway, oxygen) as indicated.
Positive direct antiglobulin (Coombs’) test results have also been reported occasionally in patients receiving cefotaxime; however, it is not clear whether the mechanism of this reaction is immunologic in nature.
Local Effects
The manufacturer states that the most frequent adverse reactions to cefotaxime are local reactions at the injection site which occur in approximately 4% of patients. IV administration has caused inflammation, phlebitis, and thrombophlebitis and IM administration has caused pain, induration, and tenderness at the injection site. Extensive perivascular extravasation of cefotaxime may result in tissue damage requiring surgical intervention; however, in most cases, perivascular extravasation responds to changing the infusion site. To minimize the potential for tissue inflammation, the manufacturer recommends that IV infusion sites be monitored regularly and changed appropriately.
GI Effects
Adverse GI effects including anorexia, diarrhea, nausea, vomiting, abdominal pain, and colitis have occurred in approximately 1% of patients receiving cefotaxime. Clostridium difficile-associated diarrhea and colitis (also known as antibiotic-associated pseudomembranous colitis), caused by toxin-producing clostridia resistant to cefotaxime, also has been reported rarely.
Mild cases of C. difficile-associated diarrhea and colitis may respond to discontinuance of cefotaxime alone, but diagnosis and management of moderate to severe cases should include sigmoidoscopy (or other appropriate endoscopic examination), appropriate bacteriologic studies, and treatment with fluid, electrolyte, and protein supplementation as indicated. If diarrhea and colitis is moderate to severe or is not relieved by discontinuance of cefotaxime alone, appropriate anti-infective therapy (e.g., oral metronidazole or vancomycin) should be administered. Other causes of colitis also should be considered.
Hematologic Effects
Transient neutropenia, granulocytopenia, leukopenia, eosinophilia, or thrombocytopenia have occurred in less than 1% of patients receiving cefotaxime. Agranulocytosis reportedly may occur rarely with cefotaxime treatment, particularly during prolonged therapy; therefore, blood cell counts should be performed in patients receiving treatment courses lasting for more than 10 days. Hemolytic anemia has also been reported rarely. Prolongation of the prothrombin time and hypoprothrombinemia have been reported only rarely in patients receiving cefotaxime.
Renal Effects
Transient increases in BUN and/or serum creatinine concentrations and interstitial nephritis have been reported in a few patients receiving cefotaxime. A transient increase in urinary concentration of alanine aminopeptidase, which may be an indication of transient tubular damage, has been reported in a few patients receiving the drug. Most studies indicate that cefotaxime is not nephrotoxic and that urine concentrations of alanine aminopeptidase are usually unchanged during therapy with the drug.
Other Adverse Effects
Transient increases in serum AST (SGOT), ALT (SGPT), LDH, bilirubin, and alkaline phosphatase concentrations have been reported in less than 1% of patients receiving cefotaxime. Headache, agitation, confusion, fatigue, and nocturnal perspiration have also been reported in less than 1% of patients receiving the drug. Seizures have been reported with some cephalosporins, During postmarketing surveillance, potentially life-threatening arrhythmias were reported in several patients who received cefotaxime by rapid (less than 1 minute) bolus injection through a central venous catheter.
Precautions and Contraindications
Prior to initiation of cefotaxime therapy, careful inquiry should be made concerning previous hypersensitivity reactions to cefotaxime, cephalosporins, penicillins, or other drugs. There is clinical and laboratory evidence of partial cross-allergenicity among cephalosporins and other b-lactam antibiotics including penicillins and cephamycins; however, the true incidence of cross-allergenicity among these anti-infectives has not been established.
Cefotaxime is contraindicated in patients with a history of allergic reactions to the drug or other cephalosporins and should be used with caution in patients with a history of hypersensitivity to penicillins.
Use of cephalosporins should be avoided in patients who have had an immediate-type (anaphylactic) hypersensitivity reaction to penicillins. Although it has not been definitely proven that allergic reactions to antibiotics are more frequent in atopic individuals, the manufacturer states that cefotaxime should be used with caution in patients with a history of allergy, particularly to drugs.
Prolonged use of cefotaxime may result in overgrowth of nonsusceptible organisms, especially Candida and Pseudomonas. Vaginitis and moniliasis have occurred in less than 1% of patients receiving cefotaxime.
Resistant strains of some organisms, especially Enterobacter, Ps. aeruginosa, and Serratia, have developed during therapy with cefotaxime. Careful observation of the patient during cefotaxime therapy is essential. If suprainfection or superinfection occurs, appropriate therapy should be instituted. Cefotaxime should be used with caution in patients with a history of GI disease, particularly colitis.
Because C. difficile-associated diarrhea and colitis has been reported with the use of cefotaxime or other cephalosporins, it should be considered in the differential diagnosis of patients who develop diarrhea during cefotaxime therapy. Seizures have been reported with several cephalosporins, particularly in patients with renal impairment in whom dosage of the drug was not reduced. If seizures occur during cephalosporin therapy, the drug should be discontinued and anticonvulsant therapy initiated as clinically indicated.
Pediatric Precautions
Cefotaxime is well tolerated in pediatric patients, and adverse effects reported in children receiving the drug are similar to those reported in adults. A retrospective review of children 3 months to 18 years of age who received cefotaxime indicates that adverse effects occurred in up to 2.5% of these children and included adverse local reactions, rash, and adverse GI effects such as diarrhea and vomiting. Safety of the chemical components that may leach out of the plastic containing commercially available frozen cefotaxime sodium injections has not been established in children.
Mutagenicity and Carcinogenicity
Cefotaxime was not mutagenic in the mouse micronucleous test or the Ames test. Studies have not been performed to date to evaluate the carcinogenic potential of cefotaxime.
Pregnancy, Fertitlity and Lactation
Reproduction studies in mice or rats using IV cefotaxime dosages up to 1.2 g/kg daily (0.4 or 0.8 times, respectively, the usual human dosage based on mg/m2) have not revealed evidence of embryotoxicity or teratogenicity.
However, the offspring of rats that received 1.2 g/kg of cefotaxime weighed less at birth and also remained smaller during 21 days of nursing than offspring of rats that did not receive the drug.
There are no adequate and controlled studies to date using cefotaxime in pregnant women, and the drug should be used during pregnancy only when clearly needed. There was no evidence of impaired fertility in rats given cefotaxime subcutaneously at dosages up to 250 mg/kg daily or in mice given the drug IV at dosages up to 2 g/kg daily (0.2 or 0.7 times, respectively, the recommended human dosage based on mg/m2).
Because cefotaxime is distributed into milk, the drug should be used with caution in nursing women.
Drug Interactions
Aminoglycosides
In vitro studies indicate that the antibacterial activity of cefotaxime and aminoglycosides may be additive or synergistic against some organisms including some strains of Ps. aeruginosa and S. marcescens. However, synergism is unpredictable and antagonism has also occurred in vitro when cefotaxime was used in combination with an aminoglycoside. Concurrent use of aminoglycosides and cephalosporins may increase the risk of nephrotoxicity during therapy.
Although this effect has not been reported to date with cefotaxime, the manufacturer states that the possibility that nephrotoxicity may be potentiated if the drug is used concomitantly with an aminoglycoside should be considered.
Other Anti-infective Agents
In one in vitro study which used the checkerboard technique to assess synergism, a combination of cefotaxime and ampicillin appeared to be partially additive or synergistic against a few strains of group B streptococci. However, when the killing-curve technique was used to assess synergism, the combination was no more effective than cefotaxime alone against these organisms. In one in vitro study, a combination of cefotaxime and clindamycin was neither synergistic nor antagonistic against Enterobacteriaceae.
Laboratory Test Interferences
Immunohematology Tests
Positive direct antiglobulin (Coombs’) test results have been reported in a few patients receiving cefotaxime. This reaction may interfere with hematologic studies or transfusion cross-matching procedures.
Tests for Glucose and Creatinine
Although other currently available cephalosporins reportedly cause false-positive results in urine glucose determinations using cupric sulfate solution (Benedict’s reagent, Clinitest®) and may cause falsely elevated serum or urine creatinine values when the Jaffe reaction is used, cefotaxime does not appear to interfere with these laboratory tests.
Acute Toxcicity
In neonatal and adult mice and rats, acute overdosage of cefotaxime resulted in significant mortality at parenteral dosages exceeding 6 g/kg daily. Common toxic signs in those that died included a decrease in spontaneous activity, tonic and clonic convulsions, dyspnea, hypothermia, and cyanosis. Acute overdosage of cefotaxime in patients has most frequently resulted in increased serum concentrations of BUN and creatinine, but most cases were not associated with overt toxicity. If acute overdosage occurs, the patient should be closely observed and given supportive treatment.
Mechanism of Action
Cefotaxime has a mechanism of action similar to that of other cephalosporins. For information on the mechanism of action of cephalosporins, see Mechanism of Action in the Cephalosporins General Statement 8:12.06. The target enzymes of b-lactam antibiotics have been classified as penicillin-binding proteins (PBPs) and appear to vary substantially among bacterial species. Studies evaluating the binding of cefotaxime to PBPs indicate that the drug has a high affinity for PBPs 1a, 1b, and 3 of Escherichia coli and PBPs 1a, 1b, 3, and 4 of Pseudomonas aeruginosa.
The affinities of various b-lactam antibiotics for different PBPs appear to explain the differences in morphology which occur in susceptible organisms following exposure to different b-lactam antibiotics and may also explain differences in the spectrum of activity of b-lactam antibiotics which are not due to the presence or absence of b-lactamases. Spectrum Based on its spectrum of activity, cefotaxime is classified as a third generation cephalosporin.
For information on the classification of cephalosporins and closely related b-lactam antibiotics based on spectra of activity, see Spectrum in the Cephalosporins General Statement 8:12.06.
Like other currently available parenteral third generation cephalosporins (e.g., cefoperazone, ceftazidime, ceftizoxime, ceftriaxone), cefotaxime generally is less active in vitro against susceptible staphylococci than first generation cephalosporins but has an expanded spectrum of activity against gram-negative bacteria compared with first and second generation cephalosporins.
The spectrum of activity of cefotaxime closely resembles that of ceftizoxime and ceftriaxone. In vitro on a weight basis, the activity of cefotaxime against most susceptible Enterobacteriaceae is approximately equal to that of ceftizoxime or ceftriaxone.
Cefotaxime is inactive against Chlamydia, fungi, and viruses.
The major metabolite of cefotaxime, desacetylcefotaxime, is also microbiologically active. In vitro, desacetylcefotaxime has only about 10% of the antibacterial activity of cefotaxime. However, desacetylcefotaxime is more active in vitro against susceptible gram-positive aerobic bacteria than is cefazolin or cefoxitin. It has been suggested that the antibacterial activity of desacetylcefotaxime may be clinically important in infections in patients with impaired renal function or in infections in organs or tissues where desacetylcefotaxime accumulates. Preliminary data indicate that the antibacterial activities of cefotaxime and desacetylcefotaxime are additive or synergistic against cefotaxime-susceptible S. aureus and Enterobacteriaceae.
In Vitro Susceptibility Testing
For most organisms, inoculum size, pH, test media, and presence of serum do not appear to influence results of in vitro cefotaxime susceptibility tests. However, results of susceptibility tests for some gram-negative bacilli (especially Proteus, Providencia, Pseudomonas aeruginosa, Klebsiella, and Serratia marcescens) may be greatly affected by the size of the inoculum.
The National Committee for Clinical Laboratory Standards (NCCLS) states that, if results of in vitro susceptibility testing indicate that a clinical isolate is susceptible to cefotaxime, then an infection caused by this strain may be appropriately treated with the dosage of the drug recommended for that type of infection and infecting species, unless otherwise contraindicated.
If results indicate that a clinical isolate has intermediate susceptibility to cefotaxime, then the strain has a minimum inhibitory concentration (MIC) that approaches usually attainable blood and tissue drug concentrations and response rates may be lower than for strains identified as susceptible.
Therefore, the intermediate category implies clinical applicability in body sites where the drug is physiologically concentrated (e.g., urine) or when a high dosage of the drug can be used. This intermediate category also includes a buffer zone which should prevent small, uncontrolled technical factors from causing major discrepancies in interpretation, especially for drugs with narrow pharmacotoxicity margins.
If results of in vitro susceptibility testing indicate that a clinical isolate is resistant to cefotaxime, the strain is not inhibited by systemic concentrations of the drug achievable with usual dosage schedules and/or MICs fall in the range where specific microbial resistance mechanisms are likely and efficacy has not been reliably demonstrated in clinical trials. Strains of staphylococci resistant to penicillinase-resistant penicillins also should be considered resistant to cefotaxime, although results of in vitro susceptibility tests may indicate that the organisms are susceptible to the drug.
Disk Susceptibility Tests
When the disk-diffusion procedure is used to test susceptibility to cefotaxime, a disk containing 30 mcg of cefotaxime should be used. The cephalosporin class disk containing 30 mcg of cephalothin or disks containing other cephalosporins should not be used for testing susceptibility to cefotaxime.
When disk-diffusion susceptibility testing is performed according to NCCLS standardized procedures using NCCLS interpretive criteria, Staphylococcus, Enterobacteriaceae, Pseudomonas aeruginosa, or Acinetobacter with growth inhibition zones of 23 mm or greater are susceptible to cefotaxime, those with zones of 15-22 mm have intermediate susceptibility, and those with zones of 14 mm or less are resistant to cefotaxime.
When disk-diffusion susceptibility testing is performed according to NCCLS standardized procedures using Haemophilus test medium (HTM), Haemophilus with growth inhibition zones of 26 mm or greater are considered susceptible to cefotaxime.
Because of limited data on resistant strains of the organism, NCCLS recommends that any Haemophilus isolate that appears to be nonsusceptible to cefotaxime be submitted to a reference laboratory for further testing. When disk-diffusion susceptibility testing is performed according to NCCLS standardized procedures using GC agar based (with 1% defined growth supplement), N. gonorrhoeae with growth inhibition zones of 31 mm or greater are considered susceptible to cefotaxime.
Because of limited data on resistant strains of the organism, NCCLS recommends that any N. gonorrhoeae isolate that appears to be nonsusceptible to cefotaxime be submitted to a reference laboratory for further testing. Interpretive criteria are not available to determine susceptibility of Streptococcus pneumoniae to cefotaxime using the disk-diffusion procedure, and NCCLS suggests that susceptibility of this organism to cefotaxime is best assessed using a dilution procedure.
NCCLS states that S. pneumoniae found to be susceptible to penicillin using a 1-mcg oxacillin disk and the NCCLS standardized procedure can be considered susceptible to cefotaxime.
When the NCCLS standardized procedure for disk susceptibility testing of streptococci is performed using Mueller-Hinton agar (supplemented with 5% sheep blood), viridans streptococci with growth inhibition zones of 28 mm or greater are susceptible to cefotaxime, those with zones of 26-27 mm have intermediate susceptibility, and those with zones of 25 mm or less are resistant to the drug.
When this procedure is used to test susceptibility of b-hemolytic streptococci, those with growth inhibition zones of 24 mm or greater are considered susceptible to cefotaxime. Because of limited data on resistant strains of the organism, NCCLS recommends that any b-hemolytic streptococcal isolate that appears to be nonsusceptible to cefotaxime be submitted to a reference laboratory for further testing.
Dilution Susceptibility Tests
When dilution susceptibility testing (agar or broth dilution) is performed according to NCCLS standardized procedures using NCCLS interpretive criteria, Staphylococcus, Enterobacteriaceae, and Ps. aeruginosa and other non-Enterobacteriaceae gram-negative bacilli (e.g., other Pseudomonas spp., Acinetobacter, Stenotrophomonas maltophilia) with MICs of 8 mcg/mL or less are susceptible to cefotaxime, those with MICs of 16-32 mcg/mL have intermediate susceptibility, and those with MICs of 64 mcg/mL or greater are resistant to the drug.
When dilution susceptibility testing of Haemophilus is performed according to NCCLS standardized procedures using HTM, isolates with MICs of 2 mcg/mL or less are considered susceptible to cefotaxime. Because of limited data on resistant strains of Haemophilus, NCCLS recommends that any isolate that appears to be nonsusceptible to cefotaxime be submitted to a reference laboratory for further testing.
When dilution susceptibility testing of N. gonorrhoeae is performed according to NCCLS standardized procedures using GC agar base (with 1% defined growth supplement), N. gonorrhoeae with MICs of 0.5 mcg/mL or less are considered susceptible to cefotaxime.
Because of limited data on resistant strains of N. gonorrhoeae, NCCLS recommends that any isolate that appears to be nonsusceptible to cefotaxime be submitted to a reference laboratory for further testing.
When broth dilution susceptibility testing of S. pneumoniae is performed according to NCCLS standardized procedures using cation-adjusted Mueller-Hinton broth (supplemented with 2-5% lysed horse blood), S. pneumoniae isolates from patients with meningitis with MICs of 0.5 mcg/mL or less are susceptible to cefotaxime, those with MICs of 1 mcg/mL have intermediate susceptibility, and those with MICs of 2 mcg/mL or greater are resistant to the drug. NCCLS states that S. pneumoniae isolates from patients with infections other than meningitis with MICs of 1 mcg/mL or less are susceptible to cefotaxime, those with MICs of 2 mcg/mL have intermediate susceptibility, and those with MICs of 4 mcg/mL or greater are resistant to the drug. In addition, NCCLS states that S. pneumoniae isolates found to be susceptible to penicillin using NCCLS standardized broth dilution procedure can be considered susceptible to cefotaxime.
When broth dilution susceptibility testing of viridans streptococci is performed according to NCCLS standardized procedures, those with MICs of 1 mcg/mL or less are susceptible to cefotaxime, those with MICs of 2 mcg/mL have intermediate susceptibility, and those with MICs of 4 mcg/mL or greater are resistant to the drug.
When broth dilution susceptibility testing of b-hemolytic streptococci is performed according to NCCLS standardized procedure, those with cefotaxime MICs of 0.5 mcg/mL or less are considered susceptible to the drug.
Because of limited data on resistant strains, NCCLS recommends that any b-hemolytic streptococcal isolate that appears to be nonsusceptible to cefotaxime be submitted to a reference laboratory for further testing.
Gram-positive Aerobic Bacteria
In vitro, cefotaxime concentrations of 0.5 mcg/mL or less inhibit most strains of Streptococcus pneumoniae, S. pyogenes (group A b-hemolytic streptococci), and S. agalactiae (group B streptococci).
Some strains of viridans streptococci are inhibited in vitro by cefotaxime concentrations of 4 mcg/mL or less. In one study, the MIC50 and MIC90 of cefotaxime for the S. milleri group of viridans streptococci (S. anginosus, S. constellatus, S. intermedius) were 0.25 and 0.5 mcg/mL, respectively. Cefotaxime concentrations of 4 mcg/mL or less inhibit most strains of Staphylococcus aureus in vitro.
Cefotaxime is active in vitro against most strains of penicillinase-producing S. aureus; however, almost all strains of staphylococci resistant to penicillinase-resistant penicillins are also resistant to cefotaxime. The MIC90 (minimum inhibitory concentration of the drug at which 90% of strains are inhibited) of cefotaxime for S. epidermidis generally is 4.8-16 mcg/mL, although lower MIC90s have been reported occasionally; in a few studies, however, the MIC90 was 64 mcg/mL or greater. Listeria monocytogenes and enterococci, including E. faecalis (formerly S. faecalis), generally are resistant to the drug. Strains of S. pneumoniae with MICS of 2 mcg/mL or greater generally are considered resistant to cefotaxime; however, strains with MICs of 0.5-1 mcg/mL that are isolated from patients with meningitis generally also are considered resistant to the drug. The MIC90 of desacetylcefotaxime reported for susceptible S. pneumoniae and S. pyogenes is 4 mcg/mL or less. S. aureus is generally resistant to desacetylcefotaxime.
Gram-negative Aerobic Bacteria
Cefotaxime is active in vitro against a wide variety of gram-negative bacteria including most Enterobacteriaceae and some strains of Pseudomonas aeruginosa. Cefotaxime is active against some gram-negative bacteria that are resistant to first and second generation cephalosporins and currently available penicillins and aminoglycosides, especially Escherichia coli, Klebsiella pneumoniae, and Serratia marcescens.
Enterobacteriaceae
Generally, cefotaxime is active in vitro against the following Enterobacteriaceae: Citrobacter freundii, C. diversus, Enterobacter aerogenes, E. cloacae, Escherichia coli, Klebsiella pneumoniae, K. oxytoca, Morganella morganii (formerly Proteus morganii), Proteus mirabilis, P. vulgaris, Providencia stuartii (formerly group B Proteus inconstans), P. rettgeri (formerly Proteus rettgeri), Salmonella, Serratia marcescens, Shigella, and Yersinia enterocolitica. The MIC90 of cefotaxime for many of these gram-negative bacilli is 4 mcg/mL or less.
However, the MIC90 of cefotaxime for C. freundii, E. aerogenes, E. cloacae, M. morganii, and Serratia generally ranges from 0.1-32 mcg/mL, although higher MIC90s have been reported. The MIC90 of desacetylcefotaxime reported for susceptible E. coli, K. pneumoniae, P. mirabilis, and Providencia stuartii is 4 mcg/mL or less; E. aerogenes, E. cloacae, M. morganii, P. vulgaris, and S. marcescens are generally resistant to desacetylcefotaxime.
Pseudomonas
The in vitro activity of cefotaxime against Pseudomonas is variable. Although some strains of Ps. aeruginosa and Ps. maltophilia (Stenotrophomonas maltophilia) are inhibited in vitro by cefotaxime concentrations of 32 mcg/mL or less, most strains of these organisms require cefotaxime concentrations of 64 mcg/mL or greater for in vitro inhibition and are therefore considered resistant to the drug. Cefotaxime is less active in vitro against susceptible Ps. aeruginosa than is cefoperazone, cefsulodin, ceftazidime, or some extended-spectrum penicillins. Ps. aeruginosa generally is resistant to desacetylcefotaxime.
Other Gram-negative Aerobic Bacteria
Cefotaxime is active in vitro against Haemophilus influenzae (including ampicillin-resistant strains) and H. parainfluenzae. The MIC90s of cefotaxime reported for H. influenzae and H. parainfluenzae are 0.01-0. and 0.024-4 mcg/mL, respectively, and the MIC90 of desacetylcefotaxime reported for H. influenzae is 4 mcg/mL or less.
Cefotaxime is active in vitro against Neisseria meningitidis and Neisseria gonorrhoeae. The MIC90 of cefotaxime reported for N. gonorrhoeae (including both penicillinase-producing and nonpenicillinase-producing strains) is 0.1-0.4 mcg/mL. Both b-lactamase- and non-b-lactamase-producing strains of Moraxella (formerly Branhamella) catarrhalis are inhibited in vitro by cefotaxime concentrations of 0.03-0.5 mcg/mL.
Cefotaxime is active in vitro against Eikenella corrodens, and the MIC90 of the drug for this organism generally is 0.06-0.5 mcg/mL. Campylobacter fetus subsp. jejuni, an organism that can be microaerophilic or anaerobic, generally is inhibited in vitro by cefotaxime concentrations of 2-6.25 mcg/mL.
Although cefotaxime has some activity in vitro against Acinetobacter, the MIC90 of the drug generally ranges from 8-32 mcg/mL for A. calcoaceticus var. lwoffi and from 16-32 mcg/mL for A. calcoaceticus var. anitratus; higher MIC90s also have been reported. In vitro, some strains of Bartonella bacilliformis are inhibited by cefotaxime concentrations of 0.03-0.12 mcg/mL.
While some strains of Burkholderia cepacia (formerly Pseudomonas cepacia) are inhibited in vitro by cefotaxime concentrations of 16 mcg/mL, the MIC90 of the drug for this organism is 64 mcg/mL and most strains are resistant to the drug. Cefotaxime is active in vitro against Capnocytophaga. In an in vitro study, the MIC90 of cefotaxime for Capnocytophaga was 0.25 mcg/mL. Cefotaxime-resistant strains of C. sputigena (formerly CDC group DF-1) have been reported. Vibrio vulnificus may be inhibited in vitro by cefotaxime concentrations of 0.03 mcg/mL.
While the clinical importance is unclear, results of an in vitro study and a study in mice indicate that the combination of cefotaxime and minocycline is more active against V. vulnificus than either anti-infective alone.
Anaerobic Bacteria
Cefotaxime is active in vitro against Bacteroides, Eubacterium, Fusobacterium, Peptococcus, Peptostreptococcus, Propionibacterium, and Veillonella. Cefotaxime is also active against some strains of Clostridium including C. perfringens; however, C. difficile is usually resistant to the drug. Although the MIC90 of cefotaxime reported for most susceptible anaerobes is 16 mcg/mL or less, cefotaxime concentrations of 16-64 mcg/mL are generally required in vitro to inhibit Bacteroides (including B. fragilis). In vitro, cefotaxime is less active than cefoxitin against susceptible B. fragilis.
Spirochetes
Borrelia burgdorferi, the causative organism of Lyme disease, reportedly may be inhibited in vitro by a cefotaxime concentration of 0.12 mcg/mL. BR>Resistance For information on possible mechanisms of bacterial resistance to cephalosporins, see Resistance in the Cephalosporins General Statement 8:12.06. Because cefotaxime contains an a-syn-methoximino group which protects the b-lactam ring from hydrolysis by many penicillinases and cephalosporinases, cefotaxime is more resistant to hydrolysis by most b-lactamases than first and second generation cephalosporins.
Cefotaxime is generally resistant to hydrolysis by b-lactamases classified as Richmond-Sykes types I, II, III, IV, and V, and most penicillinases produced by S. aureus. However, b-lactamases produced by B. fragilis and P. vulgaris can slowly hydrolyze cefotaxime. Resistant strains of some organisms, especially Enterobacter, Ps. aeruginosa, or Serratia, have developed during therapy with cefotaxime. Strains of Ps. aeruginosa which are only moderately susceptible to cefotaxime in vitro at the beginning of therapy appear to be especially likely to become resistant during therapy.
Like most cephalosporins and penicillins, cefotaxime is inactivated by inducible, chromosomally mediated b-lactamases produced by some strains of Citrobacter, Enterobacter, Pseudomonas, and Serratia.
Therefore, organisms that possess inducible b-lactamases are usually resistant to cefotaxime following derepression of the enzymes. Inducible b-lactamases may be derepressed by mutation to a stable derepressed state or may be reversibly derepressed by an enzyme inducer.
Cefoxitin, cefotetan, and imipenem are potent inducers of these enzymes, and in vitro exposure of organisms possessing these enzymes to these drugs results in resistance to cefotaxime as well as to many other b-lactam antibiotics. Inducible b-lactamases inactivate cephalosporins and penicillins either by hydrolyzing the drugs or by binding to them to prevent access to penicillin-binding proteins (PBPs).
The clinical importance of these inducible b-lactamases is unclear, but emergence of cefotaxime resistance in some organisms during therapy with the drug may be related to these enzymes. Strains of S. pneumoniae considered resistant to cefotaxime have been reported with increasing frequency. These strains generally have intermediate- or high-level resistance to penicillin G as well as decreased susceptibility to third generation cephalosporins. Resistance to cefotaxime in S. pneumoniae appears to be related to alterations in the PBPs of the organism. Tolerance to cefotaxime has been reported to occur in some bacteria including some strains of Enterobacter, Proteus, and Ps. aeruginosa. In vitro, tolerant bacteria have a minimum bactericidal concentration (MBC) of cefotaxime which is much greater than the MIC of the drug.
Bacteria which are tolerant to cefotaxime appear to be inhibited but not necessarily killed by the drug. Preliminary studies suggest that tolerant organisms may have decreased concentrations of autolysins or an increased concentration of an unidentified inhibitor of autolysis. Tolerance may be important clinically since infections caused by these organisms may persist during cefotaxime therapy despite in vitro susceptibility tests which indicate that the organisms are susceptible to the drug.
Pharmacokinetics
In all studies described in the Pharmacokinetics section, cefotaxime was administered as the sodium salt; dosages of the drug are expressed in terms of cefotaxime.
The antibacterial activity of both cefotaxime and its major metabolite, desacetylcefotaxime, must be considered when attempting to correlate the pharmacokinetics with the therapeutic effect of the drug. In early published studies on the pharmacokinetics of cefotaxime, microbiologic assays were used to determine body fluid and tissue concentrations of the drug.
Microbiologic assays which used test organisms susceptible to cefotaxime but resistant to desacetylcefotaxime accurately reflect concentrations of the parent drug; however, microbiologic assays used in some published pharmacokinetic studies of cefotaxime actually measured total microbiologic activity since both cefotaxime and desacetylcefotaxime were active against the test organism.
Information on body fluid and tissue concentrations of cefotaxime obtained from studies that used nonspecific microbiologic assays or from studies that did not identify the test organism used is reported as microbiologic activity in the following sections on the pharmacokinetics of the drug.
More recent pharmacokinetic studies generally use high-performance liquid chromatography (HPLC) that differentiates between cefotaxime and desacetylcefotaxime and can specifically measure concentrations of cefotaxime and/or its metabolite.
Absorption
Cefotaxime is not appreciably absorbed from the GI tract and must be given parenterally. Following IM administration of a single 500-mg or 1-g dose of cefotaxime in healthy adults with normal renal function, peak serum concentrations of the drug are attained within 30 minutes and average 11.-11. mcg/mL and 20.-25. mcg/mL, respectively.
Plasma concentrations of cefotaxime are undetectable 8 hours after a single 500-mg IM dose of the drug but average 1 mcg/mL 8 hours after a single 1-g IM dose of the drug. In one multiple-dose study in adults with normal renal function receiving 500-mg doses of cefotaxime by IM injection every 8 hours, steady-state peak serum concentrations of cefotaxime ranged from 9.2-11.9 mcg/mL and steady-state trough serum concentrations of the drug ranged from 0.1-0. mcg/mL.
In one study in healthy adults with normal renal function, a single 500-mg, 1-g, or 2-g dose of cefotaxime given by IV injection over 5 minutes resulted in serum concentrations of cefotaxime which averaged 37.9 mcg/mL, 102.4 mcg/mL, and 214. mcg/mL, respectively, immediately after the injection; serum concentrations of the drug averaged 1 mcg/mL, 1.9 mcg/mL, and 3.3 mcg/mL, respectively, 4 hours after the injection. In a multiple-dose study in healthy adults with normal renal function receiving 1-g doses of cefotaxime every 6 hours by IV infusion over 30 minutes, steady-state peak serum concentrations of cefotaxime ranged from 40.6-46 mcg/mL and steady-state trough serum concentrations of the drug ranged from 1.1-1.6 mcg/mL.
Following a single cefotaxime dose of 50 mg/kg given by IV infusion over 10 minutes in average birthweight neonates 1-7 days of age, microbiologic activity in serum averaged 133 mcg/mL immediately after completion of the infusion, 85 mcg/mL 1 hour later, 52 mcg/mL 4 hours later, and 38 mcg/mL 6 hours later. In one study in children 1 month to 12 years of age, serum concentrations of cefotaxime averaged 25.3 mcg/mL 30 minutes after a single cefotaxime dose of 25 mg/kg given by IM injection and averaged 53.3 mcg/mL 5 minutes after a single dose of 25 mg/kg of the drug given by IV injection.
Distribution
Following IM or IV administration of usual dosages of cefotaxime, microbiologic activity is widely distributed into body tissues and fluids including the aqueous humor, bronchial secretions, sputum, middle ear effusions, bone, bile, and ascitic, pleural, and prostatic fluids. The apparent volume of distribution of cefotaxime in adults is reported to be 0.22-0.29 L/kg. Cefotaxime is 13-38% bound to serum proteins in vitro.
Cefotaxime and its major metabolite are distributed into CSF following parenteral administration. Following IV administration of a single 2-g IV dose of cefotaxime in patients with uninflamed meninges, low concentrations of cefotaxime (0.-1. mcg/mL) and desacetylcefotaxime (0.06-0.38 mcg/mL) are attained in CSF; however, higher concentrations are attained in patients with inflamed meninges. In one study in neonates and children 2 weeks to 2 years of age with inflamed meninges, IV injection or infusion over 30 minutes of cefotaxime doses of 50 mg/kg every 4-6 hours resulted in microbiologic activity in CSF which ranged from 1-13.2 mcg/mL 1-4 hours after administration.
In another study in children 2 months to 12 years of age with meningitis who received cefotaxime in a dosage of 50 mg/kg IV every 6 hours, CSF concentrations of cefotaxime or its major metabolite averaged 6.2 or 5.6 mcg/mL, respectively, 1 hour after a dose; concurrent serum concentrations were 61. and 19. mcg/mL, respectively. In a study in adults with bacterial meningitis receiving 2 g of cefotaxime IV every 4 hours, trough CSF cefotaxime and desacetylcefotaxime concentrations ranged from 5.6-44. mcg/mL and 3.7-44 mcg/mL, respectively, after 1-3 days of therapy. Following IM or IV administration of usual dosages of cefotaxime, microbiologic activity in hepatic bile is reported to be 15-75% of concurrent microbiologic activity in serum and microbiologic activity in gallbladder bile is reported to be up to 3 times greater than concurrent microbiologic activity in serum.
Microbiologic activity in ascitic fluid is reported to be 40% of concurrent microbiologic activity in serum. In patients receiving 2-g doses of cefotaxime IV every 6 hours, concentrations of cefotaxime and desacetylcefotaxime in bronchial secretions averaged 1.7 and 5.8 mcg/mL, respectively, and plasma concentrations averaged 23.1 and 9.3 mcg/mL, respectively, in samples obtained 1-2 hours after the fourth dose.
Cefotaxime readily crosses the placenta, and microbiologic activity in amniotic fluid is reported to be equal to or greater than concurrent microbiologic activity in maternal serum following multiple doses of the drug. Cefotaxime is distributed into milk. In one study, microbiologic activity in milk ranged from 0.25-0. mcg/mL 2-3 hours after a single 1-g IV dose of cefotaxime.
Elimination
Cefotaxime is partially metabolized in the liver to desacetylcefotaxime which has antibacterial activity. (See Spectrum.)
Desacetylation of cefotaxime occurs rapidly in vivo and rapidly in vitro in hemolyzed blood. Following IV injection over 5 minutes of a single 500-mg or 2-g dose of cefotaxime in adults with normal renal function, peak plasma concentrations of desacetylcefotaxime are generally attained within 45 minutes and average 2.7 mcg/mL and 9.8 mcg/mL, respectively.
Desacetylcefotaxime is partially converted in the liver to desacetylcefotaxime lactone which is inactive and is further degraded to 2 unidentified inactive metabolites currently designated as UP1 and its optical isomer UP2. Serum concentrations of cefotaxime appear to decline in a biphasic manner. In adults with normal renal function, the serum half-life of cefotaxime in the initial phase (t1/2a) averages 0.2-0. hours and the serum half-life of the drug in the terminal phase (t1/2b) averages 0.9-1. hours.
The t1/2b of desacetylcefotaxime is longer than that of the parent drug and is reported to be 1.4-1.9 hours in adults with normal renal function. In adults with renal impairment, the t1/2a of cefotaxime is not affected, and the t1/2b is only slightly prolonged in patients with creatinine clearances of 20 mL/min or greater per 1.73 m. In adults with creatinine clearances of 10 mL/min or less per 1.73 m, the t1/2? of cefotaxime is reported to range from 1.4-11. hours and the t1/2? of desacetylcefotaxime is reported to range from 8.2-56. hours. The t1/2b of both cefotaxime and desacetylcefotaxime may be prolonged in patients with impaired hepatic function. In a study in patients with chronic parenchymal liver disease with or without jaundice, edema, or ascites, the t1/2b of the parent drug ranged from 1.49-2. hours and the apparent t1/2 of the metabolite ranged from 7.1-13. hours. In one study in children 5 months to 1 year of age, the t1/2a of cefotaxime averaged 0.2 hours and the t1/2? averaged 1.2 hours. In children 2-12 years of age, the t1/2a averaged 0.3 hours and the t1/2b averaged 1.5 hours. In neonates, the half-life of cefotaxime depends principally on gestational and chronologic age. The t1/2a is reported to range from 0.1-0. hours in premature or full-term neonates.
The t1/2b of cefotaxime averages 5-6 hours in premature neonates less than 1 week of age, 3.4-3.5 hours in premature neonates 1-4 weeks of age, 2-3.4 hours in full-term neonates less than 1 week of age, and 2 hours in full-term neonates 1-4 weeks of age. Cefotaxime and its metabolites are excreted principally in urine; tubular secretion of the drug occurs. In adults with normal renal function, approximately 40-60% of a single IM or IV dose of cefotaxime is excreted in urine as unchanged drug and approximately 24% is excreted as desacetylcefotaxime within 24 hours.
The majority of the IM or IV dose is excreted within the first 2 hours following administration. In one study, urine concentrations of cefotaxime ranged from 90-3261 mcg/mL in urine collected over 2 hours following a single 500-mg IM dose of cefotaxime. The serum clearance of cefotaxime in adults with normal renal function is reported to be 207-342 mL/minute per 1.73 m. In one study, the serum clearance of the drug averaged 23 mL/minute per 1.73 m in low birthweight neonates 1-7 days of age and 44 mL/minute per 1.73 m in average birthweight neonates 1-7 days of age.
Oral probenecid administered shortly before or concomitantly with cefotaxime usually slows the rate of excretion of the antibiotic and its metabolites and produces higher and more prolonged serum concentrations of cefotaxime and its metabolites. The volume of distribution of cefotaxime does not appear to be affected by concomitant administration of oral probenecid. Cefotaxime and its metabolites are removed by hemodialysis.
The amount of cefotaxime removed during hemodialysis depends on several factors (e.g., type of coil used, dialysis flow-rate); however, a 4- to 6-hour period of hemodialysis in one study removed into the dialysate 60% of a single 15 mg/kg dose of cefotaxime when the dose was given by IV injection immediately prior to dialysis. Only minimal amounts of cefotaxime are removed by peritoneal dialysis.
Chemistry and Stability
Chemistry
Cefotaxime is a semisynthetic cephalosporin antibiotic. Like cefepime, ceftazidime, ceftizoxime, and ceftriaxone, cefotaxime is a parenteral aminothiazolyl cephalosporin. Cefotaxime contains an aminothiazolyl-acetyl side chain, with an a-syn-methoximino group, at position 7 of the cephalosporin nucleus. The aminothiazolyl side chain enhances antibacterial activity, particularly against Enterobacteriaceae, and generally results in enhanced stability against b-lactamases; the methoximino group contributes to stability against hydrolysis by many b-lactamases.
Cefotaxime is commercially available as the sodium salt. Potency of cefotaxime sodium is expressed in terms of cefotaxime. Cefotaxime sodium occurs as an off-white to pale yellow, crystalline powder. Cefotaxime sodium is sparingly soluble in water, slightly soluble in alcohol, and has a pKa of 3.4. The sodium salt of cefotaxime contains 2.2 mEq of sodium per gram of cefotaxime. Commercially available frozen cefotaxime sodium injections are pale yellow to light amber solutions containing 1 or 2 g of cefotaxime in 50 mL of 5% dextrose injection and have osmolalities of 340-420 or 440-540 mOsm/kg, respectively, and a pH of 5-7..
Stability
Commercially available cefotaxime sodium sterile powder for injection should be stored at less than 30°C. The commercially available frozen cefotaxime sodium injection should be stored at a temperature not greater than -20°C.
Cefotaxime sodium powder for injection and solutions of the drug tend to darken, depending on storage conditions, and should be protected from excess heat and light. Discoloration of cefotaxime sodium sterile powder for injection or solutions of the drug may indicate a loss of potency. Following reconstitution with sterile or bacteriostatic water for injection, 0.9% sodium chloride injection, or 5% dextrose injection, cefotaxime sodium solutions containing 50-330 mg of cefotaxime per mL have a pH of 4.5-6.5 and are light yellow to amber in color.
These extemporaneously prepared solutions are stable in their original containers for 24 hours at room temperature, 10 days when refrigerated at 5°C or less, or at least 13 weeks when frozen. In disposable glass or plastic syringes, these solutions are stable for 24 hours at room temperature, 5 days when refrigerated at 5°C or less, or 13 weeks when frozen. When reconstituted as directed in 0.9% sodium chloride injection or 5% dextrose injection, solutions prepared from ADD-Vantage® vials of the drug are stable for 24 hours at a room temperature of 22°C or less; these solutions should not be frozen. The manufacturer states that the stability of the commercially available frozen cefotaxime sodium injection may vary.
These injections are stable for at least 90 days from the date of shipment when stored at -20°C. The frozen injection should be thawed at room temperature or under refrigeration (at 5°C or lower) and, once thawed, should not be refrozen. Frozen injections should not be thawed by immersion in water baths or by exposure to microwave radiation.
Thawed solutions of the commercially available frozen injection are stable for 24 hours at room temperature (22°C or lower) or 10 days when refrigerated at 5°C or lower. The commercially available frozen injection of the drug is provided in a plastic container fabricated from specially formulated multilayered plastic PL 2040 (Galaxy®). Solutions in contact with the plastic can leach out some of its chemical components in very small amounts within the expiration period of the injection; however, safety of the plastic has been confirmed in tests in animals according to USP biological tests for plastic containers as well as by tissue culture toxicity studies. Cefotaxime sodium is physically and chemically compatible with the following IV solutions: 0.9% sodium chloride; 5% or 10% dextrose; 5% dextrose and 0.2%, 0.45%, or 0.9% sodium chloride; lactated Ringer’s; 1/4 M sodium lactate; 10% invert sugar; or Travasol® 8.5%.
Reconstituted solutions of cefotaxime sodium which have been further diluted with 50 mL to 1 liter of one of the above IV solutions are physically and chemically stable for 24 hours at room temperature or at least 5 days when refrigerated at 5°C or less. The manufacturer states that solutions of cefotaxime sodium are most stable at a pH of 5-7 and that the drug should not be diluted with IV solutions (e.g., sodium bicarbonate) which have a pH greater than 7.5. The manufacturer states that reconstituted solutions of cefotaxime sodium which have been further diluted with 50 mL to 1 liter of 0.9% sodium chloride injection or 5% dextrose injection may be frozen in Viaflex® containers immediately after preparation and are stable for 13 weeks.
Frozen solutions of cefotaxime sodium should be thawed at room temperature. Once thawed, solutions are stable for 24 hours at room temperature or 5 days at less than 5°C and should not be refrozen.
Cefotaxime sodium is potentially physically and/or chemically incompatible with some drugs, including aminoglycosides, but the compatibility depends on several factors (e.g., concentrations of the drugs, specific diluents used, resulting pH, temperature). Specialized references should be consulted for specific compatibility information. Because of the potential for incompatibility, the manufacturer states that cefotaxime sodium and aminoglycosides should not be admixed.
Preparations
Cefotaxime Sodium Parenteral For injection 500 mg (of cefotaxime) Cefotaxime Sodium for Injection, American Pharmaceutical Partners Claforan®, Aventis 1 g (of cefotaxime) Cefotaxime Sodium for Injection, American Pharmaceutical Partners Claforan®, Aventis 2 g (of cefotaxime) Cefotaxime Sodium for Injection, American Pharmaceutical Partners Claforan®, Aventis 10 g (of cefotaxime) Cefotaxime Sodium for pharmacy bulk package Injection, American Pharmaceutical Partners Claforan®, Aventis 20 g (of cefotaxime) Cefotaxime Sodium for pharmacy bulk package Injection, American Pharmaceutical Partners For injection, for 1 g (of cefotaxime) Claforan®, IV infusion Aventis Claforan® ADD-Vantage®, Aventis 2 g (of cefotaxime) Claforan®, Aventis Claforan® ADD-Vantage®, Aventis Cefotaxime Sodium in Dextrose Parenteral Injection (frozen) 20 mg (of cefotaxime) per mL Cefotaxime Sodium in Iso- , for IV infusion (1 g) in 3.4% Dextrose osmotic Dextrose Injection, (Galaxy®) Baxter 40 mg (of cefotaxime) per mL Cefotaxime Sodium in Iso- (2 g) in 1.4% Dextrose osmotic Dextrose Injection, (Galaxy®) Baxter

