Clindamycin is a semisynthetic antibiotic that is a derivative of lincomycin. It is active against most aerobic gram-positive cocci, including staphylococci, Streptococcus pneumoniae, and other streptococci (except Enterococcus faecalis, formerly S. faecalis).

Clindamycin is effective in vitro against various bacteria, including gram-positive and anaerobic organisms. It targets pathogens such as Arcanobacterium haemolyticum, Actinomyces, Bacteroides, and Fusobacterium. Clindamycin also inhibits Prevotella, Porphyromonas, Mobiluncus, and some strains of Clostridium and Haemophilus influenzae.
In addition, it shows activity against Gardnerella vaginalis. It has some effect on Plasmodium in vitro. Still, it is ineffective against N. meningitidis, Enterobacteriaceae, fungi, and most strains of C. difficile. The minimum inhibitory concentration (MIC) for clindamycin typically ranges from 0.04 to 4 mcg/mL for susceptible strains of staphylococci, streptococci, and anaerobic bacteria.
Pharmacokinetics
Clindamycin may be bacteriostatic or bactericidal in action, depending on the concentration of the drug at the site of infection and the susceptibility of the infecting organism. Clindamycin palmitate hydrochloride and clindamycin phosphate are inactive until hydrolyzed to free clindamycin. This hydrolysis occurs rapidly in vivo. Clindamycin appears to inhibit protein synthesis in susceptible organisms by binding to 50S ribosomal subunits; the primary effect is the inhibition of peptide bond formation. The site of action appears to be the same as that of erythromycin, chloramphenicol, lincomycin, oleandomycin, and troleandomycin.
Absorption
About 90% of oral clindamycin hydrochloride is rapidly absorbed after being converted to active clindamycin in the GI tract. Serum concentrations rise linearly with dosage and are minimally affected by food, though peak levels may be delayed. After a 150-mg dose, peak serum levels average 1.9-3.9 mcg/mL within 45-60 minutes.
Clindamycin phosphate is quickly hydrolyzed to active clindamycin for IM or IV administration. Peak serum concentrations occur within 3 hours for adults and 1 hour for children.
Distribution
Clindamycin distributes widely in body tissues and fluids but poorly penetrates the CSF. Concentrations in synovial fluid and bone are about 60-80% of serum levels. It crosses the placenta and is present in breast milk, with approximately 93% bound to serum proteins.
Elimination
The serum half-life is typically 2-3 hours in adults and children and longer in those with renal or hepatic impairment. In neonates, it varies by age and weight. Clindamycin is partially metabolized and excreted mainly in urine and feces. About 10% of an oral dose appears in urine within 24 hours as active drugs and metabolites. Probenecid does not affect its excretion.
Uses
Before selecting clindamycin, the physician should consider the nature of the infection and the suitability of less toxic alternatives (e.g., erythromycin).
Clindamycin primarily treats serious infections caused by susceptible gram-positive and anaerobic bacteria. Due to a higher risk of Clostridium difficile-associated diarrhea and colitis, its use should be limited to serious infections when other less toxic antibiotics are unavailable. C. difficile-related issues are common with many antibiotics, particularly clindamycin, cephalosporins, and ampicillin. Clindamycin should not be used empirically for infections likely of nonbacterial origin, such as upper respiratory tract infections. Before treatment, the causative organism should be cultured, and clindamycin does not replace the need for surgical interventions when necessary. Additionally, it is ineffective in treating meningitis due to poor CNS distribution.
Clindamycin is also indicated in treating serious infections due to susceptible strains of streptococci, pneumococci, and staphylococci. Its use should be reserved for penicillin-allergic patients or other patients for whom, in the physician’s judgment, penicillin is inappropriate.
- Anaerobes: Serious respiratory tract infections such as empyema, anaerobic pneumonitis, and lung abscess; severe skin and soft tissue infections; septicemia; intraabdominal infections such as peritonitis and intra-abdominal abscess (typically resulting from anaerobic organisms resident in the normal gastrointestinal tract); infections of the female pelvis and genital tract such as endometritis, nongonococcal tubo-ovarian abscess, pelvic cellulitis, and postsurgical vaginal cuff infection.
- Streptococci: Serious respiratory tract infections; severe skin and soft tissue infections.
- Staphylococci: Serious respiratory tract infections; severe skin and soft tissue infections.
- Pneumococci: Serious respiratory tract infections.
Bacteriologic studies should be performed to determine the causative organisms and their susceptibility to clindamycin.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of Cleocin and other antibacterial drugs, Cleocin should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered when selecting or modifying antibacterial therapy. Such data is necessary for local epidemiology and susceptibility patterns to contribute to the empiric selection of therapy.
Administration
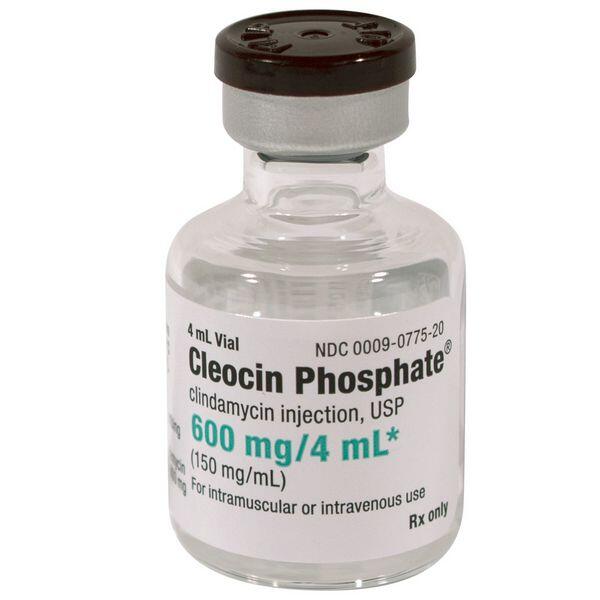
Clindamycin hydrochloride and clindamycin palmitate hydrochloride are administered orally. Clindamycin phosphate is administered by IM injection or intermittent or continuous IV infusion.
Oral Administration
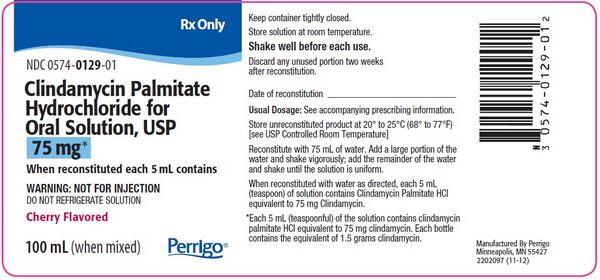
Clindamycin hydrochloride capsules and clindamycin palmitate hydrochloride oral solution can be administered without regard to food. To avoid the possibility of esophageal irritation, clindamycin hydrochloride capsules should be administered orally with a full glass of water.
Clindamycin palmitate hydrochloride oral solution is reconstituted by adding 75 mL of water to the 100-mL bottle; a large portion of the 75 mL should be added initially and the bottle shaken vigorously, and then the remainder of the water should be added and the bottle shaken until the solution is uniform. The resulting solution contains 75 mg of clindamycin per 5 mL.
Parenteral Administration
Before IV administration, clindamycin phosphate injection (including injection contained in ADD-Vantage® vials) must be diluted with a compatible IV solution to a concentration not exceeding 18 mg/mL. For intermittent IV infusion, the diluted solution should be infused over at least 10-60 minutes and at a rate not exceeding 30 mg/minute; the drug should not be administered IV undiluted as a bolus.
The manufacturers suggest that 300- or 600-mg doses of the drug be diluted in 50 mL of diluent and infused over 10 or 20 minutes, respectively, 900-mg doses of the drug be diluted in 50-100 mL of diluent and infused over 30 minutes, or that 1.2-g doses be diluted in 100 mL of diluent and infused over 40 minutes. A maximum of 1.2 g of the drug should be given by IV infusion in a single 1-hour period.
As an alternative to intermittent IV infusion, clindamycin may be given by continuous IV infusion after the first dose of the drug has been given by rapid IV infusion. The commercially available injections of clindamycin phosphate in 5% dextrose are administered by IV infusion. The container should be checked for minute leaks by firmly squeezing the bag. Clindamycin phosphate in 5% dextrose injection should be inspected visually for particulate matter and discoloration before administration whenever solution and container permit.
The injection should be discarded if the container seal is intact, leaks are found, or the solution is not clear. Additives should not be introduced into the injection container.
The injection should not be used in series connections with other plastic containers since such use could result in air embolism from residual air being drawn from the primary container before administration of the fluid from the secondary container is complete. The clindamycin phosphate pharmacy bulk packages are not intended for direct IV infusion; doses of the bulk package must be further diluted in a compatible IV infusion solution before administration.
The bulk package is intended for use only in a laminar flow hood. Entry into the vial should be made using a sterile transfer set or other sterile dispensing device, and the contents should be dispensed in aliquots using the appropriate technique; multiple entries with a syringe and needle are not recommended because of the increased risk of microbial and particulate contamination. The date and time the pharmacy bulk package was opened should be recorded on the pharmacy bulk vial.
After entry into a bulk package vial, the entire contents of the Cleocin Phosphate pharmacy bulk package vial should be used promptly; any unused portion should be discarded within 24 hours after initial entry into the vial. The manufacturer of another clindamycin phosphate pharmacy bulk package (Gensia) states that the contents should be used as soon as possible after initial entry, but within 4 hours; if not used immediately, the vial should be stored at room temperature under the laminar flow hood during this period.
Dosage
Dosage is expressed in terms of clindamycin and depends on the infection’s severity and the infecting organism’s susceptibility. In the treatment of serious anaerobic infections, parenteral clindamycin is usually used initially, and oral clindamycin may be substituted when the condition of the patient warrants; however, in clinically appropriate circumstances, treatment may be initiated or continued with oral clindamycin. The duration of clindamycin therapy depends on the type and severity of the infection. If clindamycin is used in infections caused by group A b-hemolytic streptococci, therapy should be continued for at least 10 days. At least 6 weeks of therapy may be required for severe infections such as endocarditis or osteomyelitis.
Oral Dosage
| Indication | Dosage |
|---|---|
| General Adult Dosage | 150-450 mg every 6 hours, depending on the type and severity of infection. |
| General Pediatric Dosage | 8-25 mg/kg daily, divided into 3 or 4 doses; minimum for ≤10 kg: 37.5 mg three times daily. |
| Bacterial Vaginosis | 300 mg orally twice daily for 7 days (nonpregnant and pregnant women). |
| Prevention of Bacterial Endocarditis | Adults: 600 mg as a single dose; Children: 20 mg/kg as a single dose, not exceeding adult dosage. |
| Toxoplasmosis | Long-term suppressive therapy: 20-30 mg/kg daily in 4 doses with pyrimethamine and leucovorin. |
| Acne | Adults: 150 mg orally twice daily. |
| Malaria | Adults: 900 mg clindamycin 3 times daily for 5 days; Children: 20-40 mg/kg daily in 3 doses. |
| Pharyngitis and Tonsillitis | Children: 20-30 mg/kg daily for 10 days in 3 doses; Adults: 600 mg daily for 10 days in 2-4 doses. |
IM/IV Adult Dosage
| Indication | Dosage |
|---|---|
| General Adult Dosage | 600 mg to 2.7 g daily, divided into 2-4 doses; max single IM dose: 600 mg; max IV infusion: 1.2 g/hour. |
| Life-Threatening Infections | Up to 4.8 g daily via IV. |
| Serum Concentration Maintenance | IV infusion at 10 mg/min for 30 min, then 0.75 mg/min; or 15 mg/min for 30 min, then 1 mg/min; or 20 mg/min for 30 min, then 1.25 mg/min. |
| Pelvic Inflammatory Disease (PID) | 900 mg IV every 8 hours with gentamicin (2 mg/kg initially, then 1.5 mg/kg every 8 hours). |
| Pneumocystis jiroveci Pneumonia | 600 mg IV every 6 hours or 300-450 mg orally every 6 hours for 21 days with primaquine (30 mg daily). |
| Prevention of Perinatal GBS Disease | 900 mg IV every 8 hours until delivery. |
| Prevention of Bacterial Endocarditis | Single dose of 600 mg IV within 30 minutes before procedure. |
| Perioperative Prophylaxis | 600-900 mg IV with gentamicin (1.5 mg/kg) prior to surgery; repeat if needed. |
| Anthrax Treatment | 900 mg IV every 8 hours with ciprofloxacin and rifampin. |
| Babesiosis Treatment | 1.2 g IV twice daily or 600 mg orally three times daily for 7-10 days with oral quinine (650 mg three times daily). |
| Dosage in Renal and Hepatic Impairment | Reduced dosage may be needed for severe impairment; no adjustment for mild/moderate impairment. |
Side Effects
Clindamycin is associated with a range of side effects that can significantly impact patient health. Notably, gastrointestinal disturbances such as nausea, vomiting, and the risk of pseudomembranous colitis due to Clostridium difficile overgrowth are among the most serious adverse reactions linked to its systemic use.
GI Effects
Adverse GI effects frequently occur with oral, IM, or IV clindamycin. They may be severe enough to necessitate discontinuance of the drug. Adverse GI effects of clindamycin include nausea, vomiting, diarrhea, abdominal pain, and tenesmus. In addition, flatulence, bloating, anorexia, weight loss, and esophagitis have occurred. An unpleasant or metallic taste has occurred occasionally following IV administration of high doses of the drug. Nonspecific colitis and diarrhea, as well as potentially fatal Clostridium difficile-associated diarrhea and colitis (also known as antibiotic-associated pseudomembranous colitis), have also occurred in patients receiving clindamycin.
Diarrhea and Colitis
C. difficile-associated diarrhea and colitis, mainly when induced by clindamycin, is marked by severe diarrhea and abdominal cramps and may include blood or mucus in stools. Symptoms often develop 2-9 days after starting clindamycin but can appear weeks later. The condition is more prevalent in hospitalized patients due to nosocomial transmission, with infected humans being the primary reservoirs. Asymptomatic carriers are common in institutions with high rates of symptomatic cases.
The infection is caused by toxin-producing strains of Clostridioides difficile, which are resistant to the antibiotics being administered. Although antibiotic-associated diarrhea of unknown origin is more common, C. difficile may be responsible for 15-25% of cases linked to antibiotic use. Diagnosis typically requires endoscopic examination to identify pseudomembranes.
Treatment involves discontinuing the offending antibiotic and may include supportive care such as fluid and electrolyte replacement. For moderate to severe cases, anti-infective therapies like oral metronidazole or vancomycin are recommended, with metronidazole preferred initially to reduce the risk of vancomycin-resistant enterococci. Cholestyramine and colestipol have shown some efficacy in binding toxins but lack established benefits. Corticosteroids may help relieve symptoms, but antidiarrheal agents can worsen the condition.
Infection control measures are crucial in institutional settings, although previous outbreaks have shown that educational and cleaning efforts alone may not suffice; restricting clindamycin use was necessary to resolve one outbreak. Overall, while patients in hospitals are at risk for C. difficile infection, they typically become vulnerable only after exposure to anti-infective therapy.

Dermatologic and Sensitivity Reactions
Generalized mild to moderate morbilliform rash is the most frequently reported adverse reaction to clindamycin. Maculopapular rash, urticaria, pruritus, fever, hypotension, and rarely polyarthritis have also occurred. A few anaphylactoid reactions have been reported in patients receiving clindamycin. Rarely, erythema multiforme, sometimes resembling Stevens-Johnson syndrome, has occurred with the drug.
Local Effects
Thrombophlebitis, erythema, and pain and swelling have occurred with IV administration of clindamycin. IM administration of clindamycin has caused pain, induration, sterile abscess, and reversible increases in serum creatine kinase (CK, creatine phosphokinase, CPK) concentrations. Local reactions can be minimized by giving deep IM injections or avoiding the prolonged use of indwelling IV catheters.
Other Adverse Effects
Other reported adverse effects of clindamycin include transient increases in serum bilirubin, alkaline phosphatase, and AST (SGOT) concentrations; transient leukopenia; neutropenia; eosinophilia; thrombocytopenia; and agranulocytosis.
The relationship of liver function and hematologic abnormalities to clindamycin is not known. Polyarthritis has been reported rarely, and rare occurrences of cardiopulmonary arrest and hypotension have been reported following too rapid IV administration of the drug. Although renal damage has not been directly attributed to clindamycin, renal dysfunction manifested as azotemia, oliguria, and/or proteinuria has been observed rarely in patients receiving the drug. Polyarthritis also has been reported rarely with clindamycin.
Precautions and Contraindications
Clindamycin therapy requires careful monitoring, mainly if diarrhea occurs, as it may indicate severe conditions like pseudomembranous colitis. If diarrhea is clinically significant or persistent, discontinuing the drug is advised, with alternative treatments considered. Older patients with severe illnesses may experience more severe effects and should be closely observed for bowel changes.
Routine tests for liver and renal function and blood cell counts are recommended during prolonged use of clindamycin due to the potential overgrowth of nonsusceptible organisms, particularly fungi. Patients with preexisting Candida infections should receive antifungal treatment concurrently. In cases of hypersensitive reactions, clindamycin should be stopped immediately and appropriate therapies initiated.
The capsules of Cleocin contain tartrazine, which can cause allergic reactions in sensitive individuals. Caution is advised for patients with a history of gastrointestinal diseases and those with severe renal or hepatic impairment, where serum concentrations should be monitored. Clindamycin is contraindicated in individuals with hypersensitivity to it or lincomycin. It is unsuitable for treating CNS infections due to inadequate distribution in the central nervous system.
Pediatric Precautions
When clindamycin is administered to pediatric patients 16 years of age, organ system functions should be monitored.
Each mL of clindamycin phosphate injection contains 9.45 mg of benzyl alcohol. Although a causal relationship has not been established, administration of injections preserved with benzyl alcohol has been associated with toxicity in neonates. Toxicity has resulted from the administration of large amounts (i.e., about 100-400 mg/kg daily) of benzyl alcohol in these neonates. Although the use of drugs preserved with benzyl alcohol should be avoided in neonates whenever possible, the American Academy of Pediatrics (AAP) states that the presence of small amounts of the preservative in a commercially available injection should not proscribe its use when indicated in neonates.

Geriatric Precautions
Clinical studies of clindamycin did not include sufficient numbers of patients 65 years and older to determine whether geriatric patients respond differently from younger patients. Clinical experience indicates that C. difficile-associated diarrhea and colitis seen in association with anti-infective agent therapy may occur more frequently and be more severe in geriatric patients (i.e., patients older than 60 years of age).
Therefore, geriatric patients receiving clindamycin should be carefully monitored for the development of diarrhea (e.g., changes in bowel frequency). Studies have not revealed any clinically important differences in oral or parenteral clindamycin pharmacokinetics between younger adults and geriatric patients with normal hepatic function and normal (age-adjusted) renal function.
Pregnancy, Fertility and Lactation
Clindamycin’s safety during pregnancy is not fully established, as there are no adequate controlled studies in pregnant women. Animal studies have shown no significant fetal harm at high doses. However, a specific mouse strain exhibited cleft palates, which other strains or species did not observe. Therefore, clindamycin should only be used in pregnancy when needed, as animal studies do not always predict human outcomes.
The CDC recommends screening and treating bacterial vaginosis (BV) in pregnant women when clinically indicated. For those at high risk of complications from BV, a 7-day regimen of either oral metronidazole or clindamycin is advised to reduce adverse pregnancy outcomes, such as preterm birth. Fertility studies in rats indicate that clindamycin does not impair fertility or mating ability.
Clindamycin is excreted in breast milk, with concentrations ranging from 0.7 to 3 mcg/mL after oral or intravenous administration. Due to potentially severe adverse reactions in nursing infants, the decision to continue breastfeeding while taking clindamycin should consider the drug’s importance to the mother.
Resistance
Staphylococcal resistance to clindamycin has been induced in vitro and is acquired stepwise. Natural and acquired resistance to the antibiotic has been demonstrated in vitro and in vivo in strains of staphylococci, streptococci, and B. fragilis. Complete cross-resistance occurs between clindamycin and lincomycin, and there is evidence of partial cross-resistance between clindamycin and erythromycin. In vitro, bacteria resistant to erythromycin and susceptible to clindamycin may exhibit a dissociated type of resistance to clindamycin during susceptibility testing if erythromycin is also present. This phenomenon may result from competition between erythromycin and clindamycin for the ribosomal binding site.
Acute Toxicity
The manufacturer does not report any information to date on overdosage of clindamycin in humans. Convulsions, depression, and death have been reported in mice receiving IV administration of 855-mg/kg doses of clindamycin; death has been reported in rats receiving oral or subcutaneous administration of 2618-mg/kg doses of clindamycin. Clindamycin is not removed by hemodialysis or peritoneal dialysis.
Drug Interactions
Neuromuscular Blocking Agents
Clindamycin has been shown to have neuromuscular blocking properties that may enhance the neuromuscular blocking action of other agents (e.g., ether, tubocurarine, pancuronium). Clindamycin should be used cautiously in patients receiving such agents, and such patients should be observed for prolongation of neuromuscular blockade.
Aminoglycosides
Clindamycin has been reported to antagonize the bactericidal activity of aminoglycosides in vitro, and some clinicians recommend that these drugs not be used concomitantly. However, in vivo antagonism has not been demonstrated, and clindamycin has been administered successfully in conjunction with an aminoglycoside with no apparent decrease in activity.
More information on indications, dosage, side effects, interactions, and contraindications can be found here. The information is provided by the FDA.
Other Brand Names and Forms of Clindamycin
| Dosage forms of Clindamycin: | |||
|---|---|---|---|
| Apo-Clindamycin 300 mg Capsule | Mylan-Clindamycin 300 mg Capsule | Novo-Clindamycin 300 mg Capsule | Dalacin C 150 mg Capsule |
| Clindets 1% pledgets | Clindamycin hcl 150 mg capsule | Clindamycin 2% vaginal cream | Clindamax 2% vaginal cream |
| Clindamycin ph 300 mg/2 ml vial | Cleocin t 1% gel | Cleocin phos 150 mg/ml vial | Cleocin 2% vaginal cream |
| Clindamycin 150 mg/ml addvan | Dalacin C 300 mg Capsule | Cleocin hcl 75 mg capsule | Cleocin hcl 150 mg capsule |
| Clindamycin (60 & 120 Ml) 150 mg/ml | Clindamycin 150 mg/ml | Clindamycin phosphate 1% foam | Clindamycin hcl 300 mg capsule |
| Dalacin C Phosphate 150 mg/ml | Cleocin 150 mg capsule | Clindagel 1% gel | Evoclin 1% foam |
| Clindamycin phos crystals | Cleocin hcl 300 mg capsule | Clindamycin Phosphate 1% Solution 30ml Bottle | Clindamycin phosphate powdr |
| Clindamycin Phosphate 1% Solution 60ml Bottle | Clindamycin Phosphate 1% Gel 30 gm Tube | Clindesse 2% vaginal cream | Clindamycin Phosphate 1% Lotion 60ml Bottle |
| Clindamycin Phosphate 60 1% Swab Box | Clindamycin Phosphate 2% Cream 40 gm Tube | Cleocin-T 1% Gel 30 gm Tube | Cleocin-T 1% Solution 60ml Bottle |
| Clindamycin Phosphate 1% Gel 60 gm Tube | Clindamycin hcl crystals | Cleocin 75 mg/5ml Solution 100ml Bottle | Cleocin 3 100 mg Suppository Box |
| Cleocin 2% Cream 40 gm Tube | Cleocin-T 60 1% Swab Box | Cleocin-T 1% Lotion 60ml Bottle | Cleocin-T 1% Gel 60 gm Tube |
| Clindamycin Phos-Benzoyl Perox 1-5% Gel 50 gm Jar | Clindamycin Phosphate 1% Foam 50 gm Can | Clindagel 1% Gel 40ml Bottle | Evoclin 1% Foam 50 gm Can |
| Clindamycin Phosphate 1% Foam 100 gm Can | Evoclin 1% Foam 100 gm Can | Clindagel 1% Gel 75ml Bottle | Dalacin C Palmitate 15 mg/ml Solution |
| Cleocin 600 mg-d5w-galaxy | Cleocin 900 mg-d5w-galaxy | Clinda-derm 1% solution | Apo-Clindamycin 150 mg Capsule |
| Mylan-Clindamycin 150 mg Capsule | Novo-Clindamycin 150 mg Capsule | Clindamycin ph 9 g/60 ml vial | |
Delivery
Australia, Canada, Mexico, New Zealand, USA, Europe [Belgium, France, Norway, Holland, Ireland, Spain, Switzerland, Great Britain (UK), Italy] and etc.
Preparations
| Product Name | Dosage | Formulation | Brand | Manufacturer |
|---|---|---|---|---|
| Clindamycin Hydrochloride Oral Capsules | 75 mg (of clindamycin) | Oral Capsules | Cleocin HCl® | Pfizer |
| Clindamycin Hydrochloride Oral Capsules | 150 mg (of clindamycin) | Oral Capsules | Cleocin HCl® | Pfizer |
| Clindamycin Hydrochloride Oral Capsules | 300 mg (of clindamycin) | Oral Capsules | Cleocin HCl® | Pfizer |
| Clindamycin Palmitate Hydrochloride | 75 mg (of clindamycin) per 5 mL | Oral solution | Cleocin Pediatric® | Pfizer |
| Clindamycin Phosphate Parenteral Injection | 150 mg (of clindamycin) per mL | Injection | Cleocin Phosphate® | Pfizer |
| Clindamycin Phosphate Parenteral Injection | 9 g (150 mg/mL) | Pharmacy bulk package | Cleocin Phosphate® | Pfizer |
| Clindamycin Phosphate Injection | N/A | Injection (IV) | Cleocin Phosphate® | AstraZeneca |
| Clindamycin Phosphate ADD-infusion | 150 mg (of clindamycin) per mL | Injection (IV) | Vantage® | Hospira |
| Clindamycin Phosphate ADD | 150 mg (of clindamycin) per mL | Injection (IV) | Vantage® | Pfizer |
| Clindamycin Phosphate in Dextrose Parenteral Injection | 6 mg (of clindamycin) per mL | IV infusion in 5% Dextrose | Cleocin Phosphate® IV | Pfizer |
| Clindamycin Phosphate in Dextrose Parenteral Injection | 12 mg (of clindamycin) per mL | IV infusion in 5% Dextrose | Cleocin Phosphate® IV | Pfizer |
| Clindamycin Phosphate in Dextrose Parenteral Injection | 18 mg (of clindamycin) per mL | IV infusion in 5% Dextrose | Cleocin Phosphate® IV | Pfizer |


 (9 votes, average: 4.11 out of 5)
(9 votes, average: 4.11 out of 5)