Drug Nomenclature
Pharmacopoeias in China, Europe, and US
European Pharmacopoeia
A white, or almost white, crystalline powder or colourless crystals. Freely soluble in water; soluble in alcohol and in dichloromethane. Protect from light.
The United States Pharmacopeia
Colourless, practically odourless, lustrous crystals or white crystalline powder. Soluble 1 in 1.5 of water, 1 in 12.5 of alcohol, 1 in 10 of chloroform, and 1 in 320 of ether. Its solutions are alkaline to litmus.
Methenamine Hippurate
Drug Nomenclature
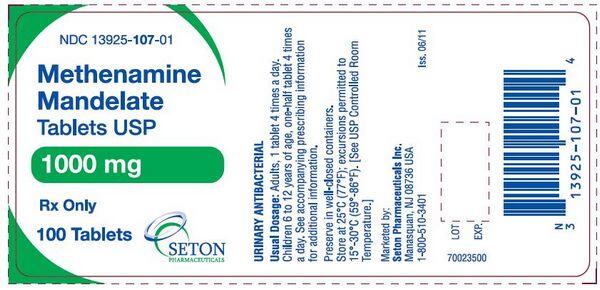
Methenamine Mandelate
Drug Nomenclature
The United States Pharmacopeia
A white, practically odourless crystalline powder. Very soluble in water; soluble 1 in 10 of alcohol, 1 in 20 of chloroform, and 1 in 350 of ether. Its solutions have a pH of about 4.

Adverse Effects and Precautions
Methenamine and its salts are generally well tolerated but may cause gastrointestinal disturbances such as nausea, vomiting, and diarrhoea. Skin rashes, pruritus, and occasionally other hyper-sensitivity reactions, may occur. Comparatively large amounts of formaldehyde may be formed during prolonged use or when large doses are given.
This may produce irritation and inflammation of the urinary tract, especially the bladder, as well as painful and frequent micturition, haematuria, and proteinuria.
The effect of the formaldehyde may be reduced by alkalinising drugs, such as sodium bicarbonate, or large quantities of water, but it is then less effective. Methenamine and its salts are contra-indicated in patients with hepatic impairment because of the liberation of ammonia in the gastrointestinal tract.
Although methenamine itself is not contra-indicated in renal impairment, its salts should be avoided in severe impairment because of the risk of mandelate or hippurate crystalluria.
They should also be avoided in patients with severe dehydration, metabolic acidosis, or gout. Interference with laboratory estimations for catecholamines, 17-hydroxycorticosteroids, and oestrogens in the urine has been reported.
Interactions
The use of drugs that alkalinise the urine, including some antacids, potassium citrate, and diuretics such as acetazolamide or the thiazides, should be avoided because the activation of methenamine to formaldehyde may be inhibited (but see above). Use of methenamine with sulfonamides may increase the risk of crystalluria since methenamine requires low urinary pH for its effect, at which sulfonamides and their metabolites are poorly soluble; methenamine may also form poorly soluble compounds with some sulfonamides.
Antimicrobial Action
Methenamine owes its antibacterial properties to formaldehyde, a non-specific bactericide, which is slowly liberated by hydrolysis at acid pH. Most Gram-positive and Gram-negative organisms and fungi are susceptible. Hippuric and mandelic acids have some antibacterial activity in vitro, but their contribution to the antibacterial action of the salts in vivo, beyond assisting the maintenance of low urinary pH, is uncertain. Urea-splitting organisms such as Proteus and some Pseudomonas spp. tend to increase urinary pH and inhibit the release of formaldehyde, thereby decreasing the effectiveness of methenamine. Use with acetohydroxamic acid, a potent inhibitor of bacterial urease, has been suggested for urinary infections due to these organisms. True resistance to formaldehyde does not appear to be a problem in clinical use.
Pharmacokinetics
Methenamine is readily absorbed from the gastrointestinal tract and widely distributed in the body. Under acid conditions methenamine is slowly hydrolysed to formaldehyde and ammonia: about 10 to 30% of an oral dose may be converted in the stomach unless it is given as an enteric-coated preparation. Almost no hydrolysis of methenamine takes place at physiological pH, and it is therefore virtually inactive in the body. The half-life is reported to be about 4 hours. Methenamine is rapidly and almost completely eliminated in the urine, and provided this is acidic (preferably below pH 5.5) bactericidal concentrations of formaldehyde are achieved. Because of the time taken for hydrolysis, however, these are not achieved until the urine reaches the bladder, with peak concentrations occurring up to 2 hours after an oral dose. Absorption, and hence excretion, may be somewhat delayed in patients given enteric-coated formulations. Methenamine crosses the placenta and small amounts may be distributed into breast milk. The mandelate and hippurate moieties are also rapidly absorbed and are excreted in urine by tubular secretion as well as glomerular filtration.
Uses and Administration
Methenamine is used, usually as the hippurate or mandelate, in the prophylaxis and treatment of chronic or recurrent, uncomplicated, lower urinary-tract infections and asymptomatic bacteriuria. It has been considered suitable for long-term use because acquired resistance does not appear to develop. Methenamine and its salts should not be used in upper urinary-tract infections because it is eliminated too rapidly to exert an effect, nor in acute urinary infections. It is only active in acidic urine, when formaldehyde is released, and although hippuric or mandelic acid helps to acidify the urine, ammonium chloride or ascorbic acid may be tried. If urea-splitting bacteria such as Proteus or some Pseudomonas spp. are present they may produce so much ammonia that the urine cannot be acidified (see also Antimicrobial Action, above). The usual oral adult dose of methenamine or methenamine man-delate is 1 g given four times daily. Methenamine hippurate is given orally in a usual dose of 1 g twice daily; the dose may be increased to three times daily in catheterised patients. For details of doses in children, see below. Methenamine has been used topically in deodorant preparations, since in the presence of acid sweat it liberates formaldehyde. Methenamine calcium thiocyanate has been used in combination preparations for upper respiratory-tract disorders.
Administration in children
In the US or USA, the usual recommended oral dose of methenamine mandelate in children up to 6 years old is about 18 mg/kg given four times daily; those aged 6 to 12 years may be given methenamine or methenamine mandelate 500 mg four times daily. In the UK, methenamine hippurate may be given in a usual oral dose of 500 mg twice daily in children aged 6 to 12 years. Doses of up to 1 g twice daily have been given in the US.
Preparations
The United States Pharmacopeia 31, 2008: Methenamine Elixir; Methenamine Hippurate Tablets; Methenamine Mandelate Delayedre lease Tablets; Methenamine Mandelate for Oral Solution; Methenamine Mandelate Oral Suspension; Methenamine Mandelate Tablets; Methenamine Tablets.
Proprietary Preparations
Australia: Hiprex; Austria: Hiprex; Belgium: Hiprex; Canada: Dehydral; Hiprex; Manclelamine; Urasal; Denmark: Geasaloll; Haiprex; Finland: Hipeksal; Hiprex; Germany:; Antihydral; Urotractan; Ireland: Hiprex; Israel: Hiprex; Mexico: Bioran; Netherlands: Reflux; Norway: Hiprex; New Zealand: Hiprex; Philippines: Hiprex; Poland: Stoppot; South Africa: Hippramine; Mandelamine; Sweden: Hiprex; Switzerland: Antihydral; Turkey: Helpa; Hippurin; Manuprin; Neturone; Purinol; Uron; United Kingdom (UK): Hiprex; United States of America (US or USA): Hiprex; Mandelamine; Urex; Venezuela: Mandelamine.
Multi-ingredient
Argentina: Calculina Belgium: Carbobel; Mictasol; Mictasoll; Brazil: Abacateiroh; Acridin; Cystex; Sepurin; Urodonall; Chile: Uroknop; France: Mictasol; Pedi-Relax Anti-Transpirant; Germany; Antihydral MI; Hong Kong; Antihydral M; Hungary: Bilagit; Mexico: Furanton; Poland: Dezorol; Pedipur; Urosal; Turkey: Helmobleu; US: Atrosept; Cystex; Dolsedl; MHP-A; MSP-Blu; Prosed/DS; Trac Tabs 2X; UAA; Urelle; Uretron; Uridon Modified; Urimar; Urimax; Urised; Uriseptic; UriSym; Uritact; Uro Blue; Urogesic Blue; Utira; Venezuela: Azo-Mandelamine.

