Drug Nomenclature
International Nonproprietary Names (INNs) in main languages (French, Latin, Russian, and Spanish):
Adverse Effects
Diarrhoea and other gastrointestinal disturbances such as nausea, vomiting, abdominal pain, and flatulence are among the most common adverse reactions after use of telithromycin. Severe, but usually reversible, hepatic dysfunction, including elevation of liver enzymes and hepatitis, with or without jaundice has been reported; however, there have been cases of fatal hepatotoxicity including fulminant hepatitis, hepatic necrosis, and hepatic failure.
Effects on the CNS may include dizziness, headache, vertigo, and, occasionally, insomnia or drowsiness. Taste, and very rarely smell, disturbances may occur. Other less commonly reported adverse effects include paraesthesia, eosinophilia, skin rashes, and cardiovascular effects such as arrhythmias, hypotension, and bradycardia. Visual disturbances, particularly affecting accommodation, have occurred. Syncope, usually associated with the vagal syndrome, has been noted. Very rarely reported adverse effects include angioedema and anaphylaxis.
There have been isolated cases of erythema multiforme, pseudomem-branous colitis, and muscle cramps. Life-threatening acute respiratory failure has been reported in patients with myasthenia gravis (see also Precautions, below).
Effects on the eyes
Visual disturbances, namely blurred vision, difficulty with focusing, and diplopia have been associated with telithromycin. These have been reported to be more common in females under the age of 40 years and to occur in 1.1 % of patients compared with 0.28% in those receiving a comparable antibacterial. Licensed product information reports that symptoms are fully reversible, mostly mild to moderate in severity, and typically occur within a few hours of the first or second dose, lasting for several hours and recurring upon subsequent dosing. They have not been associated with any ocular abnormality.
Effects on the kidneys
Acute interstitial nephritis has been reported in an 18-year-old man who received telithromycin for 5 days. Complete recovery of renal function occurred 2 weeks after starting symptomatic treatment with methylprednisolone.
Effects on the liver
Hepatotoxicity is an established adverse effect of telithromycin and may be severe. Of 3 case reports of serious liver toxicity in patients with no pre-existing hepatic impairment, after receiving telithromycin at the usual dose, one patient spontaneously recovered, one required a liver transplant, and one died.
Effects on the skin
A 26-year-old woman with a history of rash to penicillin and sulfonamides developed toxic epidermal necrolysis after 13 doses of oral telithromycin for treatment of sinusitis; she was discharged 4 weeks after admission to hospital but had scars on her face and body and had lost her eyelashes.
Precautions
Telithromycin should not be given to patients with known hypersensitivity to it or to the macrolides; similarly, a history of hepatitis and/or jaundice associated with telithromycin or macrolides is a contra-indication. Telithromycin is contra-indicated in patients with myasthenia gravis because it may exacerbate symptoms of the disease; exacerbations usually occur within 1 to 3 hours of the first dose.
Fatalities have been reported.
Patients with a congenital or family history of QT interval prolongation should not receive telithromycin; it should be used with care in those with coronary heart disease, cardiac arrhythmias, and in those with hypo-kalaemia or hypomagnesaemia, due to its potential to prolong the QT interval. Certain medications may also increase the risk of cardiac arrhythmias and prolong the QT interval (see Interactions, below).
Patients should be informed about signs and symptoms of hepatitis. Should any of these develop during treatment with telithromycin, they should stop taking the drug and consult their doctor. It should be used with caution in patients with hepatic impairment; however, this is based on limited data in such patients.
Reduced doses may be necessary in those with severe renal impairment (see below). Since telithromycin can produce visual disturbances or loss of consciousness caution is advised when driving, operating machinery or undertaking similar hazardous activities.
Breast feeding
Telithromycin has been shown to be excreted in the milk of lactating animals at concentrations about 5 times greater than those in maternal plasma, although corresponding data for humans is not available.
Pregnancy
Reproductive toxicity, but not teratogenicity, has been seen in animals; the potential risk for humans is unknown.
Interactions
Telithromycin is an inhibitor of the cytochrome P450 isoenzymes CYP3A4 and CYP2D6. Although there have been few clinical reports, drug interactions with telithromycin may be expected to be similar to those seen with erythromycin. In particular, caution is required when telithromycin is given with drugs that may prolong the QT interval. Use of telithromycin with cisapride, ergot alkaloid derivatives, pimozide, astemizole, or terfenadine is usually contra-indicated.
Caution is usually necessary with benzodiazepines such as alprazolam, midazolam, and triazolam, and with metoprolol. T
elithromycin should not be given with drugs that induce the cytochrome P450 isoenzyme CYP3A4, such as rifampicin, phenytoin, carbamazepine, or St John’s wort. Telithromycin increases plasma concentrations of some statins and hence the risk of myopathy; it should not be given with atorvastatin, lovastatin, or simvastatin.
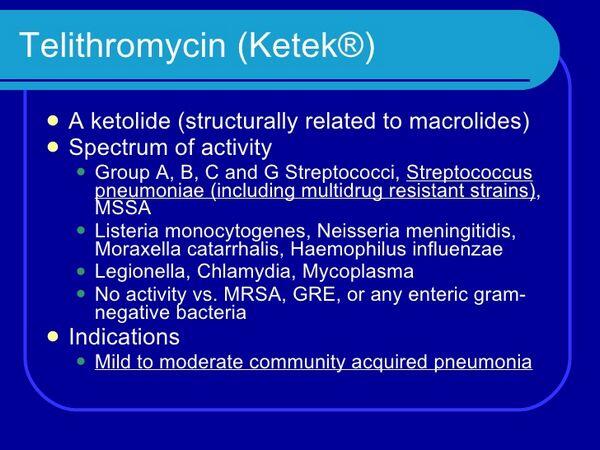
Antimicrobial Action
Telithromycin is a ketolide antibacterial with a bactericidal action and is highly active against certain Gram-positive bacteria, including multidrug-resistant strains of Streptococcus pneumoniae. Some strains of Streptococcus pyogenes and of Staphylococcus aureus are also sensitive. Telithromycin also shows good activity against the Gram-negative organisms Haemophilus influenzae and Moraxella catarrhalis (Branhamella catarrhalis).
Activity against Mycoplasma pneumoniae and Chlamydophila pneumoniae (Chlamydia pneumoniae) is comparable with macrolides, and it shows greater activity than erythromycin and roxithromycin against Legionella spp. Mycobacterium spp. are reported to be moderately susceptible. Enterobacteriaceae, Pseudomonas spp., and Acinetobacter spp. are not susceptible.
Pharmacokinetics
Telithromycin is rapidly absorbed after an oral dose, with a bioavailability of 57%. Peak plasma concentrations of about 2 micrograms/mL are reached around 1 to 3 hours after a dose of 800 mg. Food does not affect the absorption of telithromycin. Telithromycin is widely distributed in body fluids and tissues, including those of the respiratory tract, and plasma protein binding is 60 to 70%.
Concentrations in target tissues are reported to be higher than plasma concentrations, suggesting the drug may remain active when the plasma concentration has fallen below the MIC About two-thirds of a dose is metabolised in the liver to inactive metabolites and the remaining third is eliminated unchanged in the urine and faeces. Metabolism is mediated both by cytochrome P450 isoenzymes (mainly CYP3A4) and non-cytochrome P450 enzymes. The pharmacokinetics of telithromycin are triphasic with a biphasic elimination phase; the elimination half-life is 2 to 3 hours and the terminal half-life about 10 hours. Distribution into milk has been found in studies in animals.
Uses and Administration
Telithromycin is a ketolide antibacterial used for the treatment of susceptible respiratory-tract infections in adults including mild to moderate community-acquired pneumonia. In some countries it is also licensed for use in the treatment of acute sinusitis and acute bacterial exacerbations of chronic bronchitis when resistance to beta-lactam and/or macrolide antibacterials is known or suspected; and as an alternative to beta-lactam antibacterials for tonsillitis or pharyngitis caused by Group A beta streptococci in patients over 12 years of age. It is given orally in a usual dose of 800 mg once daily. Doses may need to be reduced in patients with renal impairment (see below).
Administration in renal impairment
Doses of telithromycin should be reduced in severe renal impairment (creatinine clearance of less than 30 mL/mfnute):
- UK licensed product information states that alternating daily doses of 800 mg and 400 mg, starting with 800 mg may be given whether or not hepatic function is also impaired
- US licensed product information recommends a dose of 600 mg once daily if there is no hepatic impairment but a dose of 400 mg once daily if there is co-existing impairment
Doses should be given after dialysis sessions to patients on haemodialysis.
Respiratory disorders
As well as their established antibacterial effect, it has been suggested that macrolides also have immunomodulatory effects that could be useful in the management of respiratory diseases (see also Respiratory Disorders, under Uses of Erythromycin). Ketolides also appear to have such effects: a 10-day course of oral telithromycin 800 mg daily, started with standard treatment for acute asthma in adults, was reported to improve asthma symptoms regardless of infection with Chlamydophila pneumoniae (Chlamydia pneumoniae) or Mycoplasma pneumoniae The mechanism of this effect is unclear, however, and further studies are needed.
Single-ingredient Preparations
Argentina: Ketek; Belgium: Ketek; Brazil: Ketek; Canada: Ketek; Chile: Ketek; Finland: Ketek; France: Ketek; Germany: Ketek; Greece: Ketek; Ireland: Ketek; Italy: Ketek; Japan: Ketek; Mexico: Ketek; Norway: Ketek; Leviax; Portugal: Ketek; South Africa: Ketek; Spain: Ketek; Levviax; Sweden: Ketek; United Kingdom: Ketek; United States: Ketek; Venezuela: Ketek

