IV vancomycin hydrochloride is used in the treatment of potentially life-threatening infections caused by susceptible organisms which cannot be treated with other effective, less toxic anti-infective agents. Vancomycin is used principally for the treatment of severe infections caused by gram-positive bacteria in patients who cannot receive or who have failed to respond to penicillins and cephalosporins or for the treatment of gram-positive bacterial infections that are resistant to b-lactams and other anti-infectives.
Drug Use
Guidelines for the Prevention of Vancomycin Resistance Use of, and exposure to, anti-infectives are major risk factors for the emergence of anti-infective-resistant pathogens, and anti-infective resistance results in increased morbidity, mortality, and healthcare costs.
Prevention of the emergence of drug resistance, its dissemination among pathogens, and the spread of such pathogens has become an increasingly important public health problem. Medical, pharmacy, and other staff and individuals responsible for drug-use policy and formulary decisions should review and restrict the use of certain anti-infectives, including vancomycin, and ensure that their use is appropriate.
Clinicians should recognize that unnecessary and inappropriate use of anti-infectives has important, far-reaching implications for human health globally. Because of the rapidly increasing prevalence of vancomycin-resistant enterococci in the US and concerns regarding the possibility of vancomycin-resistant strains of other gram-positive bacteria (e.g., Staphylococcus aureus), a subcommittee of the US Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee and others have made recommendations designed to prevent the spread of vancomycin resistance.
The CDC recommends that hospitals in collaboration with quality improvement and infection control programs, pharmacy and therapeutics committees, and clinical, microbiology, nursing, administrative, and housekeeping departments develop comprehensive, institution-specific strategic plans for the detection, prevention, and control of infection and colonization with vancomycin-resistant enterococci and other bacterial pathogens.
Since vancomycin use has consistently been reported to be a risk factor for colonization and infection with vancomycin-resistant enterococci, these strategic plans should include recommendations for the prudent use of vancomycin. In addition, all hospitals and other health-care delivery services (even those that have not had reports of vancomycin-resistant enterococci) should develop a comprehensive antimicrobial-utilization plan to provide education for their medical staff and medical students, oversee surgical prophylaxis, and develop guidelines for the appropriate use of vancomycin as applicable to their particular institution. Continuing education programs for hospital staff (e.g., attending and consulting physicians, medical students and residents, personnel in pharmacy, nursing, and laboratory departments) should include information on the epidemiology of vancomycin-resistant enterococci and the potential impact on cost and outcome of patient care. Enterococcal isolates obtained from blood, sterile body sites (with the possible exception of sterile urine), and other sites as clinically indicated should be evaluated for vancomycin resistance and high-level resistance to penicillin (or ampicillin) and aminoglycosides. If resources permit, laboratories may choose to routinely test wound and urine isolates for resistance to vancomycin, penicillin, and ampicillin
Patients with vancomycin-resistant Enterococcus faecium (VREF) or staphylococcal infections that have not responded to appropriate anti-infective therapy or in whom vancomycin-resistant strains are suspected or documented may be candidates for treatment with linezolid (Zyvox®) or the fixed combination of quinupristin and dalfopristin (Synercid®). Linezolid may be active against vancomycin-resistant E. faecalis, but quinupristin and dalfopristin is not active against E. faecalis, and enterococcal species differentiation is important to avoid misidentification of this organism.
Based on recent reports of staphylococci, including MRSA, with reduced susceptibility to vancomycin and concerns about the possible appearance of staphylococci highly resistant to vancomycin,the CDC Hospital Infection Control Practices Advisory Committee also has issued interim guidelines designed to prevent and control the spread of infection caused by such strains.
The interim guidelines include steps to decrease the likelihood of emergence of staphylococci with reduced susceptibility to vancomycin (e.g., limiting overuse and misuse of vancomycin), information on how to identify strains with reduced susceptibility to vancomycin (see Spectrum: In Vitro Susceptibility Testing), information on how to obtain an investigational antistaphylococcal anti-infective agent if use of such an agent is considered necessary (see Uses: Staphylococcal Infections), and information on infection control measures that should be used to prevent the spread of such strains within and between facilities and minimize the potential for the organism to become endemic.
The CDC recommends that vancomycin be reserved for use in the treatment of serious infections caused by gram-positive bacteria resistant to b-lactam anti-infectives; treatment of gram-positive bacterial infections in patients with severe hypersensitivity to b-lactam anti-infectives; prophylaxis in certain patients at high risk for bacterial endocarditis as recommended by the American Heart Association (AHA); treatment of antibiotic-associated pseudomembranous colitis that is severe or potentially life-threatening or that fails to respond to oral metronidazole; and for perioperative prophylaxis for major surgical procedures involving implantation of prosthetic materials or devices (e.g., cardiac and vascular procedures and total hip replacement) at institutions with a high rate of methicillin-resistant S. aureus (MRSA) or S. epidermidis.
The CDC suggests that use of the drug in other situations be discouraged. Situation in which the use of vancomycin should be discouraged include: treatment of antibiotic-associated colitis when metronidazole would be effective; routine empiric therapy for febrile neutropenic patients, unless there is strong evidence that the infection is caused by gram-positive organisms (e.g., inflamed exit site of Hickman catheter) and the prevalence of MRSA in the hospital is substantial; continued use after results of in vitro tests indicate that an infection is not caused by gram-positive organisms resistant to b-lactam anti-infectives; selective decontamination of the GI tract; eradication of colonization with MRSA; routine prophylaxis in patients undergoing surgery, except in patients with life-threatening allergy to b-lactam anti-infectives; routine prophylaxis in patients undergoing continuous ambulatory peritoneal dialysis or hemodialysis; systemic or local (e.g., antibiotic lock) prophylaxis for infection or colonization of indwelling central or peripheral intravascular catheters; routine prophylaxis in very low birthweight neonates; use for topical application or irrigation; use for treatment of infections caused by gram-positive organisms susceptible to b-lactam anti-infectives; and use in response to a single blood culture positive for coagulase-negative staphylococci if other blood cultures drawn in the same time frame are negative (i.e., contamination of the blood culture with skin flora is likely).
Staphylococcal Infections
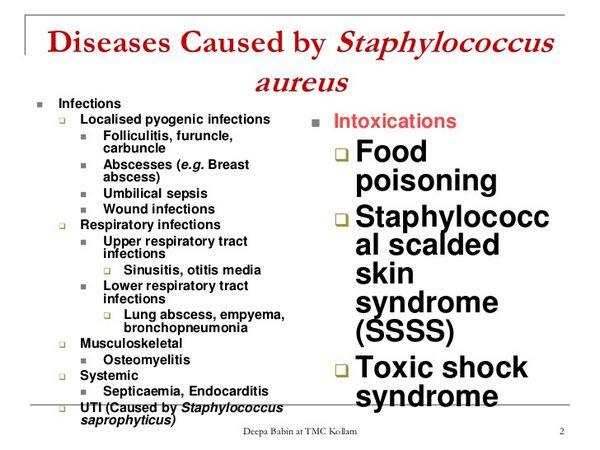
IV vancomycin has been used alone successfully in the treatment of endocarditis, osteomyelitis, pneumonia, septicemia, and soft-tissue infections caused by Staphylococcus aureus or S. epidermidis, including methicillin-resistant strains. IV vancomycin, alone or in conjunction with other anti-infectives, generally is considered the treatment of choice for infections caused by methicillin-resistant staphylococci.
Because methicillin-resistant staphylococci are being reported with increasing frequency, initial therapy for suspected staphylococcal infections should include vancomycin if methicillin-resistant strains are prevalent in the community or hospital. Patients with diabetes mellitus, peripheral vascular disease, or burn wounds appear to be at particularly high risk of acquiring MRSA, and methicillin-resistant S. epidermidis has been reported frequently in patients with prosthetic valve endocarditis or infected CSF shunts and in granulocytopenic children with cancer.
However, in a study of empiric therapy in a limited number of febrile, neutropenic cancer patients, addition of vancomycin to a regimen of ceftazidime and amikacin did not improve outcome and was associated with more frequent nephrotoxicity; it has been suggested that such vancomycin use generally be limited to patients with likely or documented gram-positive bacteremia or in institutions where gram-positive bacteremia (especially if caused by methicillin-resistant staphylococci) is common. In addition, if empiric therapy initially includes vancomycin, it generally is recommended that the drug be discontinued 3-4 days later if a fulminant gram-positive infection is not confirmed. Infections caused by MRSA or methicillin-resistant S. epidermidis generally are treated with vancomycin alone or vancomycin in conjunction with rifampin and/or an aminoglycoside.
When MRSA is suspected in patients with bacteremia or sepsis, a regimen of vancomycin with or without gentamicin and/or rifampin often is recommended. Vancomycin has been effective when given by instillation via the arteriovenous shunt for the treatment and prophylaxis of staphylococcal infections in hemodialysis patients. The drug also has been effective when given IV for the treatment of peritonitis caused by susceptible staphylococci or other gram-positive bacteria in peritoneal dialysis patients.
Vancomycin does not replace appropriate surgical measures when staphylococcal infections are localized and purulent. IV vancomycin is considered the drug of choice for the treatment of endocarditis caused by methicillin-resistant staphylococci. While a regimen of vancomycin administered alone is recommended for methicillin-resistant staphylococcal endocarditis in patients with native cardiac valves, patients with a prosthetic valve or other prosthetic material should receive a combination regimen of IV vancomycin, oral rifampin, and IV or IM gentamicin.
Patients with endocarditis caused by methicillin-susceptible staphylococci generally should receive a regimen that consists of a penicillinase-resistant penicillin (i.e., IV nafcillin or IV oxacillin) with or without IM or IV gentamicin; oral rifampin is added if a prosthetic valve or other prosthetic material is present.
Penicillin-allergic patients with methicillin-susceptible staphylococcal endocarditis who have native cardiac valves usually can receive IV cefazolin (or other parenteral first-generation cephalosporin) with or without IM or IV gentamicin unless they have a history of immediate-type penicillin hypersensitivity; IV vancomycin usually is reserved for use as an alternative agent for the treatment of patients with a history of immediate-type hypersensitivity to penicillin.
Data are limited regarding use of combination regimens in patients with a prosthetic valve or other prosthetic material who have staphylococcal endocarditis caused by methicillin-susceptible strains; however, some clinicians recommend that these patients receive a regimen of a penicillinase-resistant penicillin (i.e., IV nafcillin or IV oxacillin) with oral rifampin and IM or IV gentamicin and that a parenteral first-generation cephalosporin or IV vancomycin should be substituted for the penicillin in those who are penicillin-allergic.
Because staphylococcal isolates with reduced susceptibility to vancomycin have recently been reported in patients who received the drug, staphylococci from patients who fail to respond to vancomycin therapy should be tested to determine if resistance to the drug has developed.
Patients with staphylococcal infections that have not responded to appropriate anti-infective therapy may be candidates for treatment with quinupristin and dalfopristin (Synercid®) if the causative organism is found to have reduced susceptibility to vancomycin.
Streptococcal Infections
While a regimen of IV penicillin G (with or without IM or IV gentamicin) or a regimen of IV or IM ceftriaxone usually is recommended for the treatment of endocarditis caused by viridans streptococci or S. bovis, IV vancomycin is the regimen of choice for patients with a history of immediate-type hypersensitivity to penicillin.
For the treatment of enterococcal endocarditis, a regimen of either IV penicillin G or IV ampicillin with IM or IV gentamicin is preferred for most patients; however, a regimen of IV vancomycin with IM or IV gentamicin is considered the regimen of choice for the treatment of enterococcal endocarditis in patients with a history of immediate-type hypersensitivity to penicillins.

Vancomycin is used alone or in conjunction with a third generation cephalosporin (ceftriaxone, cefotaxime) with or without rifampin for the treatment of infections caused by Streptococcus pneumoniae that are highly resistant to penicillins. Highly penicillin-resistant S. pneumoniae also may have reduced susceptibility to third generation cephalosporins (e.g., cefotaxime, ceftriaxone). In areas where there have been reports of highly penicillin-resistant S. pneumoniae that also have reduced susceptibility to third generation cephalosporins, the CDC and many clinicians recommend use of vancomycin (with or without rifampin) in conjunction with a third generation cephalosporin (e.g., cefotaxime, ceftriaxone) for empiric treatment of severe, life-threatening infections (e.g., meningitis) pending results of in vitro susceptibility tests. Vancomycin should be discontinued if the causative organism is found to be susceptible to the cephalosporin.
Vancomycin has been used in conjunction with rifampin for the treatment of pneumococcal meningitis in patients hypersensitive to penicillins. There is evidence that vancomycin used alone may not achieve effective CSF concentrations in some patients, and the drug should not be used alone for the treatment of pneumococcal meningitis. Although vancomycin has been administered intrathecally for the treatment of meningitis caused by susceptible organisms, the manufacturers state that safety and efficacy of intrathecal (intralumbar or intraventricular) administration have not been determined.
Bacterial Endocarditis
IV vancomycin is used for the treatment of bacterial endocarditis and for prevention of bacterial endocarditis.
Treatment
IV vancomycin is used for the treatment of endocarditis caused by S. aureus or S. epidermidis, including methicillin-resistant strains, and is considered the drug of choice for the treatment of endocarditis caused by methicillin-resistant staphylococci. (See Uses: Staphylococcal Infections.) IV vancomycin also is used for the treatment of endocarditis caused by viridans streptococci or S. bovis in patients with a history of immediate-type hypersensitivity to penicillin.Vancomycin also has been reported to be effective for the treatment of diphtheroid endocarditis.
Prevention
IV vancomycin is used as an alternative agent for prevention of enterococcal endocarditis in penicillin-allergic adults and children with congenital heart disease, rheumatic or other acquired valvular heart dysfunction (even after valvular surgery), prosthetic heart valves (including bioprosthetic and allograft valves), surgically constructed systemic pulmonary shunts or conduits, hypertrophic cardiomyopathy, mitral valve prolapse with valvular regurgitation and/or thickened leaflets, or previous bacterial endocarditis (even in the absence of heart disease), who undergo certain GI, biliary tract, or genitourinary surgery or instrumentation likely to cause transient bacteremia and increase the risk of endocarditis.
These procedures include sclerotherapy for esophageal varices; esophageal structure dilation; endoscopic retrograde cholangiography with biliary obstruction, biliary tract surgery; surgical operations that involve intestinal mucosa; prostatic surgery, cystoscopy; and urethral dilation.
The American Heart Association (AHA) recognizes that its current recommendations for prophylaxis against bacterial endocarditis are empiric, since no controlled efficacy studies have been published, and that prophylaxis of endocarditis is not always effective. However, the AHA generally recommends routine use of prophylactic anti-infectives in patients with the cardiac conditions described above since these are associated with a high or moderate risk for bacterial endocarditis. Prophylaxis against bacterial endocarditis is not considered necessary for adults or children with cardiac conditions considered to be associated with a negligible risk for endocarditis since these individuals are at no greater risk than the general population.
Therefore, prophylaxis against bacterial endocarditis is not considered necessary for individuals with a history of isolated secundum atrial septal defect; surgical repair of atrial septal defect, ventricular septal defect, or patent ductus arteriosus (without residua beyond 6 months); previous coronary artery bypass graft surgery; mitral valve prolapse without valvar regurgitation; physiologic, functional, or innocent heart murmurs; previous Kawasaki disease without valvar dysfunction; previous rheumatic fever without valvar dysfunction; or cardiac pacemaker (intravascular and epicardial) and implanted defibrillators. When selecting anti-infectives for prophylaxis of bacterial endocarditis, the current recommendations of the AHA should be consulted.
Enterocolitis and Clostridium difficile-associated Diarrhea and Colitis
Although vancomycin hydrochloride is not effective by the oral route for the treatment of systemic infections, the drug may be given orally for the treatment of enterocolitis caused by Staphylococcus aureus (including methicillin-resistant strains) or for Clostridium difficile-associated diarrhea and colitis (CDAD; also known as antibiotic-associated diarrhea and colitis, C. difficile diarrhea, C. difficile colitis, and pseudomembranous colitis); parenteral antibiotic administration may be given concomitantly.
Some clinicians believe that vancomycin hydrochloride is the drug of choice for staphylococcal enterocolitis because it does not affect the normal coliform bacteria present in the GI tract.
Oral vancomycin is used for the treatment of C. difficile-associated diarrhea and colitis, particularly in severe cases.
Fever may resolve within 24-48 hours and diarrhea generally remits gradually over about 3-5 days after initiation of oral vancomycin therapy; however, resolution of fever and diarrhea occasionally may take a week or longer, probably because of persistent inflammation despite cessation of toxin production. Relapse, which usually is apparent within several weeks (occasionally up to several months) and probably is secondary to persistent germinating C. difficile spores or reinfection with the same or different strains, occurs in about 10-35% of patients treated with an effective anti-infective but generally responds to additional therapy with the same or an alternative anti-infective; true treatment failures (i.e., secondary to resistant strains) are rare.
Although oral vancomycin also has been used in combination with oral rifampin for possible synergistic or other combined activity against C. difficile and/or its spores, the role, if any, of this approach in the treatment of multiple relapses remains to be established.
Oral metronidazole appears to be as effective as oral vancomycin for the treatment of pseudomembranous colitis caused by C. difficile. Therefore, because of cost considerations and concerns about increasing enterococcal and other (e.g., staphylococcal) resistance to vancomycin (see Resistance) and the risk of selection of such strains secondary to widespread and/or injudicious use of the drug, most experts and clinicians state that oral metronidazole therapy is preferred (unless a resistant strain of C. difficile is suspected or therapy with metronidazole is contraindicated or not tolerated) when anti-infective therapy is indicated for most cases of antibiotic-associated colitis and diarrhea.
The relative efficacy of oral metronidazole for severe, potentially life-threatening cases of pseudomembranous colitis remains unclear, and some clinicians continue to consider vancomycin the drug of choice when anti-infective therapy is indicated for such cases (e.g., in critically ill patients). Most clinicians currently recommend that oral vancomycin only be used for the treatment of C. difficile-associated colitis in seriously ill patients (i.e., with severe or potentially life-threatening colitis) or those who cannot tolerate or do not respond to oral metronidazole.
Oral vancomycin or oral metronidazole also has been used to prevent nosocomial outbreaks of C. difficile diarrhea and colitis in institutionalized patients who asymptomatically harbor the organism. However, current evidence suggests that the risks of such prophylactic therapy (e.g., in selecting potentially resistant organisms such as enterococci), particularly with vancomycin, outweigh any possible benefit. Most experts currently recommend that appropriate enteric and barrier precautions (e.g., isolation of patients, private bathroom facilities, strict hygiene) rather than prophylactic anti-infective therapy be implemented to prevent nosocomial transmission of the organisms.
Respiratory Tract Infections
Although not considered a drug of choice for the treatment of community-acquired pneumonia (CAP), there may be some situations when IV vancomycin is included in anti-infective regimen used for empiric therapy of severe CAP that may be caused by S. aureus (e.g., in patients from a nursing home known to harbor this organism). In addition, use of IV vancomycin may be considered for the initial treatment of pneumonia caused by highly penicillin-resistant S. pneumoniae, especially when cephalosporins (e.g., ceftriaxone, cefotaxime) cannot be used.
Perioperative Prophylaxis
IV vancomycin is used for perioperative prophylaxis to reduce the risk of infection in patients undergoing certain cardiac, neurosurgical, orthopedic, thoracic (noncardiac), or vascular surgical procedures at institutions where MRSA or methicillin-resistant S. epidermidis are frequent causes of postoperative wound infection or for perioperative prophylaxis in patients undergoing these procedures when the drugs of first choice (cefazolin, cefuroxime) cannot be used because the patient is hypersensitive to b-lactam anti-infectives. However, routine use of vancomycin for perioperative prophylaxis is not recommended since such use may promote emergence of vancomycin-resistant enterococci or staphylococci.
Prevention of Perinatal Group B Streptococcal Disease
IV vancomycin is used as an alternative to parenteral penicillin G or ampicillin for prevention of perinatal group B streptococcal (GBS) disease in certain women who are hypersensitive to penicillin.
Pregnant women who are colonized with GBS in the genital or rectal areas can transmit GBS infection to their infants during labor and delivery resulting in invasive neonatal infection that can be associated with substantial morbidity and mortality. Intrapartum anti-infective prophylaxis for prevention of early-onset neonatal GBS disease is administered selectively to women at high risk for transmitting GBS infection to their neonates.
When intrapartum prophylaxis is indicated in the mother, penicillin G is the regimen of choice and ampicillin is the preferred alternative. When intrapartum prophylaxis to prevent GBS in the neonate is indicated in women who are hypersensitive to penicillins, the CDC recommends a regimen of IV cefazolin for those allergic to penicillins who are not at high risk for anaphylaxis. For those allergic to penicillins who are at high risk for anaphylaxis (e.g., those with a history of immediate penicillin hypersensitivity, such as anaphylaxis, angioedema, or urticaria; those with a history of asthma or other conditions that would make anaphylaxis more dangerous or difficult to treat, including individuals receiving adrenergic blocking agents), the CDC recommends a regimen of IV clindamycin or IV erythromycin.
However, the fact that S. agalactiae (group B streptococci) with in vitro resistance to clindamycin and erythromycin have been reported with increasing frequency should be considered when choosing an alternative to penicillins for these patients. In addition, strains of GBS resistant to erythromycin often are resistant to clindamycin, although this may not be evident in results of in vitro testing. When use of erythromycin or clindamycin is being considered in a women hypersensitive to penicillin, in vitro susceptibility testing of clinical isolates obtained during GBS prenatal screening should be performed whenever possible to determine if the isolates are susceptible to these drugs. If in vitro susceptibility testing is not possible, results are unknown, or isolates are found to be resistant to erythromycin or clindamycin, a regimen of vancomycin should be used for intrapartum prophylaxis in women with penicillin allergy who are at high risk for anaphylaxis.
Empiric Therapy in Febrile Neutropenic Patients
IV vancomycin is used in conjunction with 1 or 2 other anti-infectives for empiric anti-infective therapy of presumed bacterial infections in febrile neutropenic patients. Vancomycin should never be used alone for empiric therapy in febrile neutropenic patients. Some clinicians suggest that it may be prudent to include vancomycin in an initial empiric regimen in selected patients with clinically suspected serious catheter-related infections (e.g., bacteremia, cellulitis); known colonization with penicillin- and cephalosporin-resistant S. pneumoniae or methicillin-resistant S. aureus; initial blood culture results indicating presence of gram-positive bacteria; or hypotension or other evidence of cardiovascular impairment.
However, if vancomycin is included in an initial empiric regimen, it should be discontinued within 24-48 hours if results of cultures do not identify gram-positive bacteria susceptible to the drug. Successful treatment of infections in granulocytopenic patients requires prompt initiation of empiric anti-infective therapy (even when fever is the only sign or symptom of infection) and appropriate modification of the initial regimen if the duration of fever and neutropenia is protracted, if a specific site of infection is identified, or if organisms resistant to the initial regimen are present.
No empiric regimen has been identified that would be appropriate for initial treatment of all febrile neutropenic patients. The initial empiric regimen should be chosen based on the underlying disease and other host factors that may affect the degree of risk and on local epidemiologic data regarding usual pathogens in these patients and data regarding their in vitro susceptibility to available anti-infective agents.
The fact that gram-positive bacteria have become a predominant pathogen in febrile neutropenic patients should be considered when selecting an empiric anti-infective regimen. The Infectious Diseases Society of America (IDSA) recommends use of a parenteral empiric regimen in most febrile neutropenic patients; use of an oral regimen (e.g., oral ciprofloxacin and oral amoxicillin and clavulanate) should only be considered in selected adults at low risk for complications who have no focus of bacterial infection and no signs or symptoms of systemic infection other than fever.
At health-care facilities where gram-positive bacteria are common causes of serious infection and use of vancomycin in the initial empiric regimen is considered necessary, the IDSA recommends 2- or 3-drug combination therapy that includes vancomycin and either cefepime, ceftazidime, imipenem, or meropenem given with or without an aminoglycoside; vancomycin should be discontinued 24-48 hours later if a susceptible gram-positive bacterial infection is not identified.
At health-care facilities where vancomycin is not indicated in the initial empiric regimen, the IDSA recommends monotherapy with a third or fourth generation cephalosporin (ceftazidime, cefepime) or a carbapenem (imipenem, meropenem) for uncomplicated cases; however, for complicated cases or if anti-infective resistance is a problem, combination therapy consisting of an aminoglycoside (amikacin, gentamicin, tobramycin) given in conjunction with an antipseudomonal penicillin (ticarcillin and clavulanate, piperacillin and tazobactam), an antipseudomonal cephalosporin (cefepime, ceftazidime), or a carbapenem (imipenem, meropenem) is recommended.
Regardless of the initial regimen selected, patients should be reassessed after 3-5 days of treatment and the anti-infective regimen altered (if indicated) based on the presence or absence of fever, identification of the causative organism, and the clinical condition of the patient. Published protocols for the treatment of infections in febrile neutropenic patients should be consulted for specific recommendations regarding selection of the initial empiric regimen, when to change the initial regimen, possible subsequent regimens, and duration of therapy in these patients. In addition, consultation with an infectious diseases expert knowledgeable about infections in immunocompromised patients is advised.
Other Uses
Vancomycin is recommended by some clinicians as a drug of choice for the treatment of infections caused by Corynebacterium jeikeium (JK group). The drug has been used concomitantly with rifampin and/or an aminoglycoside for the treatment of early-onset prosthetic valve endocarditis caused by diphtheroids (e.g., C. jeikeium).
Vancomycin has been used orally with some success for the treatment of necrotizing ulcerative gingivitis and oral cavity infections. Vancomycin is recommended by some clinicians as a drug of choice for the treatment of infections caused by Bacillus cereus or B. subtilis.
Some clinicians suggest that infections caused by Rhodococcus equi be treated with a regimen of vancomycin used in conjunction with a fluoroquinolone, rifampin, imipenem (or meropenem), or amikacin. In at least one HIV-infected patient, vancomycin used in conjunction with imipenem was effective for the treatment of pulmonary infection caused by R. equi. R. equi has been identified as a cause of pulmonary infections (e.g., lung abscess) in immunocompromised individuals, including HIV-infected patients and solid organ transplant recipients. While optimum regimens for the treatment of these infections have not been identified, combination regimens usually are recommended.

