Type I reactions
Anaphylactic shock can occur, even after oral administration of penicillin and skin testing. However, anaphylactic shock is less common after oral than parenteral administration. In one study the incidence of anaphylactic shock was 0.04% of all patients treated with penicillin. It is also low in patients receiving long-term benzathine penicillin (1.2 million units every 4 weeks).
Four episodes of anaphylaxis occurred in 0.012% of injections (1.2 reactions to 10 000 injections).
Anaphylactic shock resulting in death occurred in 0.002% of all patients treated with penicillin and in 0.003% of those treated with benzathine penicillin. In nearly half of the cases, the course of anaphylactic shock, especially that induced by penicillin and other small molecular substances, is that of a cardiovascular reaction without any other effects suggestive of an allergic mechanism.
There is an extensive list of articles on anaphylactic shock to penicillins. General anesthesia does not inhibit the development of anaphylactic shock in penicillin allergy.
Diagnosis
The two most important elements in the evaluation of an individual for the presence or absence of beta-lactam hypersensitivity are the drug history and skin tests. Other diagnostic tools, such as measurement of drug-specific antibodies and lymphocyte transformation tests, are investigational or restricted to specialized laboratories. Standardized and widely used protocols for skin testing only exist for the penicillins and allow assessment of IgE-mediated hypersensitivity.
The most commonly used reagents are penicilloyl-polylysine (PPL, which contains multiple penicilloyl molecules coupled to a polyly-sine carrier) and fresh penicillin followed by minor determinant mixtures (MDM), containing penicilloate, benzylpenicilloate, and benzylpenilloate.
A survey conducted among members of the American Academy of Allergy and Immunology reported the use of penicilloyl-polylysine and fresh penicillin by 86% and minor determinant mixtures by 40% of those responding to the questionnaire. Skin tests are first applied as a prick test for safety. In the absence of a local or systemic reaction, an intradermal test is performed and interpreted as described elsewhere.
Experience with skin testing in penicillin allergy has been reviewed. Properly performed sequential testing is considered a safe procedure, and only an estimated 1 % or less of penicillin allergic patients will have systemic symptoms while undergoing skin tests.
However, at least three deaths have been reported with both epicutaneous and intradermal testing. In a collaborative study in the National Institute of Allergy and Infectious Diseases (NIAID), hospitalized patients were tested with major and minor skin test reagents in order to assess the predictive value of skin testing. Among 600 history-negative patients, 568 had negative skin tests and none had a reaction to penicillin. Among 726 history-positive patients, 566 had a negative skin test and received penicillin, seven of whom (1.2%) had a possibly IgE-mediated reaction.
Nine of the 167 patients with positive skin tests were exposed to penicillin, two of whom had reactions compatible with IgE-mediated reactions. These data suggest that overall, 99% of patients with negative skin tests to penicilloyl-polylysine and minor determinant mixtures can safely receive penicillin.
A history of a previous reaction slightly increases the risk of an adverse reaction, to 1.2%. Most positive skin tests were detected with penicilloyl-polylysine with or without minor determinant mixtures, and a further 16% reacted to minor determinant mixtures alone. In another study in an outpatient clinic for sexually transmitted diseases, 5063 consecutive patients were tested with penicilloyl-polylysine with and without minor determinant mixtures. The role of the history of a previous penicillin reaction was emphasized in this study: 1.7% of history-negative subjects had a positive skin test; in contrast, 7.1% of history-positive patients had a positive skin test, and a previous history of anaphylaxis or urticaria was associated with positive skin tests in 17% and 12% respectively.
Penicillin was safe in more than 99% of patients with a negative history and a negative skin test. Reactions were more common (2.9%) in patients with a positive history and a negative skin test. The reactions were mild and self-limiting. Two patients with a history of severe IgE-mediated reaction had mild anaphylactic reactions. Relatively safe doses for skin testing, provided that one begins with a prick test, are 25 nmol/ml of penicilloyl-polylysine and purified benzylpenicillin. Positive skin tests of the immediate type with penicilloyl-polylysine are usually obtained 2 weeks to 3 months after the clinical reaction.
The safety of such an approach has been challenged in a description of three patients who were negative in skin tests with penicilloyl-polylysine and minor determinant mixtures and who tolerated therapeutic doses of benzyl-penicillin, but reacted to amoxicillin. In an extension of that study, 177 patients who were allergic to beta-lactams were identified using the clinical history, a skin test panel including penicilloyl-polylysine, and minor determinant mixtures, as well as ampicillin and amoxicillin and drug-specific radio-allergosorbent tests. Fifty-four patients (31%) tolerated penicillin G but reacted to amoxicillin with anaphylaxis, urticaria, or angioedema.
Skin tests with penicilloyl-polylysine and minor determinant mixtures failed to detect those patients, but tests with amoxicillin were positive in 63%. Canadian data have partly confirmed these findings.
Benzylpenicillin derivatives and semisynthetic penicillins were applied to 112 patients with a history of an allergic reaction to penicillins. The tests were positive in 21 patients (19%), of whom 10 reacted against the semisynthetic penicillin reagents only. Reports of subjects allergic to flucloxacillin, cloxacillin, and cefa-droxil, but not penicillin, lend further support to the concept of side chain-specific allergic reactions (see the post on beta-lactam antibiotics).
Management
Fearing penicillin anaphylaxis, many clinicians overdiag-nose penicillin allergy in patients who have not had a true allergic reaction. Consequently, penicillins are withheld from many patients who could safely receive them. This was the background to a study whose objectives were to determine the likelihood of true penicillin allergy, taking into consideration the clinical history, and to evaluate the diagnostic value added by appropriate skin testing. The authors searched MEDLINE for relevant English-language articles dated 1966 to October 2000. Bibliographies were searched to identify additional articles. Original articles describing the precision of skin tests in the diagnosis of penicillin allergy were included, and studies that did not use both minor and major determinants were excluded; 14 studies met the inclusion criteria. At least three authors independently reviewed and abstracted the data from all the articles and reached a consensus about any discrepancies.
Some of their conclusions are worth remembering:
- 80-90% of all patients who report penicillin allergy have negative skin tests, suggesting that penicillins are withheld from many patients who could safely receive them;
- patients who develop a rash while taking penicillins should not be automatically labeled as allergic without considering other possibilities, including rashes due to ampicillin distinct from allergic rashes, and rashes caused by the infection being treated or by other drugs;
- for patients with a history of immediate (type I) penicillin allergy who have a compelling need for penicillin, skin testing should be performed;
- at least 98% of patients with positive histories of penicillin allergy and negative skin test results can tolerate penicillin without any sequelae.
Desensitization
Patients with a history of penicillin allergy should undergo skin testing with both penicilloyl-polylysine and minor determinant mixtures. Patients with positive skin tests should be treated with another immunologically unrelated compound or should undergo desensitization.
The management of patients with a negative skin test but a history of a severe IgE-mediated reaction has to be individualized; options include the use of an alternative compound, desensitization, or the controlled administration of a test dose.
Acute drug desensitization is commonly described as the process by which a drug-allergic individual is converted from a highly sensitive state to a state in which the drug is tolerated. The procedure involves cautious administration of incremental doses of the drug over a short period of time (hours to a few days). In the past it has mainly been considered to be of value in patients in whom IgE antibodies to a particular drug are known or assumed to exist and no alternative treatment agent is available. In clinical practice, most of the desensitization protocols have involved penicillins. However, the principle has been applied successfully to other agents as well, including other antibiotics, insulin, chemotherapeutic agents, vaccines, heterologous sera, and other proteins.
Mechanism It has been stated that in patients with penicillin-specific IgE antibodies who underwent successful penicillin desensitization, the data suggest that anti-specific, mast cell desensitization is responsible for the tolerant state and that mediator depletion plays no role. Additionally, the clinical observation that wheal-and-flare skin responses to penicillin often become negative with successful desensitization, while IgE responses to other antigens remain unchanged, also supports an involvement of an antigen-specific mechanism.
Furthermore, both clinical reactivity and skin-test reactivity return within a few days, unless a tolerant state is maintained by continued drug administration. The author stressed that these findings show that the desensitized state depends on the continuous presence of antigen and that clinical sensitivity returns rapidly in the absence of antigen. However, the underlying mechanisms responsible for the antigen-specific desensitized state are still unclear. It has been hypothesized that IgE receptor aggregation may generate counter-regulatory forces that, instead of causing cell activation, actually extinguish activating signals. The key point is that during desensitization, the drug is introduced very slowly and the drug concentration rises gradually.
The slow rate of possible receptor aggregation caused by the gradual increase in drug concentration, along with suppression of cellular activation signals, may lead to antigen-specific desensitization and clinical tolerance. It has also been long thought that during desensitization, univalent drug-hapten protein conjugates are formed and may act by inhibiting the cross-linking of drug-specific IgE molecules on mast cells. It is slightly surprising that this prospect has not come into routine therapy.
Procedure Beta-lactam desensitization should be done in an intensive care unit and any concomitant risk factors for anaphylaxis, such as use of beta-blockers should be corrected. Protocols based on incremental use of the drug orally or parenterally have been described.
The oral route is preferable and is associated with a lower incidence of adverse events, but mild transient reactions are frequent. Pregnant women with limited antibiotic choices have been treated with immunotherapy. Repeated administration will maintain a state of anergy, which is often lost after withdrawal. At the conclusion of therapy, patients must be informed that after withdrawal, they may once again become allergic to penicillin, with a new reaction to the first subsequent application.
Desensitization is not effective in non-IgE-mediated reactions and should therefore not be attempted, for example in cases of serum sickness-like syndromes or Stevens-Johnson syndrome.
Treatment of acute anaphylaxis
For acute anaphylaxis, immediate treatment is essential, with adrenaline followed by intravenous histamine Hx receptor antagonists, glucocorticoids, fluids, and electrolytes. In view of the frequency of cardiac dysrhythmias and conduction disturbances in patients with anaphylactic shock, they should immediately be monitored.
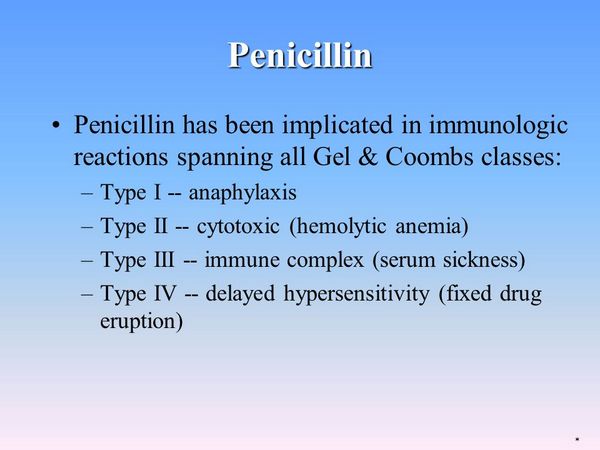
Type III reactions
Serum sickness was first described by von Pirquet and Schick in 1905 and was regarded as a syndrome resulting from the administration of heterologous serum or other foreign proteins. The immunopathology of classic serum sickness results from antigen-antibody complex formation with a foreign protein as the antigen. Characteristic symptoms include fever, cutaneous eruptions, edema, arthralgia, and lymphadenopathy. The incidence of classical serum sickness has fallen secondary to the refinement of foreign proteins. However, a serum sickness-like reaction that is clinically similar to classical serum sickness can result from the administration of a number of non-protein drugs, such as tetracyclines, penicillins, and cephalosporins. The reaction typically occurs within 1 month of the start of therapy and resolves after withdrawal. Serum sickness has been associated with penicillins.
- A 39-year-old woman developed the characteristic symptoms for serum sickness, having completed a 5-day course of amoxicillin for a perilingual infection 1 week before. She was treated with prednisone 60 mg/day and diphenhydramine 25-50 mg tds. Her symptoms gradually resolved and the prednisolone dose was tapered over 2 weeks.
- A 29-year-old woman complained of fever, rash, throat and facial swelling, abdominal pain, and increasing joint pain, leaving her wheelchair-bound. Her symptoms started a week after she had completed a 10-day course of penicillin V for a dental abscess. She was given oral methylprednisolone, 40 mg every 6 hours, and over the next few days her symptoms gradually resolved.
- A 29-year-old woman developed symptoms of serum-sickness 2 weeks after completing a 21-day course of co-amoxiclav for sinusitis. She responded to prednisone 40 mg/day. The authors suggested that serum sickness may be more common than has previously been described and that the reaction may be under-reported or unrecognized.




