Drug Approvals
INNs in other languages (French, Latin, and Spanish): Amfotericin; Amfotericin B; Amfotericina B; Amfotericinas B; Amfoterisiini; Amfoterisiini B; Amfoterisin; Amfoterisin B; Amfoterycyna b; Amphotericin; Amphotericine B; Amphotericinum; Amphotericinum B; Anfotericina B.
C47H73NOl7= 924.1.
CAS — 1397-89-3.
ATC — A01AB04; A07AA07; C01AA03; J02AA01.
Pharmacopoeias in China, Europe, International, Japan, and US
European Pharmacopoeia, 6th ed. (Amphotencin B Amphotericin BP 2008)
A mixture of antifungal polyenes produced by the growth of certain strains of Strepiomyces nodosus or by any other means. It consists largely of amphotericin B. It occurs as a yellow or orange powder. The potency is not less than 750 units per mg with reference to the dried substance. It contains not more than 10% of tetraenes, or not more than 5% if intended for use in parenteral dosage forms. Practically insoluble in water and in alcohol soluble in dimethyl sulfoxide and in propylene glycol slightly soluble in dimethylformamide very slightly soluble in methyl alcohol. Amphotericin B is inactivated at low pH values. Store at 2° to 8° in airtight containers. Protect from light.
The United States Pharmacopeia 31, 2008(Amphotericin B)
A yellow to orange, odourless or practically odourless, powder. It contains not less than 750 micrograms of C47H73N017 per mg, and, for material intended for oral or topical use, not more than 15% of amphotericin A, both calculated on the dried substance. Insoluble in water, in dehydrated alcohol, in ether, in benzene, and in toluene soluble in dimethylformamide, in dimethyl sulfoxide, and in propylene glycol slightly soluble in methyl alcohol. Store at a temperature not exceeding 8° in airtight containers. Protect from light.

Formulation
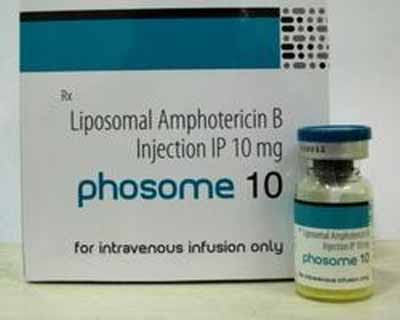
Conventional formulations of amphotericin B injection are typically a complex of amphotericin B and deoxy-cholate with suitable buffers which form a colloidal dispersion when reconstituted. Nonconventional ‘lipid’ formulations of amphotericin B for injection include liposomal amphotericin B, a colloidal dispersion of an amphotericin B and sodium choles-teryl sulfate complex, and a phospholipid complex.
Incompatibility
Because of the wide range of incompatibilities reported with conventional and lipid formulations of amphotericin B, it is generally advisable not to mix them with any other drug. Most incompatibilities are caused by precipitation of amphotericin B due to a change in pH or by the disruption of the colloidal suspension.
Precipitation can occur if amphotericin B is added to sodium chloride 0.9% or to electrolyte solutions. Although heparin is generally reported to be compatible with conventional amphotericin B injection, care should be taken if heparin flush solutions, which are diluted with sodium chloride solution, are used to maintain the patency of intravenous lines in patients receiving amphotericin B.
Flushing the intravenous line with 5% glucose solution has been suggested. Mixtures of conventional amphotericin B in commercial lipid emulsions have been reported to be unstable, although others have reported satisfactory stability. In one study, vigorous agitation of the mixtures enhanced their stability when compared with gentle mixing.
Preparation of solutions for injection
Recommendations from the manufacturers for preparation of amphotericin solutions are:
- conventional amphotericin B formulations for injection are prepared by reconstitution of amphotericin B with sterile water for injection without preservatives, then dilution with glucose injection 5% with a pH above 4.2 to the desired final concentration.
- liposomal amphotericin B: injections are prepared by reconstitution with sterile water for injection without a preservative the required reconstituted amount is then withdrawn and injected via a sterile filter into the desired volume of glucose 5%.
- amphotericin B-sodium cholesteryl sulfate complex: injections are prepared by rapidly adding the required amount of water for injection, then further diluting with glucose 5% until the desired final concentration is reached.
- amphotericin B-phospholipid complex: before infusion the suspension concentrate must be diluted to the required final concentration with glucose 5%. The required amount of concentrate is injected via a sterile filter into the glucose 5%. Caution: Mixture with sodium chloride injection 0.9% would precipitate amphotericin B.
Stability of oral suspensions
An oral suspension of amphotericin B 100 mg/mL, prepared from powder and a cherry-flavoured vehicle and maintained at pH 5.3, was found to be stable at 22 to 25° for 93 days.
Adverse Effects
Amphotericin B for intravenous use was originally only available in a conventional colloidal form lipid formulations have been developed to reduce toxicity.
The following adverse effects apply to the conventional form. Common adverse effects which occur during or after intravenous infusion of amphotericin B include headache, nausea, vomiting, chills, fever, malaise, muscle and joint pains, anorexia, diarrhoea, and gastrointestinal cramp.
Hypertension, hypotension, cardiac arrhythmias including ventricular fibrillation and cardiac arrest, skin rashes, flushing, anaphylactoid reactions including bronchospasm and dyspnoea, blurred vision, tinnitus, hearing loss, vertigo, gastrointestinal bleeding, liver disorders, peripheral neuropathy, and convulsions have been reported occasionally. Some degree of nephrotoxicity occurs in almost all patients given amphotericin B intravenously.

Both tubular and glomerular damage occur there may be improvement on cessation of therapy, but there is a risk of permanent renal impairment, particularly in patients given large cumulative doses (over 5 g).
Renal tubular acidosis without systemic acidosis may develop. Use of amphotericin B is associated with increased urinary excretion of potassium and magnesium resulting in hy-pokalaemia and hypomagnesaemia respectively. Uric acid excretion is increased and nephrocalcinosis can occur. Limited data indicate that renal toxicity may be associated with sodium depletion for strategies to improve sodium load see Nephrotoxicity, under Treatment of Adverse Effects, below. A reversible, normocytic, normochromic anaemia develops in most patients given amphotericin B, possibly due to a direct suppressive effect on erythropoietin production.
There are rare reports of thrombocytopenia, leucopenia, agranulocytosis, eosinophilia, and coagulation defects. Leukoencephalopathy has been reported rarely in patients also receiving total body irradiation. Amphotericin B solutions irritate the venous endothelium and may cause pain and thrombophlebitis at the injection site. Extravasation may cause tissue damage. After intrathecal injection amphotericin B may also cause irritation of the meninges, neuropathy with pain, impaired vision, and retention of urine. In general, adverse effects of lipid formulations have been similar to those of conventional amphotericin B, but are less frequent and less severe.
Brief reversible episodes of renal impairment have been observed but these formulations have been considered to be safe enough to use in patients with renal impairment who could not be given conventional amphotericin B. Ana-phylaxis has been reported rarely. Amphotericin applied topically may produce local irritation, pruritus, and skin rash.
Effects on the cardiovascular system
Ventricular arrhythmias in 2 patients, resulting in fatal sudden cardiac arrest in 1, were associated with both conventional and liposomal formulations of amphotericin B at conventional doses and infusion rates, but cardiac toxicity is more common with high doses or rapid infusion rates (see Infusion Rate, under Administration, below).
Cardiac arrests in 5 infants and children, fatal in 4 cases, were associated with overdoses of conventional amphotericin B of between 3.8 and 40.8 mg/kg. Fatal cardiac toxicity has also been reported in an adult who inadvertently received an overdose (5 mg/kg) of conventional amphotericin B on 2 consecutive days. A case of reversible dilated cardiomyopathy and congestive heart failure has been reported in a 20-year-old male patient after about 2 months of treatment, initially with conventional amphotericin B for 30 days and then with amphotericin B phosphol-ipid complex.
Symptoms resolved within 6 weeks of stopping treatment An increased risk of arrhythmia and cardiac arrest has been reported in patients with evidence of antimony-induced myocardial damage who were switched to amphotericin B treatment for visceral leishmaniasis. A rest period of at least 10 days was advised before beginning amphotericin B in such patients. Severe hypertension was associated with infusion of phospholi-pid-amphotericin B complex in 1 patient.

Effects on the eyes
Rapid loss of vision resulting in permanent bilateral blindness occurred in a patient with lupus ery-thematosus and cryptococcal meningitis after a 1 -mg test dose of amphotericin B. Amphotericin B was considered to be the cause as visual disturbances associated with cryptococcal meningitis are usually progressive in nature and acute blindness with normal funduscopic appearance had not previously been reported.
Effects on the liver
Amphotericin B has only rarely been associated with adverse effects on the liver. Fatal hepatic failure was reported in a patient after a total dose of 4.82 g given intermittently over 1 year. The patient had been given a potentially incompatible intravenous admixture of amphotericin B and diphenhydramine. There have been a few reports of abnormal liver-function tests during amphotericin B therapy in such cases amphotericin B should be stopped. Hyperbilirubinaemia associated with amphotericin B has also been reported. An episode of reversible hepatic and renal toxicity has been reported in a child with cystic fibro-sis after a cumulative dose of 84 mg of conventional amphotericin B and 168 mg ofliposomal amphotericin B.
Effects on the lungs
Reports implicating use of leucocytes or other blood products in the development of pulmonary reactions in patients receiving amphotericin B have been refuted, and a report has indicated that amphotericin B can produce pulmonary toxicity in the absence of blood products. An increased incidence of pulmonary symptoms was noted in patients given amphotericin B in lipid emulsion, including acute respiratory distress after starting the infusion. Chest discomfort, including tightness, pain, dyspnoea, and acute hypoxia, has been reported in 3 patients during one-hour infusions of liposomal amphotericin B. The reactions occurred within 5 to 10 minutes of starting the infusion and resolved on stopping the infusion. A slower rate of infusion was subsequently tolerated in 2 patients.
Effects on potassium homoeostasis
In addition to the hypokalaemia known to be associated with amphotericin B and due to increased urinary excretion of potassium, hyperkalaemia has been reported in a patient with severe renal impairment who received a rapid infusion of amphotericin B (see Infusion Rate, under Administration, below). Hyperkalaemia also occurred in a 2-year-old child with chronic renal failure after a two-hour infusion of conventional amphotericin B. Hyperkalaemia and fatal cardiac arrest were also reported in a 4-year-old child after 3 infusions of amphotericin B lipid complex.
Hypersensitivity
Anaphylactoid reactions have occurred with conventional amphotericin B, but have also been associated with liposomal amphotericin B, including reports of patients who subsequently tolerated conventional formulations.
Red man syndrome
Red man syndrome (see Vancomycin) occurred in a patient on 2 occasions after a 1-mg test dose of amphotericin B.
Treatment of Adverse Effects
To reduce febrile reactions antipyretics and antihista-mines may be given before the intravenous infusion of conventional amphotericin B. Hydrocortisone given intravenously before or during amphotericin B infusion may also reduce febrile reactions. However, corti-costeroids should not be given indiscriminately to patients given amphotericin B (see Interactions, below) and dosage should be kept to a minimum. In the UK the advice is to give antipyretics or hydrocortisone pro-phylactically, but only to patients who have previously had acute adverse reactions and in whom continued treatment with intravenous amphotericin B is essential (see Prophylaxis). Pethidine has been given intravenously to treat amphotericin B-induced shaking chills. Antiemetics may also be required. Amphotericin B is not removed by haemodialysis. Hypokalae-mia and hypomagnesaemia should be corrected, and adequate hydration and sodium supplements may reduce the severity of renal impairment. Lipid formulations of amphotericin B can be substituted for conventional amphotericin B if the latter cannot be tolerated. Heparin has been added to conventional amphotericin B infusions to reduce the incidence of thrombophlebitis.
Anaemia
Amphotericin B appears to produce a normochro-mic, normocytic anaemia by suppression of erythropoietin production. Stopping amphotericin B reverses the suppression but if the anaemia is severe, or treatment with amphotericin B cannot be stopped, blood transfusions may be required. Recombinant erythropoietin may prove an alternative to blood transfusions in patients who need to continue treatment with amphotericin B.
Electrolyte disturbances
It has been suggested that amiloride could ameliorate the hypokalaemia and hypomagnesaemia associated with amphotericin B. However, since amiloride may produce sodium depletion and its own associated renal toxicity this strategy is potentially hazardous. Another report has suggested that spironolactone may be a safe and effective method of preventing hypokalaemia.
Nephrotoxicity
A review of strategies for limiting the toxicity of amphotericin B concluded that sodium balance should be monitored and sodium replacement implemented if necessary and that, where possible, salt restriction and drugs that potentiate sodium loss or nephrotoxicity should be avoided. Correction of sodium depletion may reverse amphotericin B-induced nephrotoxicity. However, assessment of sodium status and correction of deficiency should precede use of amphotericin B.
While supplementation with 150 mmol sodium has been recommended for suitable patients, routine prophylactic use of sodium is not advised. However, a randomised study in a small number of patients has suggested that prophylactic sodium supplementation could be beneficial, but that it enhances potassium loss. Diuretics in general should be avoided although there have been suggestions that potassium-sparing diuretics such as amiloride or spironolactone may be useful in preventing hypokalaemia (see Electrolyte Disturbances).
Use of mannitol as a protective agent is controversial and is notrecommended. Amphotericin B is often given on alternate days although this has never been proven to reduce nephrotoxicity. More recently, lipid formulations have been reported to overcome most problems of chronic nephrotoxicity, even in patients with renal impairment after previous treatment with conventional amphotericin B (see Lipid Formulations, under Administration, below).
Prophylaxis
The value of prophylaxis against generalised reactions to amphotericin B infusion was questioned after a retrospective study in 397 patients. The most commonly used drugs were diphenhydramine, corticosteroids, paracetamol, and heparin. It was concluded that patients who had had an adverse reaction after amphotericin B should be given appropriate pre-medication before subsequent amphotericin B infusions, but that routine premedication was not justified.
Precautions
Although anaphylaxis is rare after intravenous amphotericin B, it is advisable to give a test dose and then to observe the patient carefully for about 30 minutes before starting treatment. Patients experiencing acute toxic reactions in whom treatment is essential may be given prophylactic treatment, as mentioned in Treatment of Adverse Effects, above, to ameliorate the reactions. To reduce the risk of vein irritation and infusion-related adverse effects, the rate of intravenous infusion of conventional amphotericin B should be slow (see Infusion Rate, under Administration, below). Patients given any parenteral form of amphotericin B should be monitored for changes in renal function, liver function, serum electrolytes, and haematological status. If the BUN or creatinine concentrations increase to clinically significant levels amphotericin B therapy should be interrupted or the dose reduced until renal function improves. Alternatively, a lipid amphotericin B preparation may be substituted. Treatment should be stopped if liver function tests are abnormal.
Acute pulmonary reactions have been noted in patients given amphotericin B during or shortly after leucocyte transfusions. Although the association is contested (see Effects on the Lungs, above), manufacturers of some amphotericin B products consider it advisable to separate the two and to monitor pulmonary function in these patients. Care should be taken not to confuse the dosage regimens for individual preparations, and in particular those of conventional and lipid formulations.
Pregnancy
There are case reports of conventional amphotericin B having been used successfully to treat fungal infections in pregnant women without any adverse effects on the infant. A review of the use of antifungal drugs in pregnancy concluded that parenteral amphotericin B was the drug of first choice in the treatment of serious fungal infections in pregnancy. The safety of the lipid amphotericin formulations in pregnancy is not yet clear, although there has been a report of a series of 5 pregnant women with visceral leishmaniasis who were treated in the first or second trimester with a short course of liposomal amphotericin B without adverse effects on the infant.
Interactions
Most interactions involving amphotericin B have been observed during treatment with conventional formulations.
Since lipid formulations appear to be less toxic, it may be anticipated that they will produce fewer serious interactions. Use of nephrotoxic antibacterial s, ciclosporin or other nephrotoxic immunosuppressants, or parenteral penta-midine may lead to an increased risk of nephrotoxicity. If possible, amphotericin B should not be given to patients receiving antineoplastics.
Diuretics should generally be avoided in patients taking amphotericin B. If a diuretic has to be given then volume and electrolyte depletion should be monitored carefully. The potassium-depleting effect of amphotericin B may enhance the effects of neuromuscular blocking drugs and may increase the toxicity of digitalis glycosides corticoster-oids may enhance the depletion of potassium and their immunosuppressive effects may be detrimental in patients with severe fungal infections. Amphotericin B may increase the toxicity of flucyto-sine, but the combination is nonetheless used in severe infections for its synergistic activity.
For information on synergistic and antagonistic effects with other antimicrobials, see under Antimicrobial Action, below. Renal excretion of zalcitabine may be reduced by amphotericin B. For an increased risk of cardiac arrhythmias and arrest when amphotericin B was given to patients with myo-cardial damage induced by an antimony compound, see Effects on the Cardiovascular System, under Adverse Effects, above.
Antimicrobial Action
Amphotericin B is a polyene antifungal antibiotic which appears to act mainly by interfering with the permeability of the cell membrane of sensitive fungi by binding to sterols, chiefly ergosterol. It is reported to be fungistatic at concentrations achieved clinically. It is active against Absidia spp., Aspergillus spp., Basidiobolus spp., Blastomyces dermatitidis, Candida spp., Coccidioides immitis, Conidiobolus spp., Cryptococcus neoformans, Histoplasma capsulatum, Mucor spp., Paracoccidioides brasiliensis, Rhizopus spp., Rhodotorula spp., and Sporothrix schenckii. Other organisms that have been reported to be sensitive to amphotericin B include the algal Prototheca spp. and the protozoa Leishmania and Naegleria spp. It is inactive against bacteria (including rickettsia) and viruses. Some resistant strains of Candida have been isolated from immunocompromised patients given prolonged treatment with amphotericin B.
Microbiological interactions
Azotes
Although there have been occasional reports of synergy between amphotericin B and the azole antifungals, greater emphasis has been placed on possible antagonism. Studies in vitro have supported theoretical concerns that the action of amphotericin B (which depends on binding to ergosterol in the fungal cell membrane) would be antagonised by azoles (which inhibit ergosterol synthesis).
Animal studies appear to have confirmed antagonism between amphotericin B and the imidazole ketoconazole, but not between amphotericin B and the triazoles fluconazole or itraconazole.
Available clinical evidence seems to indicate that azoles given with, or as continuation therapy after, induction therapy with amphotericin B, are effective in severe infections, although reduced plasma concentrations of itraconazole have been reported in some patients while being given amphotericin B.
However, strains of Candida albicans resistant to both amphotericin B and fluconazole have emerged in patients who have received repeated or prolonged courses of fluconazole.
Pharmacokinetics
There is little or no absorption of amphotericin B from the gastrointestinal tract. When given intravenously in the conventional colloidal form and in the usual increasing dosage regimens, peak plasma concentrations of 0.5 to 4 micrograms/mL have been reported the average plasma concentration with maintenance doses of 400 to 600 micrograms/kg daily tends to be 500 nanograms/mL.
Amphotericin B is highly bound to plasma proteins and is widely distributed, but passes into the CSF only in small quantities. The plasma half-life is about 24 hours with long-term use the terminal half-life increases to 15 days. Unchanged amphotericin B is excreted in small amounts slowly in the urine. Traces are present in the serum and urine several weeks after completion of treatment. Amphotericin B is not removed by haemo-dialysis.
The pharmacokinetics of the lipid formulations differ considerably from the conventional formulation and from each other:
- at clinical doses of 1 to 7.5 mg/kg, liposomal amphotericin B produces peak plasma concentrations of around 8 to 80 micrograms/mL, around 20 times those with conventional formulations
- after doses of 0.5 to 8 mg/kg, amphotericin B-sodium cholesteryl sulfate complex produces peak plasma concentrations of about 0.7 to 6.2 micrograms/mL
- at a dose of 5 mg/kg daily, amphotericin Bphospholipid complex produces maximum plasma concentrations of about 1.7 micrograms/mL Studies in animals have shown that concentrations in the kidney are several times lower after lipid formulations than with conventional ones.
Children and neonates
Serum-amphotericin B concentrations ranged from 0.78 to 10.02 micrograms/mL in 12 children (many with leukaemia) aged 4 months to 14 years after the intravenous infusion of conventional amphotericin B 0.25 to 1.5 mg/kg daily.
Serum concentrations did not correlate with dose. The elimination half-life was 18.1 + 6.65 hours. There was an inverse relationship between age and total clearance, suggesting that children older than 9 years may require lower doses.The pharmacokinetics of amphotericin B have also been studied in a group of 13 neonates with systemic fungal infections.
Conventional amphotericin B was infused over 4 to 6 hours every 24 hours. Ten of the infants started treatment with 100 micrograms/kg increased over 4 to 6 days to 500 micrograms/kg. Three infants were started on a dose of 800 to 1000 micrograms/kg reduced to 500 micrograms/kg daily. All infants were maintained on 500 micrograms/kg daily total doses ranged from 17.3 to 28.6 mg/kg.
Serum-amphotericin B concentrations were measured after the first dose in 3 infants in the first group and 2 in the second no serum-amphotericin B could be detected in the 3 infants who had received 100 micrograms/kg. After 5 days of treatment peak serum-amphotericin B concentrations ranged from 0.5 to 4.0 micrograms/mL and this was considered to be the range that could be achieved with the daily maintenance dose of 500 micrograms/kg. The elimination half-life was 14.8 hours.
Drug elimination between doses was not detected in 4 of the infants one was in oliguric renal failure and the other 3 had developed increases in serum-creatinine concentrations. CSF-amphotericin B concentrations in 5 of the neonates ranged from 40 to 90% of simultaneous serum concentrations. It was considered that an initial dose of 500 micrograms/kg was well tolerated and could produce therapeutic serum concentrations more quickly than a regimen which consisted of 100 micrograms/kg on day one increased over 4 to 6 days to 500 micrograms/kg daily.
A comparative study of plasma concentrations of liposomal amphotericin B in adults, children, and neonates after a dose of 1 mg/kg daily for 28 days, reported peak concentrations in children and neonates that were significantly lower than in adults. Increases in the mean peak plasma concentrations over days 1 to 28 were: adults, 1.02 to 1.66 micrograms/mL children aged 1 to 12 years, 0.63 to 1.10 micrograms/mL and neonates, 0.54 to 0.73 micrograms/mL. This was thought to be due to the greater volume of distribution in the neonates and greater clearance in older children.
The pharmacokinetics of amphotericin B lipid complex was studied in a cohort of 6 paediatric cancer patients with hepatosplenic candidiasis receiving a dose of 2.5 mg/kg daily for 6 weeks, to a total dosage of 105 mg/kg It was noted that the mean plasma concentrations over the dosing interval and area under the curve increased between the first and seventh doses but were similar between doses 7 and 42, suggesting that a steady state was achieved within 1 week of therapy. After the final dose of amphotericin B lipid complex, the mean plasma-amphotericin concentration was noted to be 0.50 micrograms/mL and the maximum concentration in whole blood was 1.69 micrograms/mL.
Distribution
Amphotericin B concentrations in various organs and tissues were determined in 13 cancer patients who had received conventional amphotericin B before death. Concentrations were determined by high-pressure liquid chromatography (HPLC) and bioassay. Mean recovery by HPLC reported as a percentage of total dose given was liver 27.5%, spleen 5.2%, lungs 3.2%, kidney 1.5%, heart 0.4%, brain 0.3%, and pancreas 0.2% each organ had a specific accumulation pattern.
The mean total recovery was 38.8%. Reported median bile concentration was 7.3 micrograms/mL. The drug concentrations obtained by bioassay were much lower than those measured by HPLC. As the HPLC-determined concentrations of amphotericin B were higher than the MICs for the pathogens in patients with candidiasis or aspergillosis, the poor clinical outcome in these patients suggested that amphotericin B in the tissue lacked antifungal activity. In another study, amphotericin B was not detected in the CSF of 4 AIDS patients with cryptococcal meningitis on intravenous maintenance conventional doses of 350 to 1890 micrograms/kg given 1 to 7 times weekly. The clinical success of amphotericin B for this indication could not be explained by measurable CSF drug concentrations. Concentrations of amphotericin B have been measured in fetal-cord serum in an infant and were 37.5% of maternal serum concentration.
Half-life
The terminal half-life for amphotericin B was 15 days in 2 patients on completion of conventional amphotericin B infusion therapy for disseminated histoplasmosis. In another study,the half-life was 21.5 hours (based on the exponential phase of disappearance from the blood) in a 65-year-old patient on a maintenance conventional dose of 500 micrograms/kg infused over 1 hour every other day. Serum concentrations appeared to plateau at about 600 nanograms/mL 36 to 48 hours after each dose. This suggested that alternate-day dosage might be effective.
Uses and Administration
Amphotericin B is a polyene antifungal antibiotic. It is reported to be fungistatic at concentrations achieved clinically. Amphotericin B is given by intravenous infusion in the treatment of severe systemic fungal infections including aspergillosis, blastomycosis, candidiasis, coccidioidomycosis, cryptococcosis, histoplasmosis, mucormycosis, paracoccidioidomycosis, and sporotrichosis, and is the usual treatment of choice in fungal endocarditis, meningitis, peritonitis, or severe respiratory-tract infections. Many of these infections are most likely to occur in immunocompromised patients.
Amphotericin may be given with flucytosine in severe infections. Amphotericin B is also used for the local treatment of superficial candidiasis. It is taken orally for intestinal candidiasis, sometimes as part of regimens for selective decontamination of the digestive tract in patients at special risk of infection, such as those in intensive care. The role of amphotericin B in the treatment of the above systemic and local infections is discussed under Choice of Antifungal. Amphotericin B also has antiprotozoal activity. It is used for primary amoebic meningoencephalitis caused by Naegleria spp. and for the treatment of visceral and mucocutaneous leishmaniasis.
Administration and dosage
Amphotericin B is given by intravenous infusion conventionally as a colloidal complex with sodium deoxycholate. There is also a liposomal form and other complexes of amphotericin B available for use by infusion when conventional amphotericin B is contra-indicated because of toxicity, especially nephrotoxicity. Before starting therapy with any form of intravenous amphotericin B a test dose is usually advised and the patient observed carefully for about 30 minutes.
Details of intravenous administration and dosage vary according to the formulation being used. Therapy has sometimes continued for several months depending on the infection.
Doses are expressed in terms of amphotericin B.
- Conventional amphotericin B (Fungizone, UK). After an initial test dose (1 mg infused over 20 to 30 minutes) treatment usually starts with a daily dose of 250 micrograms/kg, increased gradually to a maximum of 1 mg/kg daily in seriously ill patients up to 1.5 mg/kg daily or on alternate days may be necessary. If treatment is stopped for longer than 7 days, it should be resumed at a dose of 250 micrograms/kg daily and increased gradually. The daily dose is infused over 2 to 4 hours at a concentration of 100 micrograms/mL in glucose 5%. Slower infusion, over up to 6 hours, may be necessary to reduce the incidence of acute toxic effects.
- Liposomal amphotericin B (AmBisome, UK). After an initial test dose (1 mg infused over 10 minutes), the usual dose is 1 mg/kg daily, increased gradually to 3 mg/kg if necessary. The daily dose is infused over 30 to 60 minutes at a concentration of 200 to 2000 micrograms/mL in glucose 5%.
- Amphotericin B-sodium cholesteryl sulfate complex (Amphocil, UK). After an initial test dose (2 mg infused over 10 minutes) the usual dose is 1 mg/kg daily, increased gradually to 3 to 4 mg/kg daily if necessary doses of up to 6 mg/kg daily have been given. The daily dose is infused at a rate of 1 to 2 mg/kg per hour at a concentration of 625 micrograms/mL in glucose 5%.
- Amphotericin B-phosphotipidcomplex (Abelcet, UK). After an initial test dose (1 mg infused over 15 minutes) the usual dose is 5 mg/kg daily. The daily dose is infused at a rate of 2.5 mg/kg per hour as a diluted suspension containing 1 mg/mL in glucose 5%.
Conventional amphotericin B may be given by intrathecal injection to patients with severe meningitis especially when intravenous therapy has been ineffective. Starting with 25 micrograms, the dose is gradually increased to the maximum that can be tolerated without excessive discomfort. The usual dosage is 0.25 to 1 mg given two to four times each week.
Conventional amphotericin B is also used orally as 10-mg lozenges or as a suspension containing 100 mg/mL for oral or perioral candidiasis. The suspension is given in a dose of 1 mL four times daily it should be retained in the mouth for as long as possible before swallowing. The lozenges are intended to be dissolved in the mouth and are given four times daily, increased to 8 lozenges daily if necessary. Doses of 100 to 200 mg are given four times daily as tablets or suspension to suppress intestinal Candida. Conventional amphotericin B has been given for can-diduria as a continuous bladder irrigation daily at a suggested concentration of 50 mg in 1000 mL of sterile water. Intermittent irrigation has also been tried.
Conventional amphotericin B has also been given into the lung by nebulised solution, into the eye topically or by subconjunctival or intravitreal injection, to the skin by topical application, into body cavities by instillation, and into joint spaces by intra-articular injection.
Administration
LIPID FORMULATIONS
A number of lipid formulations of amphotericin B have been developed in an attempt to minimise renal toxicity and acute toxic reactions. Three lipid-based formulations of amphotericin B available commercially in some countries are:
- liposomes (e.g. AmBisome)
- a lipid complex with L-a-dimyristoylphosphatidylcholine and L-a-dimyristoylphosphatidylglycerol (e.g. Abelcet)
- a colloidal dispersion with sodium cholesteryl sulfate (e.g. Amphocil)
The aim of reducing renal toxicity has largely been achieved, and in some cases patients unable to tolerate conventional amphotericin B have subsequently been successfully treated with one of the lipid-based formulations. Experience with these formulations suggests that they also produce fewer acute toxic reactions. Review articles on lipid formulations of amphotericin B indicate that clinical studies have generally been encouraging, and that although they differ in their pharmacodynamics, pharmacokinet-ics, and dosage, they appear to be clinically at least as effective as amphotericin B.
INFUSION RATE
Conventional amphotericin B is licensed for use by intravenous infusion over at least 2 hours. A long infusion time is inconvenient for outpatients and often impractical in patients receiving other intravenous medications. This may be overcome by using one of the lipid formulations that can be infused over 30 to 120 minutes. Shorter infusion times have been tried with conventional amphotericin B but although 2 studies in small numbers of patients without preexisting renal impairment found rapid infusion over 1 hour was generally no more toxic than infusion over 4 hours, another found infusion over 45 minutes to be more toxic than a 4-hour infusion during the first 5 to 7 days of treatment.
Cardiac toxicity reported in patients receiving rapid infusions includes atrial fibrillation in a patient with pre-existing cardiac disease, ventricular fibrillation associated with hyperkalaemia in a patient with severe renal impairment, and bradycardia and dilated cardiomyopathy in patients without apparent risk factors. Ventricular dysrhythmias were not observed in 27 patients with adequate renal function.
Conversely, continuous infusion of amphotericin B over 24 hours has resulted in fewer adverse effects and a significant reduction in nephrotoxicity compared with infusion over 4 hours.Furthermore, an observational study of 33 patients concluded that a continuous infusion of amphotericin B deoxycholate, started at 1 mg/kg daily and gradually escalated to 2 mg/kg daily was safe and well tolerated by most patients.
Administration in children and neonates
Intravenous doses for conventional and lipid formulations of amphotericin B similar to those in adults have been found to be safe and effective in children and neonates with candidiasis. For neonates with severe disease, dose increments of conventional amphotericin B every 12 hours have been given and daily doses up to 1.5 mg/kg tolerated. For prophylaxis of neonatal intestinal candidiasis conventional amphotericin B solution 100 mg is given orally once daily. Although the most appropriate dose of lipid formulations of amphotericin B for low-birth-weight preterm infants has yet to be firmly established reports suggest that they may be safe and effective at doses similar to those used in adults, relative to body-weight. For information on the pharmacokinetics and doses in children and neonates, see, above.
Leishmaniasis
The treatment of visceral and mucocutaneous leishmaniasis including the use of amphotericin B is described.

VISCERAL LEISHMANIASIS
Evidence of declining responsiveness to pentavalent antimonials has led to the evaluation of intravenous amphotericin B as an alternative for first-line therapy. WHO has included liposomal amphotericin B 3 mg/kg daily on each of 5 consecutive days and a sixth dose 6 days later among the regimens suggested for first-line therapy of Mediterranean visceral leishmaniasis in immunocompetent patients.
Similar doses are recommended by licensed product information for one product (AmBisome Gilead, USA), which recommends 3 mg/kg daily for5 days with further doses on days 14and21.
Experience with a short course of 10 mg/kg daily for 2 days was also shown to be effective in 41 immunocompetent children under 14 years, although 1 subsequently relapsed after 5 weeks.
Responses to liposomal amphotericin B have been reported to be slower in im-munocompromised patients relapses occurred in 8 of 11 patients despite treatment with liposomal amphotericin B 1.38 to 1.85 mg/kg daily for 21 days. Increasing the dose to 4mg/kg daily given on 10 days over a 38-day period did not improve the long-term outcome, although initial responses were good and this regimen is now that recommended by the licensed product information above. Due to frequent relapse in these patients secondary prophylaxis with intermittent amphotericin B has been considered.
An open-label, multicentre study with amphotericin B lipid complex in doses of 3 mg/kg every 21 days for 12 months was effective in 50% of HIV-infected patients. Another cohort study reported that 80% of HIV-infected patients were relapse free at 12 months after receiving an initial treatment course of liposomal amphotericin B in doses of 4 mg/kg daily for 5 consecutive days and then once weekly for 5 weeks, followed by secondary prophylaxis in doses of 5 mg/kg every 3 weeks. However, at 24 months about 45% of the patients had experienced relapses.
Amphotericin B is also being evaluated in other parts of the world. In India, conventional amphotericin B in modest doses (500 micrograms/kg on alternate days) produced good responses both in patients unresponsive to antimonials and as first-line therapy.
Experience with a higher dose of 1 mg/kg daily for 20 days achieved a 99% cure rate in 938 patients and a lower dose regimen of 0.75 mg/kg daily for 15 days was also found to be effective. Liposomal amphotericin B 2 mg/kg daily on 3, 5 or 7 days over a 10-day period all produced clinical cures and minimal toxicity, as did single infusions of 7.5 mg/kg or 5 mg/kg, or once-daily infusion of 1 mg/kg for 5 days.
Amphotericin B lipid complex 1, 2, or 3 mg/kg daily for 5 days, or 5 mg/kg given once or twice (5 days apart), has been used successfully although relapses occurred in some patients taking the lower doses in these latter studies. In Brazil, colloidal amphotericin B with sodium cholesteryl sulfate in a dose of 2 mg/kg daily for 5 days produced cures in 10 patients although 1 subsequently relapsed. A study by WHO suggested that more intensive courses of treatment may be needed in Brazil compared with India and Kenya.
MUCOCUTANEOUS LEISHMANIASIS
Amphotericin B is used in mu-cocutaneous leishmaniasis unresponsive to antimonials. Successful treatment with liposomal amphotericin B has been reported in immunocompetent and immunocompromisedpatients.
Primary amoebic meningoencephalitis
Amphotericin B is active in vitro against Naegleria fowleri and has been recommended for the treatment of primary amoebic meningoencephalitis (see Naegleria Infections) caused by this amoeba. There have been some case reports of survival after the use of intravenous and intrathecal amphotericin B. In all cases amphotericin B was combined with other antimicrobials, notably oral rifampicin.
Preparations
British Pharmacopoeia 2008: Amphotericin Lozenges; Amphotericin Oral Suspension
The United States Pharmacopeia 31, 2008, and Supplements 1 and 2: Amphotericin B Cream; Amphotericin B for Injection; Amphotericin B Lotion; Amphotericin B Ointment.
Proprietary Preparations
Argentina: Abelcet AmBisome Amfostat Amphotec Anfogen Australia: Abelcet AmBisome Amphocil Fungilin Fungizone Austria: Abelcet AmBisome Ampho-Moronal Amphocil Belgium: Abelcet AmBisome Fungizone Brazil: Abelcet AmBisome Amphocil Anforicin B Fungi B Fungizon Canada: Abelcet AmBisome Amphotec Fungizone Chile: Fungizon Czech Republic: Abelcet Amphocil Denmark: Abelcet AmBisome Fungilin Fungizone Finland: Abelcet AmBisome Fungizone France: Abelcet AmBisome Fungizone Germany: Abelcet AmBisome Ampho-Moronal Greece: Abelcet AmBisome Am-phiprol Amphocil Fungizone Hong Kong: Abelcet AmBisome Amphocil Fungizone Hungary: Abelcet AmBisome Amphocil Fungizone India: Fungizone Indonesia: Fungizone Ireland: Abelcet AmBisome Amphocil Fungizone Israel: AmBisome Amphocil Fungilin Fungizone Italy: Abelcet AmBisome Fungilin Fungizone Japan: AmBisome Malaysia: Abelcet Amphocil Fungizone Mexico: Amfostat Amphocil Candipres The Netherlands: Abelcet AmBisome Amphocil Fungizone Norway: Abelcet AmBisome Fungizone New Zealand: Abelcet AmBisome Fungilin Fungizone Philippines: Fungizone Poland: AmBisome Amphocil Portugal: Abelcet AmBisome Amphocil Fungizone Russia: AmBisome Amphoglucamin South Africa: AmBisome Fungizone Singapore: Abelcet AmBisome Amphocil Fungizone Spain: Abelcet AmBisome Amphocil Funganiline Fungizona Sweden: Abelcet AmBisome Fungizone Switzerland: Abelcet AmBisome Ampho-Moronal Fungizone Thailand: AmBisome Amphocil Fungizone Turkey: Abelcet AmBisome Fungizone UK: Abelcet AmBisome Amphocil Fungilin Fungizone USA: Abelcet AmBisome Amphotec Fungizone Venezuela: Amphotec Fungizone
Multi-ingredient
Austria: Mysteclin Brazil: Anfoterin Gino-Teracin Novasutin Talsutin Tericin AT Tricocilin B Vagiklin Chile: Talseclin France: Amphocycline Germany: Mysteclin Hong Kong: Talsutin Indonesia: Talsutin Italy: Anfocort Malaysia: Talsutin-F South Africa: Vagmycin Spain: Gine Heydenf Sanicel Trigon Topico Venezuela: Talsutin-F The symbol denotes a preparation no longer actively marketed.
