Buy Ketoconazole [Nizoral 200mg Tablets]
Ketoconazole is an imidazole antifungal that interferes with ergosterol synthesis and, therefore, alters the permeability of the cell membrane of sensitive fungi. It is reported to be fungistatic at concentrations achieved clinically. Ketoconazole has a wide spectrum of antimicrobial activity including activity against Blastomyces dermatitidis, Candida spp., Coccidioides immitis, Epidermophyton floccosum, Histoplasma capsulatum, Malassezia spp., Microsporum canis, Paracoccidioides brasiliensis, Trichophyton mentagrophytes, and T. rubrum. Some strains of Aspergillus spp., Cryptococcus neoformans, and Sporothrix schenckii are sensitive. Ketoconazole has activity against some Gram-positive bacteria and some antiprotozoal activity against Leishmania spp. There are rare reports of Candida albicans acquiring resistance to ketoconazole.
Drug Approvals
Synonyms: Ketoconazol; Ketoconazolum; Ketokonatsoli; Ketokonazol; Ketokonazolas; R-41400
The United States Pharmacopeia 31, 2008: Ketoconazole Oral Suspension Ketoconazole Tablets.
European Pharmacopoeia, 6th ed. (Ketoconazole).
A white or almost white powder. Practically insoluble in water, sparingly soluble in alcohol, freely soluble in dichloromethane, soluble in methyl alcohol. Protect from light.
Pharmacokinetics
Buy Ketoconazole without a prescription
Ketoconazole is quickly absorbed from the gastrointestinal tract, with oral bioavailability similar for tablets and suspensions, but higher for solutions. Its absorption is influenced by gastric pH; increased pH reduces bioavailability. Patients with AIDS may experience decreased absorption due to gastric hypochlorhydria, which can be normalized with dilute hydrochloric acid.
Administering ketoconazole with acidic beverages can enhance absorption in individuals with achlorhydria. Studies show that fasting adults achieve peak plasma concentrations of approximately 4.2 to 6.2 mcg/mL within 1-2 hours after a 200 mg dose, depending on the formulation. In contrast, non-fasting adults reach lower concentrations after meals. Ketoconazole’s distribution varies, showing minimal CNS penetration and being largely bound to plasma proteins (84-99%). The elimination half-life is biphasic, averaging 2 hours initially and 8 hours later. It is primarily metabolized in the liver and excreted via feces (57%) and urine (13%) within four days.
Chemistry
Ketoconazole, a synthetic azole antifungal agent, is an imidazole derivative structurally related to other imidazoles (e.g., butoconazole, clotrimazole, econazole). Ketoconazole occurs as a white to slightly beige powder and is practically insoluble in water. Ketoconazole has pKas of 2.9 and 6.5.
Uses
Oral ketoconazole is used to treat blastomycosis, candidal infections (e.g., oropharyngeal and/or esophageal candidiasis, vulvovaginal candidiasis, candiduria, and chronic mucocutaneous candidiasis), chromomycosis (chromoblastomycosis), coccidioidomycosis, histoplasmosis, and paracoccidioidomycosis.
The drug is also used orally to treat certain dermatophytoses and protozoal infections, including cutaneous or visceral leishmaniasis. In addition, it has been used to treat hypercalcemia in patients with sarcoidosis and tuberculosis-associated hypercalcemia.
Due to its endocrine effects, ketoconazole has been used to treat advanced prostatic carcinoma and various endocrine disorders. For systemic or subcutaneous mycoses, oral ketoconazole is used principally in immunocompetent patients with mild to moderately severe infections caused by susceptible fungi.
The drug should not be used for initial therapy in severe, life-threatening infections. In addition, because CSF concentrations of ketoconazole are unpredictable following oral administration, the drug should not be used to treat CNS fungal infections, including candidal, coccidioidal, or cryptococcal meningitis. Because of the potential for treatment failure, relapse, and/or disease progression (e.g., from CNS dissemination), close follow-up during and following ketoconazole therapy is recommended.
Blastomycosis
Oral ketoconazole is used to treat blastomycosis caused by Blastomyces dermatitidis. While IV amphotericin B or oral itraconazole are generally considered the drugs of choice for blastomycosis, oral fluconazole or oral ketoconazole are alternatives for mild to moderate disease. IV amphotericin B is generally the drug of choice for severe blastomycosis (including when the CNS is involved) and is also considered the drug of choice for all forms of the disease in immunocompromised individuals.
Ketoconazole usually has been effective when used in immunocompetent individuals with mild to moderate pulmonary or extrapulmonary blastomycosis, and the reported response rate with the drug is 70-100%. However, many clinicians consider oral itraconazole the drug of choice for the treatment of nonmeningeal, non-life-threatening blastomycosis and also recommend itraconazole for follow-up therapy in patients with more severe infections after an initial response has been obtained with IV amphotericin B. The fact that treatment failures have been reported when oral ketoconazole was used in the treatment of cutaneous or pulmonary blastomycosis in individuals who had asymptomatic or subclinical CNS involvement at the time of the initial diagnosis should be considered when selecting an antifungal agent for the treatment of blastomycosis.
Candidal Infections
Oral ketoconazole has been used for a variety of candidal infections, including candidiasis, candiduria, chronic mucocutaneous candidiasis, oropharyngeal or esophageal candidiasis, and vulvovaginal candidiasis. Mucocutaneous or noninvasive candidal infections such as oral thrush or oropharyngeal candidiasis usually can be adequately treated with topical antifungal therapy (e.g., clotrimazole oral lozenges, nystatin oral suspension, amphotericin B oral suspension) or oral antifungal agents (e.g., fluconazole, itraconazole, ketoconazole); however, topical therapy is usually is ineffective for the treatment of esophageal candidiasis and IV amphotericin B therapy may be required for the treatment of severe mucocutaneous candidiasis or infections caused by azole-resistant Candida.
Vulvovaginal Candidiasis
Oral ketoconazole has been effective for treating uncomplicated vulvovaginal candidiasis in non-pregnant women. Limited data suggest that oral ketoconazole (200-400 mg daily for 3-6 days) may be as effective as intravaginal therapy with clotrimazole, miconazole, or nystatin, ketoconazole.
Although oral ketoconazole is not considered a drug of choice for the treatment of uncomplicated vulvovaginal candidiasis, it is recommended as one of several alternatives for the maintenance treatment of recurrent vulvovaginal candidiasis. Because the effects of ketoconazole on the fetus are unknown, oral ketoconazole should not be used in the treatment of vulvovaginal candidiasis in pregnant women.
Uncomplicated Vulvovaginal Candidiasis
The US Centers for Disease Control and Prevention (CDC) and other clinicians recommend that uncomplicated vulvovaginal candidiasis (defined as vulvovaginal candidiasis that is mild to moderate, sporadic or infrequent, most likely caused by Candida albicans, or occurring in immunocompetent women) be treated with an intravaginal azole antifungal (e.g., butoconazole, clotrimazole, miconazole, terconazole, tioconazole) given in appropriate single-dose or short-course regimens or, alternatively, oral fluconazole given in a single-dose regimen.
These regimens generally have been associated with clinical and mycologic cure rates of 80-90% in otherwise healthy, nonpregnant women with uncomplicated infections. Although a 5-day regimen of oral ketoconazole has been used in the treatment of uncomplicated vulvovaginal candidiasis, the single-dose fluconazole regimen is the only oral regimen included in current CDC recommendations for the treatment of uncomplicated infections. The potential for toxicity (e.g., hepatotoxicity) and drug interactions associated with oral ketoconazole therapy should be considered.
Complicated and Recurrent Vulvovaginal Candidiasis
Oral ketoconazole has been used for chronic maintenance to prevent relapse of vulvovaginal candidiasis in a limited number of women with a history of recurrent infections. However, optimal regimens for treating recurrent vulvovaginal candidiasis (usually defined as four or more symptomatic episodes each year) have not been established.
Although each individual episode caused by C. albicans may respond to usual single-dose oral fluconazole or short-course intravaginal antifungal therapy, a longer duration of initial therapy may be necessary to achieve mycologic remission and chronic maintenance therapy may be necessary to prevent relapse.
The CDC and other clinicians recommend the use of an initial intensive regimen consisting of 7-14 days of an intravaginal azole antifungal or a 2-dose regimen of oral fluconazole (150 mg repeated 3 days later) followed by a maintenance antifungal regimen (given for 6 months). Maintenance regimens recommended by the CDC include intravaginal clotrimazole (500 mg once weekly), oral ketoconazole (100 mg once daily), oral fluconazole (100-150 mg once weekly), or oral itraconazole (400 mg once monthly or 100 mg once daily).
These maintenance regimens can be effective in reducing recurrent infections; however, 30-40% of women will have recurrent disease once maintenance therapy is discontinued. Vaginal cultures should be obtained from patients with recurrent infections to confirm the diagnosis and identify the causative organism.
These infections may be caused by resistant strains of C. albicans or, more commonly, by other Candida with reduced susceptibility to azole antifungal agents (e.g., C. glabrata). It has been suggested that repeated treatment of recurrent vulvovaginal candidiasis with intravaginal azole antifungal agents and widespread and/or injudicious use of these agents for self-medication of vulvovaginal candidiasis may favor the selection of Candida that are resistant to azole antifungal agents.
Optimum therapy for the treatment of vulvovaginal candidiasis caused by Candida with reduced susceptibility to azole antifungal agents has not been determined to date. For the treatment of vulvovaginal candidiasis caused by Candida other than C. albicans, the CDC recommends 7-14 days of an antifungal agent other than fluconazole; if recurrence occurs, intravaginal boric acid (600-mg capsule once daily for 2 weeks) is recommended. Referral to a specialist is advised. Vulvovaginal candidiasis may occur more frequently and may be more severe in women with human immunodeficiency virus (HIV) infection than in women without HIV infection and these infections have been recognized as an early manifestation of acquired immunodeficiency syndrome (AIDS) in women.
While optimum therapy for recurrent vulvovaginal candidiasis in HIV-infected women has not been established, there is no evidence to date that these women have a lower response rate to the intravaginal or oral antifungal regimens usually recommended for the treatment of vulvovaginal candidiasis. Therefore, the CDC and other clinicians recommend that the treatment of vulvovaginal candidiasis in HIV-infected women should be the same as that in women without HIV infection.
Chromomycosis
Oral ketoconazole has been used for the treatment of chromomycosis (chromoblastomycosis) caused by Phialophora spp. A response to ketoconazole has been obtained in some patients with mild to moderate infections, but not in those with more extensive disease. While optimum regimens for the treatment of chromomycosis have not been identified, other antifungal agents (e.g., flucytosine alone or in conjunction with amphotericin B, itraconazole) are generally preferred.
Coccidioidomycosis
Oral ketoconazole is used for the treatment of mild to moderate coccidioidomycosis caused by Coccidioides immitis. While acute, uncomplicated pulmonary coccidioidomycosis may be self-limiting and resolve spontaneously without specific antifungal therapy, severe pulmonary infections or disseminated coccidioidomycosis involving the skin, bone, meninges, and joints should be treated with aggressive antifungal agent therapy. The drugs of choice for the treatment of coccidioidomycosis are IV amphotericin B or oral fluconazole; oral itraconazole or oral ketoconazole are considered alternative agents. IV amphotericin B is generally the preferred agent for the initial treatment of severe or rapidly progressing coccidioidomycosis, especially in immunocompromised patients, including those with HIV infection.
Histoplasmosis
Oral ketoconazole is used for the treatment of histoplasmosis caused by Histoplasma capsulatum. The drugs of choice for the treatment of histoplasmosis are IV amphotericin B or oral itraconazole; oral ketoconazole or oral fluconazole are considered alternative agents. IV amphotericin B generally is the preferred antifungal agent for the initial treatment of severe, life-threatening histoplasmosis, especially in immunocompromised patients such as those with HIV infection. When an oral agent is indicated in the treatment of histoplasmosis (e.g., for treatment of mild to moderate infections or as follow-up therapy in the treatment of severe infections in patients with HIV infection after a response has been obtained with amphotericin B), itraconazole may be the preferred agent.
Paracoccidioidomycosis
Oral ketoconazole is used to treat paracoccidioidomycosis (South American blastomycosis) caused by Paracoccidioides brasiliensis. While IV amphotericin B is generally preferred for the initial treatment of severe paracoccidioidomycosis, oral azole antifungal agents (e.g., ketoconazole, and itraconazole) can be used in patients with less severe infections.
Dermatophytoses
Ketoconazole has been effective when used orally in the treatment of certain dermatophytoses (i.e., tinea capitis, tinea corporis, tinea cruris, tinea pedis, tinea manuum, tinea unguium) caused by Epidermophyton, Microsporum, or Trichophyton. Tinea corporis and tinea cruris generally can be effectively treated using a topical antifungal agent; however, an oral antifungal regimen may be necessary if the disease is extensive, dermatophyte folliculitis is present, the infection is chronic or does not respond to topical therapy, or the patient is immunocompromised or has coexisting disease. Tinea capitis and tinea barbae are generally treated using an oral antifungal regimen.
While topical antifungals are usually effective for treating uncomplicated tinea manuum and tinea pedis, an oral antifungal regimen is usually necessary for treating hyperkeratotic areas of the palms and soles, chronic moccasin-type (dry-type) tinea pedis, and tinea unguium (onychomycosis).
Dermatophytic infections of glabrous skin respond more rapidly to oral ketoconazole than infections of palmar-plantar skin, while infections of nails respond at the slowest rate.
Pityriasis (Tinea) Versicolor
Oral ketoconazole has been effective when used in the treatment of pityriasis (tinea) versicolor, a superficial infection caused by Malassezia furfur (Pityrosporum orbicular or P. ovale). Pityriasis (tinea) versicolor generally can be treated topically with an imidazole-derivative azole antifungal (e.g., clotrimazole, econazole, ketoconazole, miconazole, oxiconazole, sulconazole), an allylamine antifungal (e.g., terbinafine), ciclopirox olamine, or certain other topical therapies (e.g., selenium sulfide 2.5%). However, an oral antifungal (e.g., itraconazole, ketoconazole) may be indicated, with or without a topical agent, in patients who have extensive or severe infections or who fail to respond to or have frequent relapses with topical therapy.
Other Fungal Infections
Ketoconazole has been effective in some patients for treating eumycetoma caused by Madurella mycetomatis. Although it has been investigated for treating aspergillosis, cryptococcosis, mucormycosis, and sporotrichosis, the drug has generally been ineffective and is not indicated for these infections.
Prevention of Fungal Infections
HIV-Infected Individuals
Although ketoconazole has been used for prophylaxis against initial or recurrent mucocutaneous candidiasis in individuals with human immunodeficiency virus (HIV) infection, the drug is not included in the current guidelines of the Prevention of Opportunistic Infections Working Group of the US Public Health Service and the Infectious Diseases Society of America (USPHS/IDSA). The USPHS/IDSA currently states that primary prophylaxis to prevent first episodes of mucocutaneous candidiasis in HIV-infected adults, adolescents, infants, or children is not recommended because acute mucocutaneous candidiasis generally is treatable and rarely life-threatening and because of concerns about the potential for development of resistant Candida, the possibility of drug interactions, and cost of antifungal prophylaxis.
However, chronic suppressive or maintenance therapy (secondary prophylaxis) may be indicated in HIV-infected individuals with a documented history of frequent or severe episodes of mucocutaneous candidiasis. If suppressive or maintenance therapy against mucocutaneous candidiasis is indicated in HIV-infected adults, adolescents, infants, or children with frequent or severe recurrences of oropharyngeal, esophageal, or vaginal candidiasis, the USPHS/IDSA recommends oral fluconazole as the drug of choice and itraconazole oral solution as an alternative.
Transplant Patients and Patients with Cancer
Oral ketoconazole has been used prophylactically in an attempt to reduce the incidence of fungal infections in cancer patients during periods of iatrogenic neutropenia but is not considered a good choice for antifungal prophylaxis.
The results of a limited number of studies in neutropenic cancer patients suggest that oral ketoconazole is more effective than placebo and at least as effective as oral nystatin in preventing fungal colonization and/or infection; however, some evidence indicates that it may predispose these patients to colonization with ketoconazole-resistant fungi.
The use of primary antifungal prophylaxis in cancer patients undergoing myelosuppressive therapy, bone marrow transplantation (BMT), or solid organ transplantation remains controversial. Such prophylaxis may predispose the patient to colonization with resistant fungi and/or result in the emergence of highly resistant organisms.
Therefore, many clinicians discourage primary prophylaxis with antifungal agents except in certain carefully selected high-risk patients in whom potential benefits are expected to justify possible risks (e.g., patients in institutions with a high incidence of fungal infections or circumstances where the frequency of systemic candidal infections is high). When primary antifungal prophylaxis is warranted in cancer patients, BMT patients, or solid organ transplant patients, oral fluconazole or, alternatively, IV amphotericin B is recommended.
Protozoal Infections
Acanthamoeba Infections
Oral ketoconazole has been used in conjunction with topical anti-infective agents (e.g., miconazole, neomycin, metronidazole, propamidine isethionate) in the treatment of Acanthamoeba keratitis. Optimum therapy for Acanthamoeba keratitis remains to be clearly established, but prolonged local and systemic therapy with multiple anti-infective agents and, often, surgical treatment (e.g., penetrating keratoplasty) are usually required. A regimen of oral ketoconazole, rifampin, and co-trimoxazole has been used successfully for the treatment of chronic Acanthamoeba meningitis in several immunocompetent children.
Leishmaniasis
Oral ketoconazole has been used to treat cutaneous or mucocutaneous leishmaniasis caused by Leishmania major (oriental sore), L. mexicana, L. panamensis, L. braziliensis, or L. tropica. Cutaneous leishmaniasis may subside spontaneously; however, treatment is generally required if lesions are disabling or disfiguring or fail to heal within 6 months or when dissemination to mucosal leishmaniasis is likely (e.g., L. braziliensis infections).

While pentavalent antimony compounds such as sodium stibogluconate (not commercially available in the US) or meglumine antimonate (not commercially available in the US) are generally considered the treatment of choice for cutaneous or mucocutaneous leishmaniasis, some clinicians suggest that IV amphotericin B (conventional or liposomal formulations) also is a drug of choice for these infections; alternative agents include IV or IM pentamidine, oral azole antifungal agents (e.g., itraconazole, ketoconazole), or topical paromomycin (for cutaneous leishmaniasis when there is a low potential for mucosal spread).
Ketoconazole has been used in a limited number of patients to treat antimony-resistant visceral leishmaniasis (kala-azar) caused by L.donovani; however, the drug appears to be less effective in these infections than in treating cutaneous leishmaniasis.
Prostate Cancer
Because of ketoconazole’s ability to inhibit testicular and adrenal steroid synthesis, the drug has been used in the treatment of advanced prostatic carcinoma. Ketoconazole has been used as a first-line agent in a few patients but is usually used as second-line hormonal therapy in patients with stage IV recurrent prostatic cancer. A limited number of patients with androgen-independent prostatic cancer have received ketoconazole in conjunction with doxorubicin. Ketoconazole has been used effectively as an adjunct in the acute management of disseminated intravascular coagulation (DIC) associated with prostatic carcinoma in a limited number of patients.
Hypercalcemia
Ketoconazole has been used with some success to treat hypercalcemia in adults with sarcoidosis. By competitively inhibiting the synthesis of 1,—dihydroxy vitamin D, ketoconazole may reduce elevated serum concentrations of the vitamin that may contribute to sarcoidosis-associated hypercalcemia.
Ketoconazole has been shown to produce a dose-dependent decrease in serum 1,-dihydroxyvitamin D concentrations in healthy individuals and hypercalcemic patients with primary hyperparathyroidism.
However, while ketoconazole generally decreases vitamin D serum concentrations, it has also reduced serum calcium concentrations in some, but not all, patients with sarcoidosis-associated hypercalcemia. In addition, hypercalcemia and increased serum 1—dihydroxy vitamin D concentrations may recur when the dosage of ketoconazole is decreased or the drug is discontinued.
Although corticosteroids are generally used to treat sarcoidosis-associated hypercalcemia, ketoconazole may be an alternative. It has also been effective in a few adolescents for the treatment of tuberculosis-associated hypercalcemia.
Acute Respiratory Distress Syndrome
In two small double-blind controlled trials, the development of acute respiratory distress syndrome (ARDS) and mortality rates were lower in high-risk patients given ketoconazole than in those given placebo. An accompanying editorial commented that adequate blood concentrations appeared to be essential. The mode of action could be associated with inhibition of leukotriene and thromboxane synthesis. Nevertheless, in a study of 234 patients, ketoconazole failed to reduce mortality or improve clinical outcomes when given early in the course of ARDS. Some centers have developed guidelines for ketoconazole prophylaxis in patients at risk of ARDS.
Endocrine Disorders and Malignant Neoplasms
Ketoconazole has been reported to impair steroid hormone synthesis and blunt the response of cortisone to adrenocorticotrophic hormone (ACTH) and has been tried in the management of a number of endocrine disorders. In Cushing’s syndrome, ketoconazole in doses of up to 1200 mg daily has been used successfully as an alternative or adjuvant to definitive therapies such as surgery or radiotherapy. Treatment of hirsutism is usually with an anti-androgen (see under Cyproterone), but ketoconazole has been tried in small numbers of women at a dose of 300 mg daily or 400 mg daily, with variable results.
Ketoconazole has been reported to produce a beneficial response in some forms of precocious puberty that do not generally respond to gonadorelin analogs. In small numbers of patients studied, cessation of menstruation and regression of pubertal signs in girls, reduced testosterone secretion, and an increase in adult height in boys have been noted.
The anti-androgenic effects of ketoconazole have also been found useful in the management of prostatic cancer in selected patients, although there have been some concerns about its tolerability, and it is not generally used as a first-line treatment. Ketoconazole was ineffective in suppressing postoperative erection in patients undergoing penile reconstructive surgery.
Other Uses
Ketoconazole has been used effectively for the palliative treatment of Cushing’s syndrome (hypercortisolism), including adrenocortical hyperfunction associated with adrenal or pituitary adenoma or ectopic corticotropin-secreting tumors. Ketoconazole has been used in a limited number of geriatric patients 75 years or older for the treatment of corticotropin-dependent Cushing’s syndrome and may provide an effective alternative in patients who cannot tolerate surgical treatment. Although further study is needed, ketoconazole has been used with some success in a limited number of patients for the treatment of dysfunctional hirsutism and in a limited number of boys for the treatment of precocious puberty.
Administration
Read side effects if you want cheap Ketoconazole with no prescription
Ketoconazole is administered orally. To ensure absorption in patients with achlorhydria, it has been recommended that each 200 mg of ketoconazole be dissolved in 4 mL of 0.2N hydrochloric acid solution or taken with 200 mL of 0.1N hydrochloric acid. The resultant solution should be administered via a plastic or glass straw to avoid contact with the teeth, and a glass of water should be administered immediately after the solution.
Alternatively, some clinicians have recommended that each 200 mg of ketoconazole be given with 680 mg or more of glutamic acid hydrochloride. Other clinicians have suggested that each 200 mg of ketoconazole be administered with an acidic beverage (e.g., Coca-Cola®, Pepsi®), or the dose can be dissolved in 60 mL of citrus juice to ensure absorption; however, this strategy may not be adequate in all patients with achlorhydria, and patients should be monitored closely for therapeutic failure.
Dosage
Fungal Infections
The usual initial adult dosage of ketoconazole recommended by the manufacturer is 200 mg once daily. For severe infections or if the expected clinical response is not achieved, the manufacturer states that the dosage may be increased to 400 mg once daily. Although data are limited regarding the use of ketoconazole in children, children older than 2 years of age have received a dosage of 3.3-6.6 mg/kg once daily; dosage has not been established for younger children.
Some clinicians recommend that ketoconazole be administered at a dosage of 400 mg once or twice daily to treat blastomycosis, coccidioidomycosis, or histoplasmosis. A dosage of 200 mg once or twice daily has also been used to treat histoplasmosis. A dosage of 200-400 mg daily has been recommended for the treatment of chromomycosis, paracoccidioidomycosis, or oropharyngeal and esophageal candidiasis.
For the treatment of uncomplicated vulvovaginal candidiasis in non-pregnant women, ketoconazole has been given at a dosage of 200-400 mg twice daily for 5 days. When used as a maintenance regimen to reduce the frequency of recurrent episodes of vulvovaginal candidiasis in women who have received an initial intensive antifungal regimen (i.e., 7-14 days of an intravaginal azole antifungal or a 2-dose fluconazole regimen), ketoconazole has been given at a dosage of 100 mg once daily for up to 6 months.
Children may be given about 3 mg/kg daily, 50 mg for those aged 1 to 4 years, and 100 mg for children aged 5 to 12 years. Treatment should usually be continued for 14 days and for at least one week after symptoms have cleared and cultures have become negative. Some infections may require several months of treatment, and giving ketoconazole for such prolonged periods may increase the risk of hepatotoxicity. A dose of 400 mg once daily for 5 days is used for the treatment of chronic vaginal candidiasis.
Ketoconazole is applied topically as a 2% cream in the treatment of candidal or dermatophyte infections of the skin, or in the treatment of pityriasis versicolor. It is used once or twice daily and continued for at least a few days after the disappearance of symptoms. A foam containing 2% ketoconazole applied twice daily for 4 weeks may be used in the treatment of seborrhoeic dermatitis. A shampoo containing 1 or 2% ketoconazole is also used. It is applied twice weekly for 2 to 4 weeks (or occasionally longer) in the treatment of dandruff for seborrhoeic dermatitis.
The 2% shampoo is used once daily for up to 5 days in pityriasis versicolor. For prophylaxis of seborrhoeic dermatitis, the 2% shampoo is used once every 1 to 2 weeks for prophylaxis of pityriasis versicolor. It may be used once daily for a maximum of 3 days before exposure to sunshine.
The duration of ketoconazole therapy depends on the infecting organism and the site and severity of the infection. Generally, therapy should be continued until clinical and mycologic tests indicate that the fungal infection has subsided. The usual duration of therapy for the treatment of candidiasis (including oral infections and candiduria) is 1-4 weeks, and the usual duration of therapy for chronic mucocutaneous candidiasis is 6-12 months.
Maintenance therapy may be necessary for the treatment of chronic mucocutaneous candidiasis. Prolonged therapy may also be needed for the treatment of chronic oral candidiasis, such as that associated with severe chronic xerostomia secondary to head and neck radiation therapy. The manufacturer states that paracoccidioidomycosis and histoplasmosis usually require a minimum of 6 months of therapy; however, 2-6 months of therapy have been effective in some patients.
Coccidioidomycosis, chromomycosis, and blastomycosis usually require 6-12 months of therapy.
Dermatophytoses have been successfully treated with 200-400 mg of ketoconazole daily for 1-2 months; however, tinea unguium (onychomycosis) may require at least 6-12 months of therapy.
Protozoal Infections
For the treatment of cutaneous, mucocutaneous, or visceral leishmaniasis (kala-azar), a ketoconazole dosage of 400-600 mg daily for 4-8 weeks has been used.
Prostate Cancer
For the treatment of prostatic carcinoma or as an adjunct in the management of disseminated intravascular coagulation (DIC) associated with prostatic carcinoma, a ketoconazole dosage of 400 mg every 8 hours has been used; however, the risk of depressed adrenocortical function at this high dosage should be considered.
Important Safety Information
Before buying Ketoconazole online, read information about the drug
Since ketoconazole has been reported to cause hepatotoxicity, it should not be given to patients with pre-existing liver disease. Patients given ketoconazole should be monitored for symptoms of hepatitis also, liver function tests should be performed before starting oral treatment with ketoconazole lasting for more than 14 days and then at least monthly throughout therapy. Ketoconazole has been shown to be teratogenic in animal studies and its use is generally not recommended during pregnancy.
Hypochlorhydria, which may be present in patients with AIDS, can reduce the absorption of ketoconazole. In this case absorption may be improved by giving ketoconazole with an acidic drink, such as a cola beverage.
Breastfeeding
Ketoconazole is excreted in breast milk, and licensed product information states that oral use should be avoided during breastfeeding. However, no adverse effects were seen in a breastfed infant whose mother was receiving ketoconazole. It was calculated that the infant was exposed to about 0.4%) of the usual therapeutic dose of ketoconazole for this age group. The American Academy of Pediatrics considers that the use of ketoconazole is, therefore, usually compatible with breastfeeding.
Porphyria
Ketoconazole is considered to be unsafe in patients with porphyria because it has been shown to be porphyrinogenic in in-vitro systems.
Adverse Effects
Read indications for use if you want to order Ketoconazole online
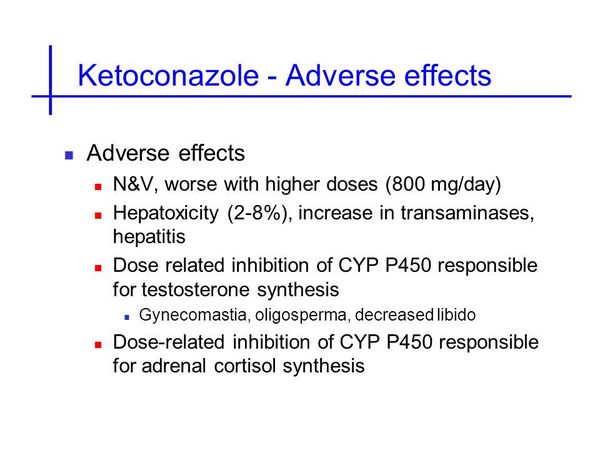
Gastrointestinal disturbances are the most frequently reported adverse effect after the oral use of ketoconazole. Nausea and vomiting have been reported in about 3% of patients, and abdominal pain in about 1%. These adverse effects are dose-related and may be minimized by giving ketoconazole with food. Asymptomatic, transient elevations in serum concentrations of liver enzymes may occur in about 10% of patients.
Hepatitis has been reported, and the risk appears to increase if treatment with ketoconazole is continued for longer than 2 weeks. It is usually reversible on stopping ketoconazole, but fatalities have occurred. Ketoconazole interferes with steroid biosynthesis, and adverse endocrine effects include gynaecomastia, oligospermia, menstrual irregularities, and adrenal cortex suppression, especially at high doses. Other adverse effects include allergic reactions such as urticaria and angioedema, and rare cases of anaphylaxis after the first dose have been reported. Pruritus, rash, alopecia, headache, dizziness, impotence, and somnolence may also occur. Thrombocytopenia, paraesthesia, raised intracranial pressure, and photophobia have been reported rarely. After topical use of ketoconazole, irritation, dermatitis, or a burning sensation has occurred.
Effects on the Blood
A case of fatal aplastic anemia was reported in a 23-year-old woman who had taken ketoconazole for 4 days for the treatment of vaginal discharge.
Effects on Endocrine Function
Oral ketoconazole blocks testosterone synthesis and adrenal response to corticotropin, resulting in azoospermia and oligospermia, gynecomastia, impotence, decreased libido, and adrenal insufficiency. As an inhibitor of steroid production, ketoconazole is valuable in controlling hypercortisolism and is used therapeutically in some endocrine disorders and prostatic cancer.
Effects on the Liver
Hepatic adverse reactions to oral ketoconazole are well known. About 10% of patients experience transient minor elevations of liver enzymes without clinical signs or symptoms of hepatic disease, which may occur at any stage of treatment. Although this reaction is not usually clinically important, it may signal the onset of more serious hepatic injury and indicate the need for close monitoring of liver function. Symptomatic hepatic reactions are much rarer (less than 0.1% of patients) but potentially fatal.
There is usually a hepatocellular pattern of damage and sometimes cholestasis. Patients at increased risk of hepatic injury include those with a history of liver disease, those aged over 50, especially women, and those requiring prolonged treatment. It is important to monitor liver function during treatment as well as to limit the length of treatment. if liver enzyme values continue to rise or jaundice or hepatitis occurs, ketoconazole should be withdrawn immediately since fatalities have occurred in patients who continued treatment after signs of hepatic injury developed.
Interactions
When you buy cheap Ketoconazole, you must know how to use it
The use of drugs that reduce stomach acidity, such as antimuscarinics, antacids, histamine H2-antagonists, and proton pump inhibitors, may reduce the absorption of ketoconazole. Absorption of ketoconazole may also be reduced by sucralfate. Enzyme-inducing drugs such as rifampicin, isoniazid, efavirenz, nevirapine, or phenytoin may reduce plasma ketoconazole concentrations. Concentrations of isoniazid and rifampicin may also be reduced by ketoconazole.
Ketoconazole inhibits certain hepatic oxidase enzymes, especially the cytochrome P450 isoenzyme CYP3A4, in a similar way to itraconazole, and similar care should be taken to avoid adverse effects due to increased plasma concentrations of the interacting drugs. A disulfiram-like reaction may occur in patients taking ketoconazole after drinking alcohol. The efficacy of oral contraceptives may be reduced. For reviews of drug interactions with azole antifungals, see Itraconazole.
Drugs Affecting Gastric Acidity
Because gastric acidity is necessary for the dissolution and absorption of ketoconazole, concomitant administration of drugs that decrease gastric acid output or increase gastric pH (e.g., antacids, cimetidine, ranitidine, antimuscarinics) may decrease absorption of the antifungal agent. In one study, administration of oral cimetidine 2 hours prior to administration of ketoconazole had no effect on the absorption of ketoconazole when the antifungal agent was administered as an acidified solution. In another study in healthy adults, concomitant administration of a single 400-mg oral dose of ketoconazole within 2 hours of an oral ranitidine 150-mg dose was associated with a reduction in ketoconazole bioavailability of approximately 95%; ranitidine had been administered in a dosage of 150 mg every 12 hours for 2 days prior to administration of ketoconazole.
Absorption of ketoconazole also appears to be reduced (e.g., by about 20%) by concomitant sucralfate administration; however, such reduced bioavailability of the drug does not appear to result from an elevation in gastric pH. If concomitant therapy with drugs that affect gastric acidity or with sucralfate is necessary during ketoconazole therapy, these drugs should be given at least 2 hours after ketoconazole tablets.
Hepatotoxic Drugs
Because ketoconazole can cause severe hepatotoxicity, patients receiving the antifungal agent concurrently with other potentially hepatotoxic drugs should be carefully monitored, especially those requiring prolonged therapy or with a history of liver disease.
Antituberculosis Agents
Concomitant administration of ketoconazole and rifampin has resulted in decreased serum concentrations of ketoconazole, and the manufacturer of ketoconazole recommends that the drugs not be administered concomitantly. In one patient receiving ketoconazole concomitantly with rifampin and isoniazid, serum concentrations of both rifampin and ketoconazole were decreased.
Although administration of ketoconazole 12 hours after the rifampin dose resulted in therapeutic serum concentrations of rifampin, serum concentrations of ketoconazole were subtherapeutic regardless of when the doses were given. In addition, isoniazid and rifampin appeared to have an additive effect in reducing serum ketoconazole concentrations.
Antiviral Agents
Although the clinical importance has not been determined, ketoconazole and acyclovir have shown dose-dependent, synergistic antiviral activity against herpes simplex virus types 1 and 2 (HSV-1 and -2) in in vitro replication studies. The combination of ketoconazole and vidarabine also showed interference, indifference, or antagonism in vitro against these viruses.
Quinolones
Norfloxacin may enhance the antifungal activity of antifungal agents (e.g., amphotericin B, flucytosine, ketoconazole, nystatin). There are conflicting reports on this interaction, however, and in at least one in vitro study, norfloxacin had no effect on the antifungal activity of amphotericin B. Further study is needed to evaluate the antifungal effect when norfloxacin is used in conjunction with an antifungal agent.
Cisapride
Concomitant administration of ketoconazole and cisapride is contraindicated. Ketoconazole appears to inhibit the metabolism of cisapride. Concomitant use of ketoconazole and cisapride has resulted in markedly elevated cisapride plasma concentrations and a prolonged QT interval. However, it has rarely caused serious cardiovascular effects, including ventricular tachycardia, ventricular fibrillation, and torsades de pointes.
Coumarin Anticoagulants
Like other imidazole derivatives, ketoconazole may enhance the anticoagulant effect of coumarin drugs. When ketoconazole is used concomitantly with these drugs, the anticoagulant effect should be carefully monitored, and the dosage of the anticoagulant adjusted accordingly.
Cyclosporine and Tacrolimus
Concomitant administration of ketoconazole and cyclosporine has been reported to increase plasma concentrations of cyclosporine and serum creatinine concentrations. It has been suggested that ketoconazole may interfere with the metabolism of cyclosporine via hepatic microsomal enzyme inhibition, although other mechanisms may also be involved.
When ketoconazole therapy is initiated in patients receiving cyclosporine, renal function and blood or plasma cyclosporine concentrations should be monitored. Some clinicians also recommend reducing the dosage or replacing it with another immunosuppressive agent. Patients stabilized on both drugs may require an increase in cyclosporine dosage when ketoconazole is discontinued. Concomitant administration of ketoconazole and tacrolimus may affect the metabolism of tacrolimus, resulting in increased plasma concentrations of the immunosuppressive agent.
Ketoconazole and tacrolimus should be used concomitantly with caution. Renal function and plasma concentrations of tacrolimus should be monitored, and dosage adjustment may be necessary.
Phenytoin
Concomitant administration of ketoconazole and phenytoin reportedly may alter the metabolism of one or both of the drugs, and serum concentrations of both drugs should be monitored if they are used concomitantly.
Theophylline
Concomitant administration of ketoconazole and theophylline has resulted in decreased serum theophylline concentrations in a limited number of patients. Data from a study in healthy adults, however, indicate that single or multiple oral doses of ketoconazole may not substantially alter the plasma clearance of single IV doses of theophylline (as aminophylline). Pending further data accumulation, serum theophylline concentrations, and the patient should be monitored closely, and the dosage of theophylline should be adjusted accordingly when ketoconazole is initiated or discontinued in patients receiving theophylline.
Terfenadine and Astemizole
Prolongation of the QT interval and QT interval corrected for rate (QTc), and rarely, serious cardiovascular effects, including arrhythmias (e.g., ventricular tachycardia, atypical ventricular tachycardia [torsades de pointes, ventricular fibrillation]), cardiac arrest, palpitations, hypotension, dizziness, syncope, and death, have been reported in patients receiving ketoconazole concomitantly with recommended dosages of terfenadine or astemizole, although these antihistamines are no longer commercially available in the US.
Ketoconazole has markedly inhibited the metabolism of astemizole or terfenadine, probably by inhibiting the cytochrome P-450 microsomal enzyme system. This results in increased plasma concentrations of unchanged drug (to measurable levels) and reduced clearance of the active desmethyl or carboxylic acid metabolite, respectively.
Such alterations in the pharmacokinetics of these antihistamines may have been associated with prolongation of the QT and QTc intervals. Similar alterations in the pharmacokinetics of these antihistamines and/or adverse cardiac effects have been reported in patients receiving the drugs concomitantly with itraconazole, although in vitro data suggest that itraconazole may have a less pronounced effect than ketoconazole on the pharmacokinetics of astemizole.
Therefore, astemizole and terfenadine have been contraindicated in patients receiving ketoconazole or itraconazole. It also has been recommended that these antihistamines not be used in patients receiving drugs that are structurally related to ketoconazole, including triazoles such as fluconazole, imidazoles such as miconazole (systemic preparations are no longer available in the US), and nitroimidazoles such as metronidazole.
Loratadine
In a limited number of individuals receiving ketoconazole dosages of 200 mg twice daily, concomitant administration of a single 20-mg dose of loratadine resulted in a 302% average increase of loratadine’s areas under the concentration-time curve (AUC), a 251% average increase in peak loratadine plasma concentrations, a 155% average increase of descarboethoxyloratadine’s (an active metabolite of loratadine) AUC, and a 141% average increase in peak descarboethoxyloratadine plasma concentrations compared with those achieved in individuals receiving loratadine and placebo.
No changes in the QTc intervals were reported 2, 6, and 24 hours after concomitant administration of the drugs and adverse effects were similar in individuals receiving loratadine concomitantly with ketoconazole and in those receiving loratadine and placebo.
Corticosteroids
Concomitant administration of ketoconazole and methylprednisolone or prednisolone may result in increased plasma concentrations of the corticosteroid, possibly due to decreased clearance of methylprednisolone or prednisolone. Ketoconazole may enhance the adrenal suppressive effects of corticosteroids. Dosage adjustment of corticosteroids may be needed when ketoconazole is administered concomitantly with these drugs.
Alcohol
Disulfiram reactions, including flushing, rash, peripheral edema, nausea, and headache, have occurred rarely in patients who ingested alcohol while receiving ketoconazole therapy but usually resolved within a few hours. Therefore, some clinicians recommend that alcohol be avoided during and for 48 hours after discontinuation of ketoconazole therapy.
Benzodiazepines
Concomitant administration of ketoconazole affects the pharmacokinetics of midazolam or triazolam, resulting in increased peak plasma concentrations and a prolonged plasma half-life of these benzodiazepines.
Because increased plasma concentrations of the drugs may result in potentiated and prolonged hypnotic and sedative effects, midazolam or triazolam should not be used concomitantly with ketoconazole.
Concomitant use of ketoconazole and triazolam is contraindicated. Special precaution is required if midazolam is administered parenterally to patients receiving ketoconazole because the sedative effect of midazolam may be prolonged with such concomitant administration.
Digoxin
Elevated plasma concentrations of digoxin have been reported in patients receiving ketoconazole. Although it is unclear whether concomitant use of ketoconazole caused these increased concentrations, digoxin concentrations should be monitored closely in patients receiving the antifungal agent.

Other Drugs
Severe hypoglycemia was reported when miconazole (a systemic preparation that is no longer commercially available in the US) was used concomitantly with an oral sulfonylurea antidiabetic agent. Because ketoconazole is structurally related to miconazole, the manufacturer states that the possibility that this interaction could occur with ketoconazole should be considered. In vitro studies indicate that ketoconazole can inhibit the metabolism of paclitaxel. Although this potential pharmacokinetic drug interaction has not been evaluated in humans, the manufacturer of paclitaxel states that caution should be exercised when paclitaxel and ketoconazole are used concomitantly.
Acute Toxicity
Although there have been no reports to date of the acute toxicity associated with overdosage of ketoconazole, the manufacturer states that in the event of overdosage, supportive measures, including gastric lavage with sodium bicarbonate, should be employed.
Storage
Ketoconazole tablets should be protected from moisture and stored in well-closed containers at 15-25°C.
Preparations
Ketoconazole Oral Tablets 200 mg Ketoconazole Tablets, (scored) Mutual Mylan Sidmak Teva United Research Nizoral®, (with povidone; scored) Jansse.
Ketoconazole Brand Names in Different Countries
| Country | Medication Names |
|---|---|
| Argentina | C-86; Cetonil; Eumicel; Faction; Fangan; Fitonal; Fungicil; Grenfung; Keduo; Ketogel; Ketole; Ketonazol; Ketozol; Krol; Micoespec K; Micoral; Orifungal; Perative; Quadion; Socosep; Tersoderm Plus; Tiki; Triatop |
| Australia | Daktagold; Hexal; Konazol Shampoo; Nizoral; Sebizole |
| Austria | Fungoral; Nizoral |
| Belgium | Docketoral; Nizoral |
| Brazil | Aciderm; Arcolan; Candiderm; Candoral; Cetocona; Cetoconalab; Cetohexal; Cetomed; Cetomicoss; Cetomizol; Cetonax; Cetoneo; Cetonil; Cetonin; Cetozan; Cetozaz; Cetozol; Fungoral; Ketomicol; Ketonan; Ketonazol; Lozan; Miconan; Micoral; Nizoral; Nizoretic; Noriderm; Noronal; Sioconazol; Tonazox; Zanoc; Zolmicol |
| Canada | Ketoderm; Nizoral |
| Chile | Arcolane; Biogel; Eprofil; Fungarest; Fungium; Ketonil; Soridermal; TKC |
| Czech Republic | Asquam; Nizoral; Orozanol |
| Denmark | Kezoral; Nizoral |
| Finland | Nizoral |
| France | Ketoderm; Ketolium; Nizoral |
| Germany | Nizoral; Terzolin |
| Greece | Abba; Adenosan; Aquarius; Botaderm; Cezolin; Ebersept; Flidaphen; Fungoral; llgem; Libroman; Mycofebrin; Neoegmol; Nyoxep; Scalpin; Sostatin; Vafluson |
| Hong Kong | Diazon; Fluzoral; Fungazol; Ketozol; Ketozole; Larry; Nizoral; Pristine; Pristinex; Sebizole; Stada K; Synizoral |
| Hungary | Ketospor; Nizoral |
| India | Arcolane; Danfree; Danru; Funazole; Fungicide; Hyphoral; Keto |
| Indonesia | Anfuhex; Dermaral; Dexazol; Dysfungal; Fexazol; Formyco; Funet; Fungasol; Fungoral; Interzol; Ketomed; Lusanoc; Micoticum; Muzoral; Mycoderm; Mycoral; Mycozid; Nizol; Nizoral; Nofung; Picamic; Profungal; Solinfec; Sporex; Thicazol; Wizol; Zoloral; Zoralin; Zumazol |
| Israel | Nizoral |
| Italy | Nizoral; Triatop |
| Malaysia | Dezor; Fungazol; Funginox; Ketozole; Kezoral; Larry; Nizoral; Pristine; Pristinex; Sebizole; Sunazol; Yucomy; Ziconal |
| Mexico | Akorazol; Apo-Kesol; Biozoral; Conazol; Cremosan; Ergomicon; Eurolat; Fungipar; Fungoral; Fungosine; Honzil; Keprobiozol; Kestomicol; Ketofar; Ketomed; Ketomizol; Ketoril; Konaderm; Konaturil; Lemyken; Lizovag; Lornazol; Messelzol; Mi-Ke-Sons; Micoser; Micozol; Mycodib; Nastil; Nazol-farm; Nazoltec; Nizoral; Onofin-K; Prenalon; Remecon; Strizole; Termizol; Tiniasil; Tiniazol; Tocomizol; Toconal; Tolcrem; Tomiko; Triatop |
| The Netherlands | Nizoral |
| Norway | Fungoral; Konazal |
| New Zealand | Daktagold; Ketopine; Nizoral; Sebizole |
| Philippines | Ketovid; Nizoral |
| Poland | Fungores; Nizoral; Noell |
| Portugal | Farmorol; Frisol; Frisolac; Micopar; Nizale; Nizoral; Rapamic; Tedol |
| Russia | Livarole; Mycosoral; Nizoral |
| South Africa | Adco-Dermed; Ketazol; Kez; Nizcreme; Nizoral; Nizorelle; Nizovules; Nizshampoo |
| Singapore | Antanazol; Beatoconazole; Dezor; Dezoral; Dia-zon; Ketozole; Kezoral; Nicozone; Nitozol; Nizoral; Pristine; Pristinex; Pro-fungal; Sebizole; Yucomy |
| Spain | Fungarest; Fungo Farmasierra; Fungo Zeus; Keto-Cure; Ketoderma; Ketoisdin; Medezol; Micoticum; Panfungol |
| Sweden | Fundan; Fungoral; Ketoson |
| Switzerland | Ketozol; Nizoral; Terzolin |
| Thailand | AC-FA; Chintaral; Dezor; Diazon; Fungazol; Fungiderm-K; Funginox; Kara; Katsin; Kazinal; Kenalyn; Kenazol; Kenazole; Kenoral; Ketazol; Ketazon; Ketocine; Ketolan; Ketomed; Ketonazole; Ketoral; Ketosil; Ketozal; Kezon; Konazol; Lama; Larry; Manoketo; Masarol; Mizoron; Mycella; Myco; Mycoral; Ninazol; Nizoral; Nora; Pasalen; Sporaxyl; Sporoxyl; Triatop |
| Turkey | Fungoral; Ketoral; Konazol; Nizoral |
| UK | Dakiarin Gold; Dandrazol; Dandrid; Nizoral |
| USA | Extina; Nizoral; Xolegel |
| Venezuela | Arcolane; Dan-free; Freetop; Kenazol; Ketazol; Ketocoval; Ketomed; Napox; Nizoral; Noractin; Topstar |
Multi-ingredient
| Country | Medication Names |
|---|---|
| Argentina | Aeromicrosona of Bactisona; Ciprocort; Dercotex Duo; Minoxi; Gentacler; Gynerium; Ketohair; Linfol Dermico; Micozol Compuesto; Microsona C; Ovogin; Prurisedan Biotic; Start NP; Torgyn Duo; Tricur; Tridermal; Triefect |
| Brazil | Betazol Cort; Candicort; Capel; Celocort; Cetobeta; Cetocort; Cetocorten; Cimecort; Emscort; Naderm; Novacort; Trok; Trok-N |
| Chile | KPL |
| India | Hyphoral; Scalpe |
| Italy | Keto Z; Ketomousse |
| Malaysia | Ketoplus |
| Mexico | Femisan; Gynoclin-V; Trexen Duo |
| Philippines | Scalpex |
| Russia | Keto Plus |
| USA | Xolegel Duo |
Dosage and Forms of Ketoconazole
Before purchasing Ketoconazole, you must read how to store tablets
| Dosage forms of Ketoconazole: | |||
|---|---|---|---|
| Ketoconazole 2% cream | Nizoral 2% cream | Apo-Ketoconazole 200 mg Tablet | Novo-Ketoconazole 200 mg Tablet |
| Nu-Ketocon 200 mg Tablet | Kuric 2% cream | Ketoconazole 200 mg tablet | Extina 2% foam |
| Nizoral 200 mg tablet | Ketoconazole powder | Ketoconazole 2% Cream 15 gm Tube | Ketoconazole 2% Shampoo 120ml Bottle |
| Ketoconazole 2% Cream 30 gm Tube | Ketoconazole 2% Cream 60 gm Tube | Nizoral 2% Shampoo 120ml Bottle | Extina 2% Foam 50 gm Can |
| Extina 2% Foam 100 gm Can | Nizoral a-d 1% shampoo | Ketoconazole 2% shampoo | Ketoderm 2 % Cream |
Synonyms of Ketoconazole
2%, Ketocanazole, Ketoconazol, Ketoconazol [INN-Spanish], Ketoconazole, Ketoconazole [Usan:Ban:Inn:Jan], Ketoconazolum [INN-Latin]
How can I get Ketoconazole online over the counter?
You can buy Ketoconazole OTC in the online drugstore at a low cost.
Therapeutic classes of Ketoconazole
Antifungal Agents, Antifungals
Delivery
Australia, Canada, Mexico, New Zealand, USA, Europe [Belgium, France, Norway, Holland, Ireland, Spain, Switzerland, Great Britain (UK), Italy] and etc.



 (24 votes, average: 3.92 out of 5)
(24 votes, average: 3.92 out of 5)
















