Terbinafine is an infective / antifungal agent that inhibits squalene epoxidase, resulting in ergosterol deficiency and a corresponding accumulation of squalene within the fungal cell leading to fungal cell death. It is indicated in the treatment of onychomycosis of the toenail or fingernail caused by dermatophytes.
Topical: used in interdigital tinea pedis, tinea cruris, or tinea corporis caused by E. floccosum, T. mentagrophytes, or T. rubrum.
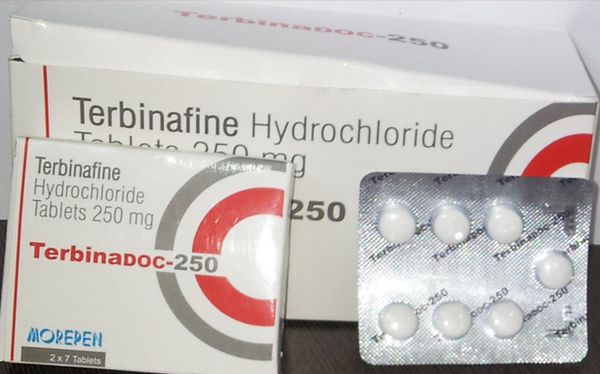
Terbinafine (Lamisil) 250mg tablets is a synthetic allylamine, structurally similar to the topical agent naftiflne.
Terbinafine (Lamisil) 250mg tablets is well absorbed, but bioavailability is decreased to about 40% because of first-pass metabolism in the liver. Proteins bind more than 99% of the drug in plasma. Drug accumulates in skin, nails, and fat. The initial half-life is about 12 hours but extends to 200 to 400 hours at steady state. Drug can be found in plasma for 4 to 8 weeks after prolonged therapy.
Terbinafine is not recommended in patients with marked azotemia or hepatic failure, because in the latter condition, terbinafine plasma levels are increased by unpredictable amounts. Rifampin decreases and cimetidine increases plasma terbinafine concentrations. The drug is well tolerated, with a low incidence of gastrointestinal distress, headache, or rash. Rarely, hepatotoxicity, severe neutropenia, Stevens-Johnson syndrome, or toxic epidermal necrolysis may occur. The drug is contraindicated in pregnancy. It is recommended that systemic terbinafine therapy for onychomycosis be postponed until after pregnancy is complete. Its mechanism of action is probably inhibition of fungal squalene epoxidase, blocking ergosterol biosynthesis.
Terbinafine (Lamisil) 250mg, given as one 250-mg tablet daily, is at least as effective for nail onychomycosis as 200 mg daily of itraconazole, and slightly more effective than pulse itraconazole therapy (see above). Duration of treatment varies, with the site being treated but typically is 3 months. Although not approved for this use, terbinafine (250 mg daily) also is effective in ringworm elsewhere on the body. No pediatric formulation is available, so there is little experience with the drug in tinea capitis, usually a disease of children.
Terbinafine (Lamisil) 1% cream or spray is applied twice daily and is effective in tinea corporis, tinea cruris, and tinea pedis. Terbinafine is less active against Candida species and Malassezia furfur, but the cream also can be used in cutaneous candidiasis and tinea versicolor. In European studies, oral terbinafine has appeared to be effective in treatment of ringworm, and in some cases of onychomycosis. The systemic use of terbinafine is discussed above.
Terbinafine Hydrochloride: Uses
Onychomycosis
Terbinafine is used orally in the treatment of dermatophytic infections of the toenail or fingernail (onychomycosis, tinea unguium) caused by susceptible fungi. Prior to administration of oral terbinafine, appropriate nail specimens for microbiologic studies (e.g., potassium hydroxide [KOH] preparation, fungal culture, or nail biopsy) should be obtained to confirm the diagnosis of onychomycosis. The optimal clinical effect of terbinafine in the treatment of onychomycoses is seen several months after mycologic cure and completion of treatment, and is related to the period required for outgrowth of healthy nail.
Because terbinafine is highly lipophilic and keratophilic, the drug distributes in high concentrations into the stratum corneum, sebum, hair, and nail matrix, bed, and plate, persisting in these tissues for several weeks to months after discontinuance of the drug. Toenail infections generally require more prolonged terbinafine therapy than do fingernail infections.
Efficacy of terbinafine has been established in uncontrolled and placebo- or comparative drug-controlled studies in patients with toenail or fingernail onychomycosis. In these studies, patients were assessed for mycologic cure (negative observation of fungus in lesion scrapings prepared with potassium hydroxide, and negative culture of lesion scrapings), effective treatment (mycologic cure and either no nail involvement or more than 5 mm of unaffected new nail growth), or mycologic and clinical (no nail involvement) cure. Terbinafine has been shown to be active against most strains of Trichophyton rubrum and T. mentagrophytes both in vitro and in clinical infections of the nail. Although terbinafine is active in vitro against most strains of Epidermophyton floccosum, Candida albicans, and Scopulariopsis brevicaulis, efficacy of the drug in the treatment of onychomycosis caused by these organisms remains to be established in controlled clinical studies.
In the toenail studies, 12 weeks of oral therapy with terbinafine 250 mg daily was more effective than placebo or itraconazole 200 mg daily, and 16 weeks of oral terbinafine therapy at this dosage was more effective than up to 52 weeks of oral griseofulin 500 mg daily. In these studies, 70-88% of patients experienced mycologic cure, 59% experienced effective treatment, and 38-57% experienced mycologic and clinical cure when evaluated 36-48 weeks after completion of terbinafine treatment; the clinical relapse rate was about 15% in those evaluated at least 6 months after experiencing clinical cure and at least 1 year after completion of terbinafine treatment.
In a study comparing 4 months of continuous (250 mg daily) or intermittent (500 mg daily for 1 week each month) oral terbinafine or intermittent (400 mg daily for 1 week each month) oral itraconazole, a trend favoring continuous terbinafine therapy was observed, but statistically significant differences in cure rates among the regimens were not observed. In a treatment duration-ranging study comparing 6-, 12-, and 24-weeks of terbinafine therapy in patients with toenail infections, mycologic cure rates were substantially greater for the 12- or 24-week regimens compared with the 6-week regimen, but the 24-week regimen was not substantially more effective than the 12-week regimen. However, some patients who do not respond to an initial 12-week course of terbinafine therapy may respond to a second course with the drug.
In the fingernail studies, 75% of patients experienced effective treatment, and 59-90% of patients experienced mycologic and clinical cure when evaluated 18-42 weeks after completion of treatment with oral terbinafine 250 mg daily for 6 weeks. Extending the course of terbinafine therapy to 12 weeks in patients with fingernail infections does not appear to improve response substantially. In a study in patients with fingernail onychomycosis who received oral terbinafine 250 mg daily for 2 or 4 weeks, 65% exhibited mycologic and clinical cure 6 months after completion of therapy; the cure rate in those who received only 2 weeks of therapy was 45%.
Terbinafine may be particularly useful in patients who cannot tolerate azole antifungal agents (e.g., itraconazole) or when there are concerns regarding possible drug interactions between azole antifungal agents and other drugs the patient is receiving.
However, liver failure (sometimes leading to death or liver transplant) has occurred rarely in patients with or without preexisting liver disease who were receiving terbinafine for the treatment of onychomycosis. Most reports of liver failure occurred in patients with serious underlying systemic conditions, and a causal relationship to terbinafine has not been established. The severity of the adverse hepatic effects and/or the outcome of such effects may be worse in patients with active or chronic liver disease and terbinafine therapy is not recommended in such patients. Prior to administration of oral terbinafine, presence of liver disease should be assessed; pretreatment determination of serum concentrations of ALT (SGPT) and AST (SGOT) is advised for all patients.
Terbinafine should be discontinued if biochemical or clinical signs of liver injury develop during therapy. Patients should be instructed to report any signs or symptoms of liver dysfunction, such as persistent nausea, anorexia, fatigue, vomiting, right upper abdominal pain or jaundice, dark urine, pale stools; patients with these signs/symptoms should discontinue terbinafine and have their liver function immediately evaluated. Terbinafine also may be associated with other intolerable adverse effects (e.g., taste or ocular [lenticular, retinal] disturbances, hematologic [decreases in absolute lymphocyte count, neutropenia] effects, serious skin reactions), and the choice of antifungal therapy for the treatment of onychomycosis should be individualized. Weighed in this consideration should be the prolonged (several months) nature and cost of therapy, and the possibility of relapse of onychomycosis.
Tinea Capitis and Tinea Corporis
Oral terbinafine has been used for the treatment of tinea capitis or tinea corporis. Although safety and efficacy of oral terbinafine in pediatric patients have not been established, the drug has been used with some success for the treatment of tinea capitis in adults and children 14 months of age or older.Preliminary data to date indicate that while oral terbinafine may be effective for the treatment of tinea capitis caused by Trichophyton, the drug appears to be considerably less effective (and may be ineffective) when the infection is caused by Microsporum.
Terbinafine: Organs and Systems
Sensory systems
Taste disturbance is a rare adverse effect of terbinafine. It is usually reversible, with a median time to recovery of 42 days. However, a 46-year-old woman had complete loss of taste after taking oral terbinafine, with persistent taste disturbances for 3 years after stopping the drug.
Hematologic
The projected rate of all blood dyscrasias associated with terbinafine has been estimated to be 32 per million patient-years. Pancytopenia has been reported.
Leukocytes
Neutropenia has been reported in patients taking terbinafine.
- A 55-year-old woman who was taking terbinafine and paroxetine presented with fever, diarrhea, and vomiting. A bone marrow biopsy showed overall reduced cellularity, and the aspirate showed a profound shift toward the production of immature myeloid cells, consistent with maturation arrest. Treatment consisted of withdrawal of all outpatient medications, hydration, intravenous fluids, broad-spectrum antibiotics, and G-CSF 5 µg/kg for 5 days. Mature granulocytes appeared in the peripheral blood on the fifth day in hospital, and she was discharged on the seventh hospital day with an absolute neutrophil count of 6.2 x 109/1. Paroxetine was resumed weeks after discharge from hospital without hematological toxicity over 6 months.
- A 60-year-old man presented with fever, oral mucositis, pedal cellulitis, and bacteremia after a 6-week course of terbinafine 250 mg. He was taking concurrent yohimbine for impotence. Bone marrow examination showed a hypocellular marrow with myeloid maturation arrest. Treatment consisted of withdrawal of outpatient medications, broad-spectrum antibiotics, hydration, and G-CSF, and was ultimately successful. Yohimbine was resumed later without any adverse effects.
- A 42-year-old man presented with fever and granulocytopenia (absolute neutrophil count: 340 x 106/1; temperature: 39.5°C) after a 30-day course of oral terbinafine 250 mg/day for presumed onychomycosis. The granulocyte count recovered promptly after withdrawal of the drug and administration of G-CSF for 2 days.
- Agranulocytosis occurred in a 15-year-old who took terbinafine 250 mg/day for toenail onychomycosis and tinea pedis. This effect was noted 4 weeks after starting terbinafine and resolved within 1 week after its withdrawal.
Platelets
Thrombocytopenia has been attributed to terbinafine, and the incidence has been estimated at 1 in 200 000 patients.
- A 25-year-old Yemeni woman with familial-ethnic leukopenia developed thrombocytopenia with epistaxis after taking terbinafine 250 mg for 4 weeks. The platelet count recovered from a nadir of 63 x 109/1 to 314 x 109/1 after drug withdrawal.
- A 53-year-old woman developed severe thrombocytopenia after a 6-week course of terbinafine (250 mg/day) for onychomycosis. A bone marrow aspirate showed a normocellular marrow. She received a platelet transfusion and recovered after a short course of prednisolone.
Mouth
- A 38-year-old man presented with acute right otitis media and unrelated painless bilateral enlargement of the parotid glands 15 days after taking oral terbinafine for tinea cruris. He stopped taking terbinafine and 12 days later the swelling had significantly abated and completely disappeared 4 weeks later.
Liver
Minor abnormalities in liver function tests have been reported in up to 4% of patients taking oral terbinafine, but have not generally been considered clinically important. Terbinafine can cause hepatitis, with an estimated rate of about 1 in 50 000. Idiosyncratic reactions can lead to liver cell necrosis as well as cholestasis. Prolonged cholestatic hepatitis and liver failure have been reported.
- In four patients with cholestatic hepatitis associated with terbinafine, all presented with jaundice and direct hyperbilirubinemia, various other clinical signs of hepatitis, and mild to moderate rises in alkaline phosphatase and hepatic transaminase activities. Biopsies in two patients showed cellular infiltrates in the portal tracts and hepatocellular and canalicular cholestasis and hepatocyte degeneration. In the two cases with long-term follow-up, hepatitis was reversible after withdrawal of terbinafine and liver tests normalized within 6 months.
- A 41-year-old man developed severe hepatic dysfunction following a 3.5-week course of terbinafine (250 mg/ day). He had marked pruritus, jaundice, malaise, anorexia, and loin pain. His serum bilirubin rose to a peak of 718 µmol/l with alkaline phosphatase 569 U/l, alanine transaminase 90 U/l, aspartate transaminase 63 U/l, and a prolonged prothrombin time of 21 seconds, unresponsive to vitamin K. Liver biopsy showed canalicular cholestasis consistent with a drug reaction. His symptoms resolved 11 months after drug withdrawal, and his liver function tests normalized after 15 months.
- A previously healthy 46-year-old man developed acute fulminant hepatitis following treatment with rabepra-zole, citalopram hydrobromide, terbinafine, and a mul-tivitamin formulation. Liver biopsy showed submassive centrilobular necrosis and intrahepatic cholestasis with florid bile duct proliferation.
In the last case, because of the similarity of the clinical, laboratory, and histological effects of omeprazole and lansoprazole, as previously reported, the authors concluded that the reaction in the second patient might have been caused by the proton pump inhibitor rather than terbinafine.
- A 56-year-old woman developed chronic biliary ductopenia and portal fibrosis 2 years after a course of terbinafine. Terbinafine treatment at that time had resulted in jaundice and evidence of cholestasis. After withdrawal of terbinafine, she continued to have pruritus and persistently raised serum alkaline phosphatase activity. Investigations for various types of chronic liver disease were negative and so chronic bile duct loss and periportal fibrosis were attributed to terbinafine.
Because of the rare and unpredictable nature of hepatobiliary reactions to terbinafine, the mechanism of hepatotoxicity has been hypothesized to be either immu-nological or metabolically mediated. A potentially toxic reactive metabolite of terbinafine, 7,7-dimethylhept-2-ene-4-ynal (TBF-A), the N-dealkylation product of terbinafine, has been identified in vitro. The authors speculated that this allylic aldehyde metabolite, formed by liver enzymes and conjugated with glutathione, would be transported across the canalicular membrane of hepatocytes and concentrated in the bile. The reactive monoglutathione conjugate could bind to hepatobiliary proteins and cause direct toxicity. Alternatively, it could modify canalicular proteins and lead to an immune-mediated reaction, causing cholestatic dysfunction.
Skin
Cutaneous adverse effects reportedly occur in 1-3% of patients taking terbinafine. The overwhelming majority of these reactions consist of mild to moderate macular exanthemas.
The risk of serious skin disorders has been estimated in 61 858 users of oral antifungal drugs, aged 20-79 years, identified in the UK General Practice Research Database. They had received at least one prescription for oral fluconazole, griseofulvin, itraconazole, ketoconazole, or terbinafine. The background rate of serious cutaneous adverse reactions (corresponding to non-use of oral anti-fungal drugs) was 3.9 per 10 000 person-years (95% CI = 2.9). Incidence rates for current use were 15 per 10 000 person-years (for itraconazole, 11.1 (3 for terbinafine, 10 for fluconazole, and 4.6 for griseofulvin. Cutaneous disorders associated with the use of oral antifungal drugs in this study were all mild.
Generalized rashes, fixed drug eruptions, toxic epidermolysis, and erythema exudativum multiforme have all been reported in association with terbinafine.
Pustular eruptions can occur occasionally.
- Acute generalized exanthematous pustulosis associated with terbinafine has been described in two patients. Both presented within 7-10 days after starting to take terbinafine with generalized pustular dermatosis and leukocytosis; fever was a presenting symptom in one patient. Treatment with systemic corticosteroids was successful in both cases.
- A 62-year-old diabetic man on stable oral medication with glibenclamide, metformin, Zestoretic (lisinopril + hydrochlorothiazide), gemfibrozil, and aspirin developed febrile generalized pustular eruptions after 44 days of therapy with oral terbinafine 250 mg/day. Withdrawal of terbinafine and symptomatic treatment with hydrotherapy and topical and systemic steroids resulted in complete resolution of fever and pustulosis within 4 days. The erythematous component responded more slowly, and mildly pruritic erythematous plaques persisted for more than 40 days.
- In another case of acute generalized exanthematous pustulosis attributed to terbinafine (250 mg/day), epicutaneous and intracutaneous skin tests were negative, and there was no evidence of viral infection.
Terbinafine can cause or exacerbate psoriatic lesions.
- Severe pustular psoriasis provoked de novo by oral terbinafine has been reported in a 65-year-old man 2 weeks after the start of therapy for onychomycosis. Treatment of psoriasis was complicated and ultimately required continuous systemic and topical antipsoriatic therapy.
- A 74-year-old woman developed inverse psoriasis after 14 days of therapy with terbinafine 250 mg/day for onychomycosis. The lesions resolved almost completely on withdrawal of terbinafine and topical therapy.
Probable psoriatic onychodystrophy, misdiagnosed as onychomycosis and treated with terbinafine, induced inverse psoriasis in the second case, underscoring the importance of mycological confirmation of onychomycosis before therapy.
Ten cases of severe skin reactions probably associated with terbinafine requiring drug withdrawal have been reported: erythema multiforme, erythroderma, severe urticaria, pityriasis rosea, and worsening of pre-existing psoriasis. All the patients made an uneventful recovery with appropriate therapy. The authors pointed out that patients should be counselled about discontinuing terbinafine at the onset of a skin eruption and about seeking medical advice about further management.
- Cutaneous lupus erythematosus attributed to terbinafine has been reported in two previously healthy women. In the first patient, the lesions improved but did not resolve completely; in the second the symptoms resolved completely with appropriate therapy and the patient remained disease-free after withdrawal of all medication.
- Another woman with a previous history suggestive of lupus erythematosus developed a widespread flare in her skin 1 week after starting oral terbinafine. The eruption ultimately responded to systemic treatment with corticosteroids.
Baboon syndrome has been attributed to terbinafine.
- A 26-year-old man developed a fixed drug eruption on his hands and inguinal and gluteal areas after oral treatment of onychomycosis with terbinafine 250 mg/day. The rash showed the characteristic distribution of the baboon syndrome. Although epicutaneous and intracutaneous tests were negative, the rash recurred 20 hours after oral rechallenge with terbinafine.
The underlying pathogenic mechanism for the baboon syndrome has been suggested to be a systemically induced allergic contact dermatitis.
Hair
Hair loss has been attributed to terbinafine.
- A 69-year-old woman took terbinafine 250 mg/day for 112 days for subungual hyperkeratosis and developed hair loss after 3 months. She was also taking hydrochlorothiazide, amiloride hydrochloride, and amlodipine besilate, all in the same dosage for more than 5 years. Clinical and laboratory investigations showed no other obvious causes, and hair loss completely reversed on withdrawal of terbinafine.
Musculoskeletal
Since its introduction, the Netherlands Pharmacovigilance Foundation Lareb has received eight reports of arthralgia in patients taking terbinafine. In four cases, skin reactions were also present and in two cases urticaria. Two patients who reported arthralgia also had a fever. Logistic regression modelling showed that both urticaria and arthralgia were statistically significantly associated with reports on terbinafine compared with all other reports in the database. These findings may point toward a clustering of these symptoms in patients using terbinafine, suggesting a shared immunological reaction.
Immunologic
Exacerbation of lupus erythematosus has been reported during terbinafine therapy. Of 21 consecutive patients with subacute cutaneous lupus erythematosus who attended an outpatient dermatology department in Germany during 1 year, 4 had terbinafine-associated disease. In addition to high titers of antinuclear antibodies with a homogeneous pattern, anti-Ro(SS-A) antibodies were present; in three of the four women, anti-La(SS-B) antibodies were also found. All the patients had antihistone antibodies, as in drug-induced lupus, and showed the characteristic genetic association with the HLA-B8,DR3 haplotype; moreover, in two cases HLA-DR2 was also present. After withdrawal of terbinafine, antinuclear antibody titers fell and antihistone antibodies became undetectable within 4.5 months in three patients.
- A 66-year-old man with giant cell arteritis and hypertension developed a hypersensitivity reaction 4.5 weeks after starting to take terbinafine, with a skin eruption, fever, lymphadenopathy, and hepatic dysfunction. Concomitant medications included prednisone, doxazosin, and aspirin. His symptoms and signs resolved within 6 weeks after withdrawal of terbinafine and continuation of all the other medications. The hypersensitivity syndrome reaction in this case was idiosyncratic, with no apparent predisposing factors.
| Dosage forms of Terbinafine: | |||
|---|---|---|---|
| Lamisil 1% cream | Apo-Terbinafine 250 mg Tablet | Co Terbinafine 250 mg Tablet | Mylan-Terbinafine 250 mg Tablet |
| Novo-Terbinafine 250 mg Tablet | Pms-Terbinafine 250 mg Tablet | Sandoz Terbinafine 250 mg Tablet | Lamisil 250 mg Tablet |
| Terbinafine hcl 250 mg tablet | Lamisil 250 mg tablet | Terbinafine HCl 1% Cream 24 gm Tube | Terbinafine hcl powder |
| LamISIL 1% Solution 30ml Bottle | LamISIL 14 187.5 mg Packets Packet | Lamisil af defense 1% powder | Lamisil antifungal 1% spray |
| Lamisil af defense crm to powd | Athlete’s 1% foot cream | CVS Pharmacy athlete’s foot 1% cream | CVS Pharmacy jock itch 1% cream |
| Lamisil at 1% cream | Sm athlete’s 1% foot cream | Lamisil 1 % Cream | Lamisil 1 % Solution |
Synonyms of Terbinafine:
Terbinafine, Terbinafine HCl, Terbinafine Hydrochloride, Ternbinafine HCl
How can i get Terbinafine online over the counter?
You can buy Terbinafine OTC in online drugstore with low cost.
Therapeutic classes of Terbinafine:
Allylamines, Antifungal Agents, Antifungals, Enzyme Inhibitors, Trypanocidal Agents
Delivery
Australia, Canada, Mexico, New Zealand, USA, Europe [Belgium, France, Norway, Holland, Ireland, Spain, Switzerland, Great Britain (UK), Italy] and etc.



 (46 votes, average: 3.63 out of 5)
(46 votes, average: 3.63 out of 5)
















