Cycloserine
Cycloserine, a structural analog of the amino acid d-alanine, is an antituberculosis antibiotic.
Uses
Tuberculosis
Active Tuberculosis
Cycloserine is used in conjunction with other antituberculosis agents in the treatment of clinical tuberculosis.
The American Thoracic Society (ATS), US Centers for Disease Control and Prevention (CDC), and Infectious Diseases Society of America (IDSA) currently recommend several possible multiple-drug regimens for the treatment of culture-positive pulmonary tuberculosis. These regimens have a minimum duration of 6 months (26 weeks), and consist of an initial intensive phase (2 months) and a continuation phase (usually either 4 or 7 months).
Cycloserine is considered a second-line antituberculosis agent for use in these regimens. The drug usually is used in the treatment of drug-resistant tuberculosis caused by Mycobacterium tuberculosis known or presumed to be susceptible to the drug. If cycloserine is added as a new drug to a regimen in patients experiencing treatment failure who have proven or suspected drug-resistant tuberculosis, at least 2, preferably 3, new drugs known or expected to be active against the resistant strain should be added at the same time. After results of in vitro susceptibility testing are available, the regimen can be adjusted accordingly.
Urinary Tract Infections
Cycloserine has been used in the treatment of acute urinary tract infections caused by susceptible bacteria, especially E. coli or Enterobacter. However, cycloserine is less effective than other drugs in the treatment of urinary tract infections caused by gram-positive or gram-negative bacteria, and the drug should be used in these infections only when other more effective and less toxic alternatives are contraindicated and susceptibility of the organism to cycloserine has been demonstrated.
Administration
Cycloserine is administered orally.
Dosage
Active Tuberculosis
In the treatment of clinical tuberculosis, cycloserine should not be given alone. The drug is considered a second-line agent for use in daily multiple-drug regimens for the treatment of active tuberculosis. Data are not available to date regarding use of cycloserine in intermittent multiple-drug regimens used in the treatment of tuberculosis. Therapy for tuberculosis should be continued long enough to prevent relapse. The minimum duration of treatment currently recommended for patients with culture-positive pulmonary tuberculosis is 6 months (26 weeks), and recommended regimens consist of an initial intensive phase (2 months) and a continuation phase (usually either 4 or 7 months). However, completion of treatment is determined more accurately by the total number of doses and is not based solely on the duration of therapy. For information on general principles of antituberculosis therapy and recommendations regarding specific multiple-drug regimens and duration of therapy.
The manufacturer states that the usual adult dosage of cycloserine for use in conjunction with other antituberculosis agents is 250 mg every 12 hours for the first 2 weeks; dosage should be adjusted to maintain blood concentrations of the drug at less than 30 mcg/mL. Most adults receive 500 mg to 1 g daily administered in equally divided doses; higher dosages are not recommended.
The American Thoracic Society (ATS), US Centers for Disease Control and Prevention (CDC), and Infectious Diseases Society of America (IDSA) state that the usual dosage of cycloserine for use in conjunction with other antituberculosis agents in adults and children 15 years of age or older is 10-15 mg/kg (up to 1 g) daily given in 2 divided doses. These experts recommend 500-750 mg daily and note that there is evidence that toxicity is more common at dosages exceeding 500 mg daily. In addition, they state that optimum dosage can be determined by maintaining peak cycloserine serum concentrations of 20-35 mg/mL.
The manufacturer states that safety and optimum dosage of cycloserine for children have not been established. The ATS, CDC, IDSA, and American Academy of Pediatrics (AAP) state that pediatric patients may receive cycloserine in a dosage of 10-20 mg/kg (up to 1 g) daily.
Urinary Tract Infections
In the treatment of acute urinary tract infections, the usual adult dosage of cycloserine is 250 mg every 12 hours for 2 weeks.
Dosage in Renal Impairment
Dosage of cycloserine in patients with renal impairment must be adjusted according to the degree of dysfunction and blood cycloserine concentrations.
Cautions
Adverse Effects
The most frequent adverse effects of cycloserine involve the nervous system. Drowsiness, somnolence, dizziness, headache, lethargy, depression, tremor, dysarthria, hyperreflexia, paresthesia, nervousness, anxiety, vertigo, confusion and disorientation with loss of memory, paresis, major and minor clonic seizures, convulsions, and coma have been reported in patients receiving the drug.
Frequent ingestion of alcohol appears to increase the risk of seizures during cycloserine therapy. Psychosis (possibly with suicidal tendencies), personality changes, hyperirritability, and aggression have also occurred in patients receiving the drug. Adverse nervous system effects appear to be dose related and occur within the first 2 weeks of therapy in about 30% of patients receiving 500 mg of cycloserine daily; symptoms generally disappear when the drug is discontinued. Adverse nervous system effects are minimized when blood cycloserine concentrations do not exceed 30 mcg/mL.
If symptoms of neurotoxicity occur, dosage should be reduced or the drug should be discontinued. Some of the neurotoxic effects may be relieved or prevented by the concomitant administration of 100-300 mg of pyridoxine hydrochloride daily in divided doses. Sedatives may be effective in controlling anxiety or tremor, and anticonvulsants may control convulsions.
Rarely, hypersensitivity reactions including rash and photosensitivity have occurred with cycloserine. Cardiac arrhythmias and sudden development of congestive heart failure have been reported rarely in patients receiving 1-1. g of the drug daily. Elevated serum aminotransferase (transaminase) concentrations, especially in patients with preexisting liver disease, have also been reported. Vitamin B12 deficiency, folic acid deficiency, megaloblastic anemia, and sideroblastic anemia have occurred rarely in patients receiving cycloserine in conjunction with other antituberculosis agents.
Precautions and Contraindications
Cycloserine is contraindicated in patients hypersensitive to cycloserine.
Cycloserine is contraindicated in patients with severe renal impairment. The drug also is contraindicated in patients with a history of epilepsy, mental depression, severe anxiety or psychosis, and in frequent users of alcohol.
Plasma cycloserine concentrations should be determined at least weekly in patients receiving more than 500 mg of cycloserine daily, in patients with reduced renal function, and in those with signs or symptoms of toxicity. The manufacturer recommends that dosage should be adjusted to maintain blood concentrations of the drug at less than 30 mcg/mL.
Renal, hepatic, and hematologic tests should be performed during cycloserine therapy. Doses and/or frequency of administration of cycloserine should be decreased in patients with renal impairment, since symptoms of acute toxicity may occur if usual dosage of the drug is used in these patients.
Pediatric Precautions
Although safe use of cycloserine in children has not been established, the drug has been used to treat tuberculosis in some children.
Mutagenicity and Carcinogenicity
Cycloserine was not mutagenic in the Ames microbial mutagen test or the unscheduled DNA repair test. Studies have not been performed to date to evaluate the carcinogenic potential of cycloserine.
Pregnancy, Fertitlity and Lactation
Reproduction studies in 2 generations of rats receiving cycloserine in dosages up to 100 mg/kg daily have not revealed evidence of teratogenicity. There are no adequate and controlled studies to date using cycloserine in pregnant women, and the drug should be used during pregnancy only when clearly needed. Because cycloserine crosses the placenta and data are limited regarding safety of the drug in pregnant women, the American Thoracic Society (ATS), US Centers for Disease Control and Prevention (CDC), and Infectious Diseases Society of America (IDSA) state that the drug should be used for the treatment of tuberculosis during pregnancy only when there are no suitable alternatives.
It is not known whether cycloserine can affect fertility in humans. In one reproduction study in 2 generations of rats, there was no impairment of fertility compared to controls in the first mating; there was a somewhat lower fertility rate in the second mating.
Because of the potential for adverse effects from cycloserine in nursing infants, a decision should be made whether to discontinue nursing or the drug, taking into account the importance of the drug to the woman.
Drug Interactions
There is some evidence that adverse nervous system effects of cycloserine, ethionamide, and isoniazid may be additive; therefore, cycloserine should be used with caution in patients receiving ethionamide or isoniazid.
Cycloserine inhibits the hepatic metabolism of phenytoin. Patients receiving both drugs should be observed for evidence of phenytoin intoxication, and the dosage of the anticonvulsant should be reduced if necessary.
Acute Toxcicity
The acute lethal dose of cycloserine in humans in not known. The median acute oral lethal dose of the drug in mice is 5.29 g/kg. Acute toxicity can occur if more than 1 g of cycloserine is ingested by an adult; chronic toxicity is dose related and can occur if more than 500 mg is administered daily.
Manifestations
Limited information is available on acute overdosage of cycloserine. Symptoms of acute toxicity generally involve the CNS and include headache, vertigo, confusion, drowsiness, hyperirritability, paresthesias, dysarthria, and psychosis. Paresis, seizure, and coma may occur with large cycloserine overdosages; alcohol ingestion may increase the risk of seizures.
Treatment
Management of cycloserine overdosage generally involves symptomatic and supportive care. The patient’s airway should be protected and ventilation and perfusion supported. The patient’s vital signs, blood gases, and serum electrolytes should be meticulously monitored and maintained within acceptable limits. Measures to remove unabsorbed drug from the GI tract should be initiated. Use of charcoal may, in many cases, be more effective than use of emesis or gastric lavage and should be considered instead of or in addition to gastric emptying; efforts should be taken to guard the patient’s airway when using gastric emptying or charcoal. The neurotoxic effects of cycloserine may be treated and/or prevented in adults with 200-300 mg of pyridoxine hydrochloride daily. Hemodialysis may enhance elimination of cycloserine from the body, but should be reserved for use in patients with life-threatening toxicity that is unresponsive to less invasive therapy. The manufacturer recommends that clinicians treating acute overdosage of cycloserine consider contacting a poison control center for the most current information on overdosage of the drug and also consider the possibility of multiple drug overdoses, interaction among drugs, and unusual drug pharmacokinetics in the patient.
Mechanism of Action
Cycloserine may be bacteriostatic or bactericidal in action, depending on the concentration of the drug attained at the site of infection and the susceptibility of the infecting organism. Cycloserine inhibits cell wall synthesis in susceptible organisms by competing with d-alanine for incorporation into the bacterial cell wall. In vitro, the antibacterial activity of cycloserine may be inhibited by d-alanine.
Spectrum
Cycloserine is active in vitro and in vivo against Mycobacterium tuberculosis, M. bovis, and some strains of M. kansasii, M. marinum, M. ulcerans, M. avium, M. smegmatis, and M. intracellulare. The drug is also active against some gram-positive and gram-negative bacteria including Staphylococcus aureus, Enterobacter, and Escherichia coli. In vitro, in alanine-free media, the minimum inhibitory concentration (MIC) of the drug is 5-30 mcg/mL for most susceptible mycobacteria and greater than 50 mcg/mL for most susceptible E. coli.
Resistance
Natural and acquired resistance to cycloserine have been demonstrated in vitro and in vivo in strains of M. tuberculosis. Resistant strains of initially susceptible M. tuberculosis develop rapidly if cycloserine is used alone in the treatment of clinical tuberculosis. When cycloserine is combined with other antituberculosis agents in the treatment of the disease, emergence of resistant strains may be delayed or prevented. There is no evidence of cross-resistance between cycloserine and other antituberculosis agents currently available in the US.
Pharmacokinetics
Absorption
About 70-90% of an oral dose of cycloserine is absorbed from the GI tract. Following a single 250-mg oral dose in healthy adults, peak plasma concentrations of the drug averaging 10 mcg/mL are attained within 3-4 hours. Some drug accumulation may occur in patients with normal renal function during the first 3 days of cycloserine therapy.
Distribution
Cycloserine is widely distributed into body tissues and fluids including the lungs, ascitic fluid, pleural fluid, and synovial fluid in concentrations approximately equal to plasma concentrations of the drug. Cycloserine also is distributed into bile, sputum, and lymph tissue. CSF concentrations of cycloserine are reported to be 50-80% of concurrent plasma concentrations of the drug in patients with uninflamed meninges and 80-100% of concurrent plasma concentrations in patients with inflamed meninges. Cycloserine is not bound to plasma proteins.
Cycloserine readily crosses the placenta and is distributed into amniotic fluid. Cycloserine is distributed into milk.
Elimination
The plasma half-life of cycloserine is approximately 10 hours in patients with normal renal function. Plasma concentrations of cycloserine are higher and the half-life is prolonged in patients with impaired renal function.
In patients with normal renal function, 60-70% of an oral dose of cycloserine is excreted unchanged in urine by glomerular filtration within 72 hours. The maximum excretion rate occurs during the first 2-6 hours; approximately 50% of the dose is eliminated within 12 hours. Small amounts of cycloserine are also excreted in feces. The remainder of the dose is apparently metabolized to unidentified metabolites.
Chemistry and Stability
Chemistry
Cycloserine, an antibiotic derived from Streptomyces orchidaceus or Streptomyces garyphalus, is also produced synthetically. The drug is a structural analog of the amino acid d-alanine. Cycloserine occurs as a hygroscopic, white to pale yellow, crystalline powder which may have a faint odor and is freely soluble in water. Cycloserine solutions containing 100 mg/mL have a pH of 5.5-6..
Stability
Cycloserine deteriorates upon absorbing water and is destroyed at neutral or acidic pH. Cycloserine capsules should be stored in tight containers at a temperature less than 40°C, preferably between 15-30°C.
Preparations
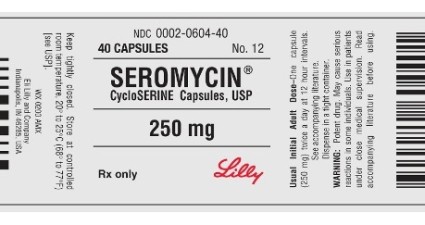
Cycloserine
Oral Capsules 250 mg Seromycin®,Elan
| Dosage forms of Cycloserine: | |
|---|---|
| Seromycin 250 mg pulvule | Seromycin 250 mg capsule |
Synonyms of Cycloserine:
Alpha-Cycloserine, Cicloserina, D-CS, D-Cycloserine, D-Cycloserine Synth. BP 88, D-Cycloserine, Synthetic, D-Oxamicina, D-Oxamycin, DL-Cycloserine, L-Cycloserine
How can i get Cycloserine online over the counter?
You can buy Cycloserine OTC in online drugstore with low cost.
Why do prices vary so much in online pharmacies?
In online pharmacies you can buy both brand-name and generic medications. Generics are cheaper than original brand-name drugs but contain the same active ingredients in the same quantity. You need to take them exactly as the brand-name medications, and they are just as effective as the original drugs.
Therapeutic classes of Cycloserine:
Anti-Infective Agents, Urinary, Antibiotics, Antibiotics, Antitubercular, Antimetabolites
Delivery
Australia, Canada, Mexico, New Zealand, USA, Europe [Belgium, France, Norway, Holland, Ireland, Spain, Switzerland, Great Britain (UK), Italy] and etc.

















































