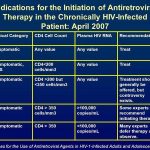
Since most occupational exposures to HIV do not result in transmission of the virus, the potential toxicity of PEP regimens must be considered carefully and, whenever possible, prophylaxis should be implemented in consultation with clinicians who have expertise in antiretroviral therapy and HIV transmission. Modification of the recommended regimens may be appropriate based on factors such as whether the source patient is known or suspected of being infected with drug-resistant strains of HIV; the local availability of antiretroviral agents; and the medical condition, concurrent drug therapy, and drug toxicity in the exposed health-care worker. A decision to offer such prophylaxis should be individualized taking into account the likelihood of HIV transmission occurring, the potential benefits and risks of such prophylaxis, and the interval between the exposure and initiation of therapy.