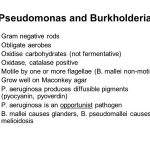
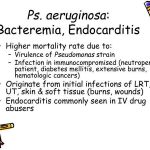
The genus Pseudomonas consists of a number of human pathogens, the most important of which is Pseudomonas aeruginosa. P aeruginosa is an opportunistic pathogen found widely in soil, water, and organic material, reflecting its limited nutritional requirements. A moist environment is favored. Human colonization in the community is rare, and, when it occurs, the skin, gut, and upper or lower airway are colonized.