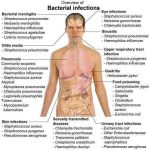
Enterotoxigenic (cholera-like) Diarrhea. Escherichia coli. Pseudomembranous Colitis (Clostridium difficile).
Systemic mycoses, such as histoplasmosis, coccidioidomycosis, cryptococcosis, blastomycosis, paracoccidioidomycosis, and sporotrichosis, are caused by primary or “pathogenic” fungi that can cause disease in both healthy and immunocompromised individuals. In contrast, mycoses caused by opportunistic fungi such as Candida albicans, Aspergillus spp., Trichosporon, Torulopsis (Candida) glabrata, Fusarium, Alternaria, and Mucor are generally found only in the immunocompromised host.
bItraconazole plasma concentrations should be measured during the second week of therapy to ensure that detectable concentrations have been achieved. If the concentration is below 1 mcg/mL, the dose may be insufficient or drug interactions may be impairing absorption or accelerating metabolism, requiring a change in dosage. If plasma concentrations are greater than 10 mcg/mL, the dosage may be reduced.
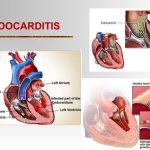
Endocarditis is an inflammation of the endocardium, the membrane lining the chambers of the heart and covering the cusps of the heart valves. Infective endocarditis refers to infection of the heart valves by microorganisms. Endocarditis is often referred to as either acute or subacute depending on the clinical presentation. Acute bacterial endocarditis is a fulminating infection associated with high fevers, systemic toxicity, and death within a few days to weeks if untreated.
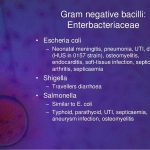
Central nervous system infections include a wide variety of clinical conditions and etiologies: meningitis, meningoencephalitis, encephalitis, brain and meningeal abscesses, and shunt infections. The focus of this chapter is meningitis. N. meningitidis meningitis is the leading cuase of bacterial meningitis in children and young adults in the United States.
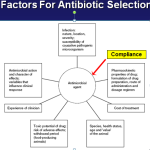
A generally accepted systematic approach to the selection and evaluation of an antimicrobial regimen is shown in Table Systematic Approach for Selection of Antimicrobials. An «empiric» antimicrobial regimen is begun before the offending organism is identified, while a «definitive» regimen is instituted when the causative organism is known. The use of combinations to prevent the emergence of resistance is widely applied but not often realized. The only circumstance where this has been clearly effective is in the treatment of tuberculosis.