This section focuses on the clinical findings, diagnosis, and treatment of pneumococcal meningitis. Please also see site for a general discussion of meningitis.
Clinical Findings
Signs and Symptoms
The clinical presentation of pneumococcal meningitis is similar to other bacterial causes of acute meningitis (Box 4). Severe headache, photophobia, neck stiffness, chills, and fever are common. Because of the rapid onset of severe symptoms, most patients present within a short time from the onset of symptoms. Depending on the initiating source of the infection, there may also be pulmonary complaints (see above) or symptoms referable to sinusitis or otitis (see site).
Patients with meningitis usually appear extremely ill. Many seek quiet areas with low light because of headache and photophobia. Tachycardia and fever, except in those who have difficulty mounting an elevated temperature (eg, the elderly or those with end-stage renal disease), are almost always present. The hallmarks of meningitis are the presence of one or more of the following three findings: nuchal rigidity, Kernig’s sign, or Brudzinski’s sign. If patients present within the initial few hours of symptoms, mental status may be normal. If they present later or if treatment has for some reason been withheld, deterioration in mental status and ultimately obtundation may ensue. Papilledema and focal neurologic signs, including cranial neuropathies, may be present especially later in the course of disease. Hyperesthesia (abnormal acuteness of sensitivity to touch) is common. The remainder of the physical examination may reveal evidence of the primary source of infection (eg, purulent discharge from nose or ear, bulging tympanic membrane, or consolidative findings on chest examination). Unlike meningococcal meningitis, a rash is not found.
Laboratory Findings
As with pneumococcal pneumonia, an elevated leukocyte count is common in pneumococcal meningitis. Other routine laboratory tests are typically normal. Lumbar puncture, which must be performed as rapidly as the diagnosis of meningitis is entertained, shows increased intracranial pressure (> 180 mm H2O), CSF pleocytosis (from 500 to > 10,000 cells/mm3, with polymorphonuclear-cell predominance), an elevated protein concentration (100-500 mg/dL), and depressed glucose (< 40 mg/dL). Gram stain is often positive for characteristic gram-positive organisms. In contrast to the evaluation of pneumonia, in which a positive Gram stain is not always definitive, the presence of gram-positive diplococci on CSF Gram stain is definitive for the diagnosis of pneumococcal meningitis. In untreated patients, the sensitivity of Gram stain has been estimated to be as high as 90%. CSF culture is positive in most cases, and blood cultures may also show growth. In situations in which antibiotics have been administered before lumbar puncture, both Gram stain and culture may be negative. Cell count, protein, and glucose levels, however, are usually abnormal in these situations and not substantially different from the untreated state. Because these abnormalities are not specific for pneumococcal infection, immunologic methods such as counter immunoelectrophoresis or latex agglutination may be helpful for definitive diagnosis. These techniques provide no additional information to routine Gram stain and culture in the evaluation of CSF samples obtained before therapy.
Imaging
Cranial radiography (computed tomography or magnetic resonance scans) is often not indicated in the evaluation of meningitis. In fact, it is contraindicated if it results in undue delays in performing lumbar punctures or initiating empiric therapy. Radiography is indicated when there is clinical evidence of increased intracranial pressure (eg, papilledema) or focal neurologic findings. In these instances, radiography is performed to evaluate whether it is safe to perform a lumbar puncture and to diagnose central nervous system mass lesions, which may require further diagnostic maneuvers. Radiography is rarely useful to confirm positively the presence of meningitis — this is the task of the clinician and the microbiology laboratory. Radiography can be useful in assessing concomitant sinusitis, mastoiditis, or subdural empyema.
Differential Diagnosis
The differential diagnosis of acute meningitis is broad and contains both nonbacterial infectious and noninfectious etiologies (see site). Once lumbar puncture has been performed and the profile of CSF findings suggests bacterial infection, the differential can be narrowed significantly. The differential diagnosis of acute bacterial meningitis is dependent on age group. In neonates, S agalactiae, members of the family Enterobacteriaceae, and Listeria monocytogenes predominate. With the marked decrease in H influenzae type B infections caused by immunization, S pneumoniae and N meningitidis are now the most prevalent organisms seen in older infants and children. In adults, S pneumoniae, N meningitidis, and L monocytogenes (in older adults) are most common.
Complications
The principal immediate and life-threatening complication of meningitis is decreased blood flow to the brain. Rather than a complication, it is best thought of as part of the pathogenic process that occurs if meningitis is unsuccessfully treated. Decreased blood flow may result either from increased intracranial pressure and loss of cerebrovascular autoregulation or from direct vasculitic effects on blood vessels.
Diagnosis
In patients with compatible clinical findings of meningitis, a lumbar puncture is always indicated except when evidence on imaging suggests a risk of herniation. Although lumbar puncture is critical to diagnose meningitis in general and to detect S pneumoniae specifically, delays in performing it should not delay empiric administration of antibiotics. Blood cultures should also be performed, and it is usually possible to collect them before antibiotic treatment. In such cases in which antibiotics must be given before lumbar puncture, blood cultures may serve as the only definitive means of specific pathogen detection.
Treatment
As with pneumonia, patients presenting with acute meningitis receive broad-spectrum empiric regimens that should include coverage for S pneumoniae (see site). Unlike pneumonia, ascertainment of the causal pathogen is more common in acute bacterial meningitis, thus giving the clinician more frequent opportunities to switch to definitive therapy. Either a characteristic CSF Gram stain or culture for S pneumoniae is definitive proof of pneumococcal meningitis.
Antimicrobial susceptibility testing of S pneumoniae is the most important factor in determining definitive therapy (Box 5). Unlike the situation in pneumonia cases, in meningitis cases, isolates that are intermediately resistant to penicillin should not be treated with standard or even higher dosages of penicillin. Instead, susceptibility to ceftriaxone disodium or cefotaxime sodium must be determined. Most isolates that are intermediately resistant to penicillin and some that are highly resistant retain susceptibility to cefotaxime sodium and ceftriaxone disodium. In such cases, these third-generation cephalosporins are the drugs of choice.
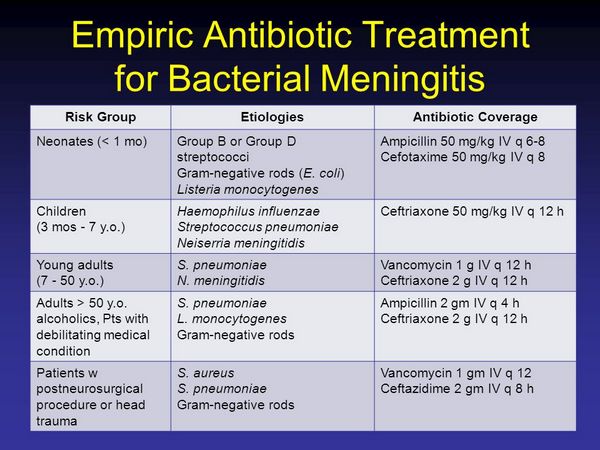
Vancomycin must be used when there is resistance to both cefotaxime sodium and ceftriaxone disodium. Even if there is resistance to both ceftriaxone and cefotaxime, using one of these agents in addition to vancomycin should be considered. If only a positive Gram stain serves as evidence of pneumococcal meningitis and susceptibility results are not available, it is prudent to consider these isolates as resistant and continue the empiric regimen (if the patient is responding) or change to vancomycin if this was not part of the empiric regimen and the patient is not responding. Antibiotic treatment should be given for 10-14 days.
The use of glucocorticoids, although accepted in children, is still controversial in adults. It may be considered for adults in whom the CSF Gram stain is positive, coma is present, or there is evidence of increased intracranial pressure. Glucocorticoids are best considered in the context of empiric therapy because the first dose should be given before antibiotics.


