Essentials of Diagnosis
- Suspected in patients living in or traveling from an endemic area who have acute onset of fever, prostration, and tender adenopathy.
- Yersinia pestis may be recovered from blood cultures or cultures of an aspirate from buboes or sputum in the pneumonic form in 80%-100% of cases.
- Gram stains of bubo aspirate or sputum demonstrate the characteristic bipolar “safety pin” gram-negative microorganisms.
- Y pestis grows aerobically on most culture media after 48-72 h of incubation.
General Considerations
The genus Yersinia, named after Alexander Yersin (1863-1943), includes Y pestis, Y enterocolitica, and Y pseudotuberculosis. Y pestis is the cause of plague, a disease that has left its mark on human history since the medieval time. Y enterocolitica and Y pseudotuberculosis also cause mesenteric lymphadenitis.
Epidemiology
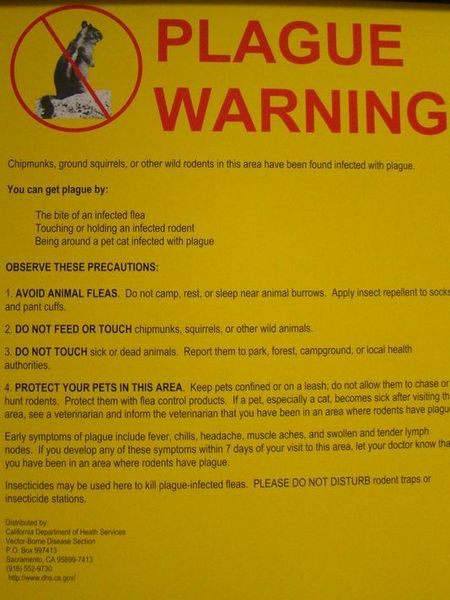
Plague occurs worldwide. The most important reservoir for this enzootic disease is rodents: Rattus rattus and Rattus sylvaticus. The ectoparasite Xenopsylla cheopsis (oriental rat flea) represents the most important and efficient vector of transmission to humans. Humans acquire the disease by a fleabite.
Most cases currently occur in developing countries in Africa and Asia. In the United States, most cases occur in the southwestern states during the months of May to October when individuals are outdoors and in contact with rodents and fleas.
Microbiology
Y Pestis, a member of the Enterobacteriaceae family, is a nonmotile gram-negative bacilli with bipolar Gram staining. This microorganism grows aerobically on most culture media after 48-72 h of incubation. It produces V and W antigens that play a role in the virulence of the organism.
Pathogenesis
After inoculation by an infested flea, Y pestis cells are phagocytized quickly by leukocytes and macrophages, where they replicate rapidly and produce the virulence antigens. The microorganisms are resistant to intracellular killing and they multiply in the regional lymph nodes and disseminate to the blood and other viscera causing profound toxemia. A severe bleeding diathesis may occur as a result of the effect of plague toxin on blood vessel walls or as a consequence of disseminated intravascular coagulation.
Clinical Findings
Signs and Symptoms
After an incubation period of 2-8 days following the bite of an infected flea, patients present with sudden onset of fever, chills, weakness, and headaches (Box 7). The bubonic form of plague is characterized by the appearance of buboes, which are swollen, painful regional lymphadenopathy (typically inguinal or axillary), appearing after a few hours or on the next day. On physical examination, patients are toxic, lethargic, and agitated. The temperature is usually elevated to 41 °C. Buboes are matted, extremely tender and are 2-10 cm in diameter. Rarely, a vesiculopapular lesion from the fleabite is present. Bleeding from the gastrointestinal tract, respiratory tract, or the genitourinary tract is common (so-called red death). Petechiae and large ecchymoses occur along with gangrene of the distal extremities, nose, or penis (so-called Black Death).
The septicemic form of plague is characterized by high-grade bacteremia without palpable lymphadenopathy. Signs and symptoms are otherwise similar to the bubonic form. In this form of the disease, death occurs in 3-5 days in ~ 50% of cases. Y pestis reaches the lungs by way of the hematogenous route or less commonly via the airborne route and causes pneumonia. The pneumonic form is highly contagious and is spread by inhalation of droplet nuclei from a patient with pneumonic plague.
Laboratory Findings
Y pestis may be recovered from blood cultures or cultures of an aspirate from buboes or sputum in the pneumonic form in 80-100% of cases. Gram stains of bubo aspirate or sputum demonstrate the characteristic bipolar “safety pin” gram-negative microorganisms.
Differential Diagnosis
The differential diagnosis includes tularemia, lymphogranuloma venereum, cat-scratch disease, or severe staphylococcal and streptococcal infections.
Complications
See Signs and Symptoms.
Treatment
Streptomycin, the drug of choice for the treatment of plague, reduces the case fatality rate from > 50% in untreated cases to 10% in treated cases (Box 8). For patients who are allergic to or unable to tolerate streptomycin, tetracycline is a satisfactory alternative agent. In meningitis, the use of an antimicrobial agent with good penetration into the cerebrospinal fluid is essential. Chloramphenicol is administered at a loading dose of 25 mg/kg followed by 15 mg/kg intravenously every 6 h for a 10-day course.
Prevention & Control
Primary prevention
Patients with suspected pulmonic plague should be placed in strict respiratory isolation until the sputum culture is negative (Box 9). Chemoprophylaxis with tetracyclines or sulfonamides should be administered to individuals who have had close contact with patients with plague pneumonia and for household contacts of flea-borne plague cases.
Secondary Prevention
For persons at high risk of exposure, two forms of vaccines are available: a live attenuated and a formalin-killed plague vaccine.




