Clinical Findings
Signs and Symptoms
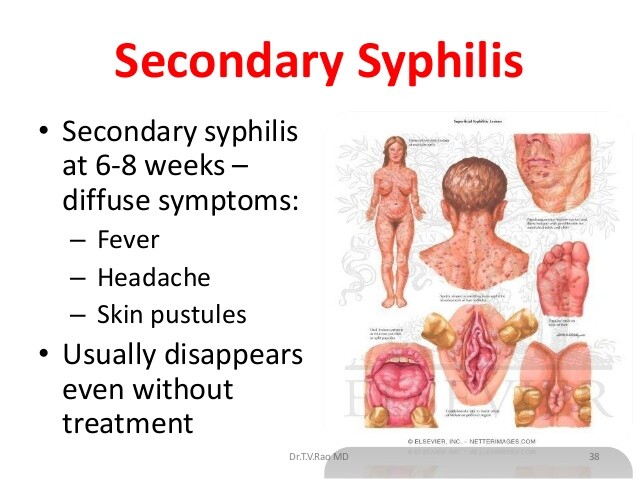
The secondary stage of syphilis occasionally overlaps with the primary phase but usually begins ~ 6 weeks after resolution of the chancre; however, it can develop as late as 6 months after infection (see Box 1). Most patients have some degree of skin or mucocutaneous involvement. A faint and evanescent macular rash of the trunk and abdomen known as roseola syphilitica is sometimes seen initially.
A generalized, symmetric, nonpruritic rash consists of some combination of erythematous or copper-colored macular, papular, papulosquamous, or pustular lesions. These lesions can be found on the palms, soles, genitalia, and oral mucous membranes. The rash of syphilis often provides a diagnostic challenge, deserving of its moniker “the great imitator.”
Condylomata lata refer to eroded papules that can fuse together to create flat, highly infectious lesions in moist, intertriginous areas such as the anogenital region.
They occur in 10-25% of secondary infections. Mucous patches refer to the slightly raised, grayish, painless ulcerations seen on mucous membranes in ~ 15-30% of patients with secondary syphilis. A patchy, “moth-eaten” appearance of hair on the scalp, eyebrows, and beard is well described.
The CNS and gastrointestinal, renal, and musculoskeletal systems may also be affected during the secondary stage of syphilis.
Patients with syphilitic meningitis typically present with headache, nausea and emesis, stiff neck, and cranial neuropathies involving the third, sixth, seventh, and eighth cranial nerves.
CSF analysis reveals a mononuclear pleocytosis, an elevated protein, and, in half of patients, hypoglycorrhachia. Optic neuritis, iritis, and uveitis can be seen during this stage as well. Although only 1-2% of patients with secondary syphilis have documented acute aseptic meningitis, CSF findings may be abnormal in ~ 25-50% of patients.
Syphilitic gastritis causes emesis and epigastric pain. Endoscopic examination usually reveals ulcerations or pronounced gastric folds that contain spirochetes. Of patients with primary or secondary syphilis, ~ 10% will have elevated liver function tests (characteristically alkaline phosphatase) and hepatomegaly, the results of hepatic necrosis and granulomatous inflammation.
Renal disease is caused by immune complex-mediated mechanisms and presents as nephrotic syndrome or glomerulonephritis. Synovitis, osteitis, or periostitis can be seen in = one-fifth of patients.
Laboratory Findings
T pallidum can be detected directly with darkfield and immunofluorescent microscopy in condylomata lata and mucous patches. Nontreponemal and treponemal serologic tests are usually reactive during this stage of disease (see Diagnosis below).
Differential Diagnosis
The differential diagnosis of the dermatologic manifestations of secondary syphilis is quite extensive and should include pityriasis rosea, tinea versicolor, erythema multiforme, drug eruption, viral exanthems, psoriasis, ringworm, and scabies. The pale, pinkish condylomata lata lesions tend not to be as raised as the venereal warts of condyloma accuminata. Mucous patches can be confused with herpes simplex lesions, aphthous ulcerations, candidiasis, and Stevens-Johnson syndrome. Both mucous patches and condylomata lata contain spirochetes, which can be visualized by darkfield examination.