Description of Medical Condition
Inflammation of the bronchioles, usually seen in young children, occasionally in high-risk adults. May be seasonal (winter and spring) and often occurs in epidemics. Usual course: insidious; acute; progressive.
System(s) affected: Pulmonary
Genetics: N/A
Incidence/Prevalence in USA: Medical care provided to 1000-1500/100,000 annually. Estimated incidence is higher. Annual winter-spring epidemics.
Predominant age: newborn-2 years (peak age 2-6 months)
Predominant sex: Male > Female
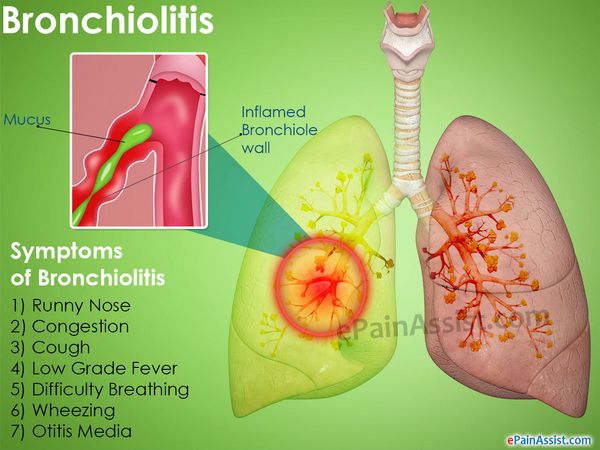
Medical Symptoms and Signs of Disease
- Anorexia
- Cough
- Cyanosis
- Expiratory wheezing
- Apnea
- Fever
- Grunting
- Inspiratory crackles
- Intercostal retractions
- Irritability
- Noisy breathing
- Otitis media
- Pharyngitis
- Tachycardia
- Tachypnea
- Vomiting
What Causes Disease?
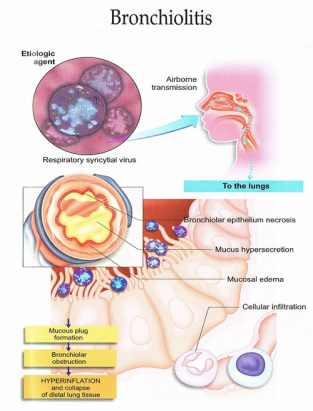
- Respiratory syncytial virus — most prevalent
- Parainfluenza
- Adenovirus
- Rhinovirus
- Influenza virus
- Chlamydia
- Eye, nose, mouth inoculation
- Exposure to adult with URI
- Day care exposure (significant)
- Idiopathic (many adult cases)
Risk Factors
- Contact with infected person
- Children in day care environment
- Heart-lung transplantation patient
- Adults — exposure to toxic fumes, connective tissue disease
Diagnosis of Disease
Differential Diagnosis
- Asthma
- Vascular ring
- Lobar emphysema
- Foreign body
- Heart disease
- Pneumonia
- Reflux
- Aspiration
- Cystic fibrosis
Laboratory
- Arterial blood gas — hypoxemia, hypercarbia, acidemia
- Respiratory viral culture
- Respiratory viral antigens
Drugs that may alter lab results: N/A
Disorders that may alter lab results: N/A
Pathological Findings
- Abundant mucous exudate
- Mucosal — hyperemia, edema
- Submucosal lymphocyte infiltrate, monocytic infiltrate, plasmacytic infiltrate
- Small airway debris, fibrin, inflammatory exudate. fibrosis
- Peribronchiolar mononuclear infiltrate
Special Tests
Infant pulmonary function studies — research tool
Imaging
- Chest x-ray
- Focal atelectasis — RUL common
- Air trapping
- Flattened diaphragm
- Increased anteroposterior diameter
- Peribronchial cuffing
Diagnostic Procedures
N/A
Treatment (Medical Therapy)
Appropriate Health Care
- Most patients can be treated at home
- Inpatient indicated for patient with increased respiratory distress, cyanosis, and dehydration or inability to feed
General Measures
- Most critical phase is first 48-72 hours after onset. Treatment is usually symptomatic.
- Fluid at maintenance
- Mechanical ventilation in respiratory failure
- Isolation: contact; handwashing most important
- Antiviral agents for selected high-risk patients
- Cardio-respiratory monitoring
- Inhaled bronchodilators are commonly used, although efficacy has been hard to demonstrate in controlled studies
- Steroids may not change course — except in patients with reactive airway disease
Activity
- Avoid exposure to crowds, viral illness for 2 months
- Avoid smoke
Diet
- Frequent small feedings of clear liquids
- If hospitalized, may require intravenous fluids
Patient Education
- Griffith: Instructions for Patients; Philadelphia, Elsevier
- American Academy of Pediatrics; website www.aap.org
Medications (Drugs, Medicines)
Drug(s) of Choice
- Oxygen
- Albuterol: may be effective for acute symptoms
- Epinephrine aerosols may be of more benefit
- Ribavirin: For infants and children, an inhaled antiviral agent active against RSV, may be indicated in patients with underlying cardio-pulmonary disease, young age (< 6 weeks), or with severe RSV (elevated pC02; require mechanical ventilation — use with caution via ventilator). Nebulize via small particle aerosol generator (SPAG). Use of ribavirin has decreased in recent years, secondary to lack of significant clinical efficacy.
Contraindications: Refer to manufacturer’s literature
Precautions: None
Significant possible interactions: None
Alternative Drugs
- Antibiotics only if secondary bacterial infection present (rare)
- Corticosteroids do not change course, unless infant has reactive airway disease. In adults corticosteroids may be helpful.
Patient Monitoring
- If patient is receiving home care, follow daily by telephone for 2-4 days
- For hospitalized patient, monitor as needed depending on severity of infection. Bronchiolitis can be associated with apnea.
Prevention / Avoidance
- Hand washing
- Contact isolation of infected babies
- Persons with colds should keep contacts with infants to a minimum
- Palivizumab (Synagis), a monoclonal product, administered monthly, November through March, 15 mg/kg IM. Available in single use vials of 100mg and 50mg. Used for RSV prevention in high risk patients:
- 28-32 weeks gestation and less than 6 months old in November
- Less than 28 weeks gestation and less than 12 months old
- Moderately severe BPD and up to two years old
- Hemodynamically significant congenital heart disease (until age 6 months)
- RSV immune globulin, a human blood product, can also be used in at-risk patients. Monthly infusions of 750 mg/kg, November through March, in a controlled setting. Avoid fluid overload. Vial is 50 mg/mL; infuse at 1.5-6 mL/kg/hr; monitor oximeter and vital signs.
- Both of these medications are quite expensive.
Possible Complications
- Bacterial superinfection
- Bronchiolitis obliterans
- Apnea
- Respiratory failure
- Death
- Increased incidence of RAD
Expected Course / Prognosis
- In most cases, recovery is complete within 7-10 days
- Mortality statistics differ, but probably under 1%
- High-risk infants (BPD, CHD) may have prolonged course
Miscellaneous
Associated Conditions
- Common cold
- Conjunctivitis
- Pharyngitis
- Otitis media
- Diarrhea
Age-Related Factors
Pediatric: Most common in infants
Geriatric: N/A
Pregnancy: N/A
International Classification of Diseases
466.11 Acute bronchiolitis due to respiratory syncytial virus
466.19 Acute bronchiolitis due to other infectious organisms
Abbreviations
BPD = bronchopulmonary dysplasia CHD = congenital heart disease RAD = reactive airway disease SPAG = small particle aerosol generator



