Description of Medical Condition
Paralysis or weakness of the muscles supplied by the facial nerve, typically unilaterally, due to inflammation and swelling of the facial nerve within the facial canal
- Bell palsy: Idiopathic
- Ramsay Hunt syndrome: Bell palsy associated with vesicles within the outer ear canal or behind the ear. due to herpes zoster infection
- Facial diplegia: The simultaneous development of bilateral Bell palsy is highly unusual and conditions such as Guillain-Barre syndrome and chronic meningitis should be considered as possible explanations.
System(s) affected: Nervous
Genetics: There is a familial tendency toward Bell palsy
Incidence/Prevalence in USA: Incidence 16 in 100,000
Predominant age: Affects all ages. Most common
in individuals over 30 years of age.
Predominant sex: Male = Female
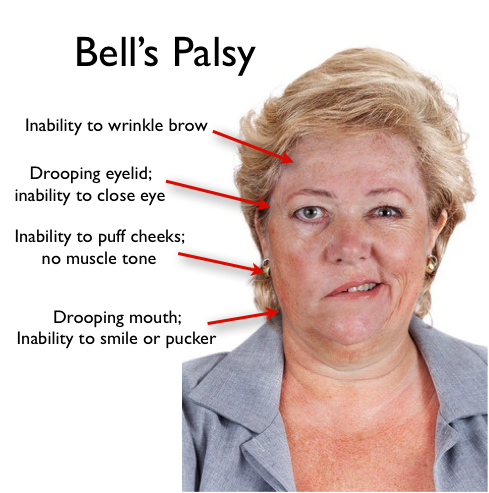
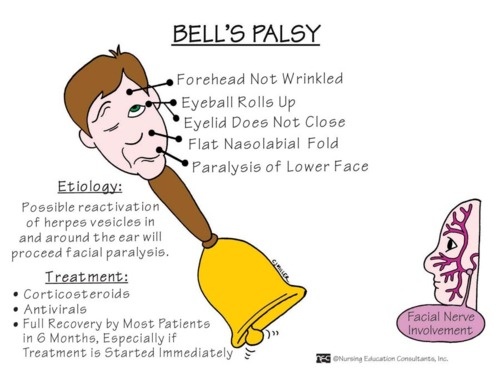
Medical Symptoms and Signs of Disease
- Sudden onset or onset over days
- Unilateral total or partial paralysis of the facial muscles
- Mild “numbness” on the affected side
- Ipsilateral inadequate tear production; ipsilateral tearing
- Ipsilateral loss of taste
- Ipsilateral ear ache
- Ipsilateral exaggerated sound
- Ipsilateral loss of corneal reflex
What Causes Disease?
- Bell palsy
- Inflammation of the facial nerve within the facial canal
- Exposure to cold
- Probably viral
- Ramsay Hunt syndrome
- Herpes zoster
- Rarely Herpes simplex
- Diabetes mellitus
Risk Factors
- Age over 30
- Exposure to cold
- Diabetes
- Pregnancy
- Upper respiratory infection (coryza, influenza)
Diagnosis of Disease
Differential Diagnosis
- Neoplastic
- Carcinomatous meningitis
- Leukemic meningitis
- Tumors of the parotid gland
- Tumors of the base of the skull
- Infectious
- Lyme disease
- Chronic meningitis
- Bacterial meningitis
- Osteomyelitis of the base of the skull
- Otitis media
- Leprosy
- Other
- Sarcoidosis
- Melkersson-Rosenthal syndrome (facial paralysis with scrotal tongue)
- Head injury with fracture of the temporal bone
- Brainstem stroke (anteroinferior cerebellar artery)
- Multiple sclerosis
- Guillain-Barre syndrome (can initially present as a very typical Bell palsy)
- Multifocal acquired demyelinating sensory and motor neuropathy (a variant of CIDP)
Laboratory
- CSF protein — mildly elevated in 1/3 of cases
- CSF cells — mildly elevated in 10% of cases, with a mononuclear cell predominance
Drugs that may alter lab results: N/A
Disorders that may alter lab results: N/A
Pathological Findings
-
Edema of the facial nerve
-
Occasional hemorrhagic streaks
-
Dilatation of the vasa nervorum
-
Infiltration of mononuclear cells in some cases
-
Atrophy of the facial nerve
Special Tests
- Electromyography in the first three weeks after onset of the condition manifests a decreased or absent interference pattern on the affected side, which reflects a reduction or absence of function of the facial motor units. After three weeks, denervation potentials (fibrillations) are typically seen. Eventually, with recovery, low-amplitude, short-duration, polyphasic (nascent) motor units may appear in previously denervated areas. Recovery may be incomplete.
- Nerve conduction velocities may reveal absence or attenuation of the evoked potential, slowing of the conduction velocity or a normal conduction velocity and amplitude (variable due to varying severity and duration of condition)
- Blink reflex — the electrophysiological equivalent of the corneal reflex, should be abnormal in all cases
Imaging
MRI to rule out posterior fossa lesions and intracanalicular 8th nerve tumors if clinical suspicion is high. Bell palsy can be mimicked by small brainstem strokes.
Diagnostic Procedures
Spinal tap may reveal an elevated protein or cell count, however, it is usually not necessary
Treatment (Medical Therapy)
Appropriate Health Care
Outpatient except for surgical decompression (very controversial and largely abandoned)
General Measures
- Close and patch ipsilateral eye
- Methylcellulose ophthalmic drops
Surgical Measures
Total failure of recovery can be treated by anastomosing the dental VII cranial nerve to the proximal end of another cranial nerve
Activity
Fully active. Due to patching, use caution in activities requiring keen depth perception.
Diet
No special diet
Patient Education
Explanation and reassurance when appropriate
Medications (Drugs, Medicines)
Drug(s) of Choice
- Corticosteroids: Prednisone 80 mg po qd for three days, then 60 mg po qd for three days, then 40 mg po qd for three days, then 20 mg po qd for three days, then discontinue use. Course of treatment to begin immediately after onset of Bell palsy. There is little benefit in starting steroids after four days. Use of corticosteroids is controversial.
- Antiviral agents with activity against herpes group of viruses in Ramsay Hunt syndrome and idiopathic Bell palsy
Contraindications: Pre-existing infections including tuberculosis and systemic mycosis
Precautions: Use with discretion in pregnancy, peptic ulcer disease, and diabetes
Significant possible interactions: MMR, OPV, and other live vaccines
Alternative Drugs
N/A
Patient Monitoring
- Recheck monthly for six to twelve months
- Look for evidence of corneal abrasions. Expect early recovery.
Prevention / Avoidance
N/A
Possible Complications
- Unmasking of subclinical infection (such as tuberculosis) by steroid usage
- Steroid-induced psychological disturbances
- Steroid-induced avascular necrosis of hips, knees and/or shoulders
- Corneal abrasion and ulceration
Expected Course / Prognosis
- Complete, partial or no recovery of function. Patients with partial denervation typically fully recover. Patients with total denervation usually partially recover, but may exhibit aberrant regeneration (e.g., crocodile tears) or hemifacial spasm as long term complications.
- May recur on the same or opposite side
Miscellaneous
Associated Conditions
N/A
Age-Related Factors
Pediatric: N/A
Geriatric: N/A
Pregnancy
Use steroids cautiously in pregnancy. Consult with obstetrician.
Synonyms
- Idiopathic facial paralysis
International Classification of Diseases
351.0 Bell palsy
See Also
Herpes simplex Herpes zoster


