Description of Medical Condition
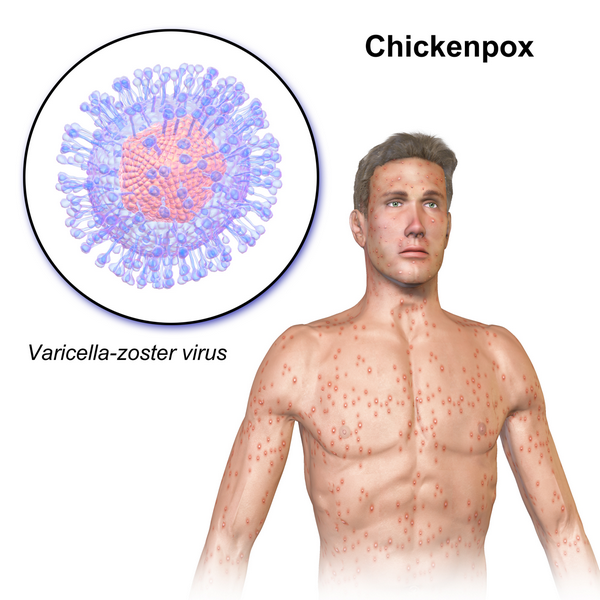
A common, highly contagious, childhood exanthem characterized by the development of typical crops of vesicles on the skin and mucous membranes.
- The virus is spread by respiratory droplets or direct contact with vesicles or indirectly through freshly soiled articles
- Outbreaks tend to occur from January to May
- The usual incubation period is 14-16 days (range 11-21). Patients are infectious from approximately 48 hours before appearance of the rash until the final lesions have crusted. Most people acquire chickenpox during childhood and develop long immunity.
System(s) affected: Skin/Exocrine, Nervous
Genetics: No known genetic pattern
Incidence/Prevalence in USA: Common
Predominant age: Peak incidence 5-9 years, but may occur at any age
Predominant sex: Male = Female
Medical Symptoms and Signs of Disease
-
- Prodromal symptoms — fever, malaise, anorexia, mild headache
- Characteristic rash — crops of “teardrop” vesicles on erythematous bases
- Lesions erupt in successive crops
- Progress from macule to papule to vesicle, then begin to crust
- Rash present in various stages of development
- Pruritic
- Usually begins on trunk, then spreads to face and scalp
- Minimal involvement of the extremities
- Lesions may be present on mucous membranes, oral and vaginal
What Causes Disease?
Human (alpha) herpesvirus 3 (varicella-zoster virus. V-Z virus), a member of the Herpesvirus group; a double-stranded DNA virus. (Reservoir: humans.)
Risk Factors

- No prior history of varicella
- Immunosuppressed (especially children with leukemia/ lymphoma in remission or on high-dose corticosteroids)
Diagnosis of Disease
Differential Diagnosis
- Herpes simplex
- Herpes zoster
- Impetigo
- Coxsackievirus infection
- Papular urticaria
- Scabies
- Dermatitis herpetiformis
- Drug rash
- Rickettsialpox
Laboratory
- Leukocyte count may be normal, low, or mildly increased
- Marked leukocytosis is suggestive of secondary infection
- Multinucleated giant cells on Tzanck smear from scrapings of vesicles
- Isolated virus from human tissue culture
Drugs that may alter lab results: N/A
Disorders that may alter lab results:
- Herpes zoster
- Herpes simplex
Pathological Findings
- Skin lesions histologically identical to herpes simplex virus
- In fatal cases intranuclear inclusions can be found in the endothelium of blood vessels and most organs
Special Tests
For complicated cases and epidemiologic studies:
- Visualization of the virus by EM
- Serologic testing by FAMA or ELISA
- Detection of viral DNA by PCR
Diagnostic Procedures
N/A
Treatment (Medical Therapy)
Appropriate Health Care
Outpatient except for complicating emergencies
General Measures
- Supportive/symptomatic treatment
- Good hygiene to avoid secondary infection
Activity
As tolerated. Children may return to school when lesions have scabbed over, temperature is normal and sense of well-being has returned.
Diet
No special diet
Patient Education
Griffith: Instructions for Patients; Philadelphia, Elsevier
Medications (Drugs, Medicines)
Drug(s) of Choice
- Antipyretics for fever
- Avoid aspirin because of its link to Reye syndrome
- Local and/or systemic antipruritic agents for itching
- In immunocompromised host — varicella-zoster immune globulin (VZIG) available for passive immunization. VZIG must be given within 96 hours after exposure to be beneficial. After 4th day postexposure, wait for rash to develop then give acyclovir 500 mg/m2/day intravenously every 8 hours for 7 days.
- Acyclovir — decreases duration of fever and shortens time of viral shedding. Recommended for adolescents, adults and high-risk patients. Most beneficial if initiated early in the disease (< 24 hours).
- 2-16 yr: 20 mg/kg/dose (max. 800 mg/dose), qid for 5 days
- Adults: 800 mg, 5 times daily.
Contraindications: Hypersensitivity to the drug
Precautions: Possible renal insufficiency with acyclovir
Significant possible interactions: Concurrent administration of probenecid increases half-life. Increased effect with zidovudine (drowsiness, lethargy)
Alternative Drugs
- Famciclovir 500 mg tid x 7-10 days
- Valacyclovir 1 gm tid x 7-10 days
- Vidarabine
- Interieron
Patient Monitoring
Usually none in mild cases. If complications occur, intensive supportive care may be required.
Prevention / Avoidance
- Exposed, susceptible individuals considered infectious for 21 days
- Isolation of hospitalized patients
- Passive immunization with ZIG, VZIG, orthe intravenous formulation of ZIP. Both ZIG and VZIG should be given within 96 hours (preferably within 72 hours) of exposure to ensure efficacy. ZIP can be given somewhat later. Recommended for persons exposed to chickenpox or shingles within 96 hours who are immunocompromised, >15 years old without prior history of chickenpox, newborns of mothers with onset of chickenpox < 5 days before delivery or < 2 days after delivery. Exposure criteria: continued household contact, prolonged face-to-face contact (same room), or indoor playmate > 1 hour.
- Varicella vaccine effectiveness decreases significantly after 1 year (most cases of breakthrough disease are mild). If administered at younger than 15 months, the vaccine’s effectiveness was lower in the first year after vaccination, but the difference in effectiveness was not statistically significant for subsequent years.
- Varicella-Virus vaccine (Varivax) — a live attenuated vaccine approved by the FDA and recommended by ACIP for immunization of healthy individuals, 12 months and above, who have not had chickenpox
- 012m-12y: single dose 0.5 mL SC. Cumulative efficacy 70-90%.
- 013y and above: two 0.5 mL SC doses 4-8 weeks apart. Efficacy 70%.
- Has been shown to prevent or significantly reduce the severity of varicella if given within 72 hours and possibly up to 5 days, postexposure in several studies
- May be considered for a subset of HIV positive children in CDC Class I with CD4 > 25%
- Vaccine recipients should avoid contact with immunocompromised people, and pregnant women who have never had chickenpox and their newborns, for up to 6 weeks after vaccination
Possible Complications
- Secondary bacterial infection — cellulitis, abscess, erysipelas, sepsis, septic arthritis/osteomyelitis, staphylococcal pyomyositis
- Pneumonia (20-30% of adults with chickenpox have lung involvement)
- Encephalitis (the most common CNS complication)
- Reye syndrome
- Purpura
- Lymphadenitis
- Nephritis
Expected Course / Prognosis
- In the healthy child, chickenpox is rarely a serious disease and recovery is complete
- Confers long immunity
- Second attack rare, but subclinical infection common
- Infection latent and may recur years later as herpes zoster in adults (and sometimes in children)
- Fatalities rarely occur from complications
Miscellaneous
Associated Conditions
N/A
Age-Related Factors
Pediatric:
- Neonates born to mothers who develop chickenpox 5 days before or 2 days after delivery are at risk for serious disease. Must give VZIG.
- Varicella bullosa seen mainly in children under two. Lesions appear as bullae instead of vesicles. Clinical course unchanged.
- Case-fatality (in USA) 2/100,000
- Most common cause of death: septic complications and encephalitis
Geriatric:
- Infection more severe than in children
- Latent varicella infection may reactivate and cause the exanthem shingles or zoster
- Case-fatality 30/100,000
- Most common cause of death: primary viral pneumonia
Pregnancy
Risk of transplacental infection following maternal infection is 25%. Congenital malformations are seen in 5% when the fetus is infected during the 1st or 2nd trimester. There is an increased morbidity for women infected during pregnancy (e.g., pneumonia).
Synonyms
• Varicella
International Classification of Diseases
052.9 Varicella without mention of complication
See Also
Immunizations Herpes zoster
Abbreviations
ACIP = Advisory Committee on Immunization Practices
FAMA = fluorescent antibody to membrane antigen
ZIG = zoster immune globulin
ZIP = zoster immune plasma
DNA = deoxyribonucleic acid
EM = electron microscopy
PCR = polymerase chain reaction
VZIG = varicella-zoster immune globulin


