Drugs mentioned:
- amoxicillin-clavulanate (Augmentin / SmithKline Beecham)
- cefaclor (Ceclor / Lilly)
- cefuroxime (Zinacef / Glaxo)
- ribavirin (Virazole / ICN)
Toxic Shock in Children
Toxic shock is an acute disease characterized by fever, mucous membrane hyperemia, subcutaneous edema, desquamating erythroderma, hypotension, and multisystem organ involvement. A decade ago it was widely described as an illness affecting young women, associated with vaginal colonization by Staphylococcus aureus and the use of tampons. Subsequent studies demonstrated that S. aureus produces several related enterotoxins — including toxic shock syndrome toxin-1 (TSST-1) — that are thought to cause the disorder by activating host inflammatory responses and by triggering the release of cytokines.
Not all cases of toxic shock are associated with menstruation, however, and not all cases are associated with S. aureus. Several infectious agents — including streptococcus, pseudomonas, mycoplasma, and adenovirus — cause a toxic-shock like syndrome. The toxins involved appear to have a common mechanism of action. TSST-1 and other staph enterotoxins, strep pyrogenic (fever-producing) exotoxins, and some mycoplasma toxins act as superantigens, binding specific regions of the T cell receptor in association with proteins in the major histocompatibility complex, with resulting T cell proliferation and cytokine release.
Torres- Martinez and colleagues in the pediatric departments at two London hospitals — St. Mary’s Hospital Medical School and Guy’s Hospital — described four children with toxic shock syndrome associated with group A beta-hemolytic streptococcus (GABHS). All four children suffered from a fulminant disorder characterized by shock, multisystem involvement, and a distinctive erythematous rash with desquamation that was diagnostic for toxic shock syndrome. The only organism isolated was GABHS.
Recent reports of a resurgence in severe acute streptococcal infections have alerted epidemiologists to the possibility that a more virulent strain of streptococcus is circulating worldwide. Not only has there been an increase in the incidence of serious disease due to GABHS in the past decade, but there has been an increase in the incidence of complications such as rheumatic fever. Before 1940, streptococcal infections accounted for a major proportion of the infectious diseases seen in developed countries, with fatalities commonly reported due to streptococcal bacteremia, severe scarlet fever, and erysipelas. According to Torres-Martinez et al, in 1937 the fatality rate for streptococcal bacteremia was 72% in the total population and 62% in children under 15 years of age.
“Based on the clinical description of the disease in those patients, it is possible that the disorder now termed streptococcal toxic shock syndrome accounted for some of the severe cases and deaths,” said the investigators. “The question therefore arises as to whether the growing number of reports of streptococcal toxic shock syndrome represents the emergence of a ‘new’ streptococcus associated syndrome, or whether it reflects the rediscovery of an entity which may have been more common in the preantibiotic era.”
One of the patients described by Torres-Martinez et al. was a 10-year old girl with an infected cut below the knee. She was hospitalized after fever and a macular erythematous rash developed. Tachycardia, jaundice, and blistering on the right upper leg were noted, and the child was transferred to Guy’s hospital. On admission she was drowsy and hypotensive, with fever, red lips and tongue, conjunctivitis, intensely swollen ankles and wrists, and desquamation. She was given large volumes of colloid and required inotropic support with dobutamine and dopamine along with prostacyclin to improve perfusion. She had renal and hepatic impairment and respiratory distress that required ventilation; full sedation; and paralysis.
She gradually improved, but her right arm had to be amputated below the elbow and extensive skin grafting was required on her feet. Antibiotic therapy consisted of high-dose penicillin and flucloxacillin, followed by cefotaxime and clindamycin. Three infants described in the report also required aggressive fluid resuscitation and vigorous antibiotic therapy (including penicillin, ampicillin, flucloxacillin, fusidic acid, gentamicin, and rifampin) and, in two cases, mechanical ventilation.
Group A beta-hemolytic streptococcus (GABHS) produces at least four serologically distinct exotoxins, said the investigators, all of which cause fever, produce non-specific stimulation of T-cell proliferation, enhance delayed hypersensitivity, and suppress immunoglobulin synthesis. These exotoxins may also enhance host susceptibility to lethal endotoxic shock and induce tumor necrosis factor. There appears to be a similarity between two of these strep toxins and staph toxins; not only are the toxins similar, they have a similar effect on the immune system.
However, there are clinical differences between the staphylococcal and streptococcal toxic shock syndromes. In the staph syndrome, bacteremia seldom occurs and the site of the infection may be unremarkable. In the strep syndrome, bacteremia occurs and there is severe focal infection; extensive soft tissue involvement more often leads to surgical intervention. On the other hand, desquamation is not always present, or the rash may appear late and coexist with desquamation. In one study of 26 adults with strep toxic shock, only eight had desquamation.
“From the therapeutic point of view,” said Torres-Martinez, “prompt recognition and understanding of the natural history of the disease should lead to an aggressive intensive care approach. Correction of hypovolemia by infusion of large amounts of colloid, inotropic support, and if necessary ventilatory assistance must be implemented to correct shock and restore adequate oxygen delivery to the tissues. In addition, prompt antimicrobial therapy should be started.”
Penicillin remains the drug of choice for GABHS infections, although antibiotics active against staphylococcus should be given until the microbial cause has been identified. “Despite the fulminant nature of the illness and the prolonged and complicated course, complete recovery is possible with early and aggressive treatment.”
Bojang and Walters at the Hospital for Sick Children in London described a five-year old girl who had fever, abdominal pain, vomiting, watery diarrhea, and an erythematous maculopapular rash following a trip to Australia and the Philippines. When hospitalized, the child was pyrexic with cervical lymphadenopathy and dehyradration. Over the next 24 hours, serum sodium dropped from 129-115 mmol/L despite good renal function, white cell count increased, platelet count decreased, and tissue perfusion deteriorated.
Abdominal distension, pain, and diarrhea continued, the erythematous rash covered the trunk and palms, and the child developed conjunctivitis, fissured lips, pulmonary edema, enlarged heart, tachycardia, hypotension, and edema. She required ventilatory support and suffered from severe hypotension and cardiac insufficiency requiring three days of high-dose dobutamine and dopamine to maintain blood pressure. She was unconscious for three days; an electroencephalogram showed non-specific encephalopathy.
Nine days after admission the child was extubated and all inotropic support discontinued; two days later desquamation developed over the tips of all her fingers. She was discharged after 17 days in the hospital, with a diagnosis of staphylococcal toxic shock syndrome. However, after discharge a non-typable strain of adenovirus was isolated from cultures of cerebrospinal fluid and urine specimens collected at initial presentation. Follow-up serology showed a rising CSF titer of antibody to adenovirus, from undetectable at admission to 1:32 six weeks later. There was no evidence of immunodeficiency.
The respiratory and gastrointestinal tract and conjunctiva are the sites most commonly affected by adenovirus, although other organs and systems may be involved (central nervous system, gastrointestinal tract, skeletal muscle, heart, respiratory tract, skin, liver, kidneys, and hematologic system).
According to Bojang and Walters, it is uncommon for a single adenovirus strain to produce multisystem disease in an apparently immunocompetent individual. Some manifestations could be due to shock, but skin changes, CNS involvement, skeletal muscle involvement, and myocarditis cannot be attributed to hypo-tension alone. While this patient satisfied the clinical diagnostic criteria for toxic shock syndrome — fever greater than 38.9ЎC, an erythematous rash, desquamation, and hypotension — she initially had negative microbiological results, with sub-sequent growth of adenovirus from cerebrospinal fluid and urine and seroconversion.
Adenovirus may induce immune events similar to those seen in streptococcal and staphylococcal toxic shock syndromes, i.e., T cell proliferation and cytokine release. “We conclude that this case with multiorgan involvement producing a clinical picture of toxic shock syndrome was due to in-fection with adenovirus,” said the investigators. “We therefore recommend that clinicians consider adenovirus infection in the differential diagnosis of toxic shock syndrome in children.”
Treating Sinusitis in Children
According to data from the National Center for Health Statistics, more than 31 million Americans suffer from sinus problems, making sinusitis one of the leading chronic medical conditions, along with arthritis and high blood pressure. It is not generally recognized that sinusitis is also very common in children. In a review that appeared in the New England Journal of Medicine, Dr. Ellen Wald wrote that an estimated 5- 10% of upper respiratory infections (URI) in children are complicated by acute sinusitis, and since children average 6-8 colds per year, sinusitis is a very common problem in clinical practice.
Uncomplicated viral upper respiratory infections (URI) produce mild-to- moderate symptoms that last five to seven days. During the course of infection, watery nasal discharge becomes thicker, colored, and opaque in a few days, then clears to a mucoid or watery consistency before resolving.
Fever may be present initially, then disappears when the respiratory symptoms begin. Acute sinusitis should be suspected if symptoms persist beyond 10 days (but less than 30 days) or if symptoms are unusually severe (high fever, purulent nasal discharge). “The 10- day mark separates simple viral upper respiratory infection from sinusitis,” said Wald, “and the 30-day mark separates acute from subacute or chronic sinusitis.” In sinusitis, the nasal discharge may be thin or thick, clear or mucous or purulent; the cough may be dry or wet, but must be present during the day although it may be worse at night. The child may have bad breath, painless morning eye swelling, and low-grade fever, but facial pain and headache are rare.
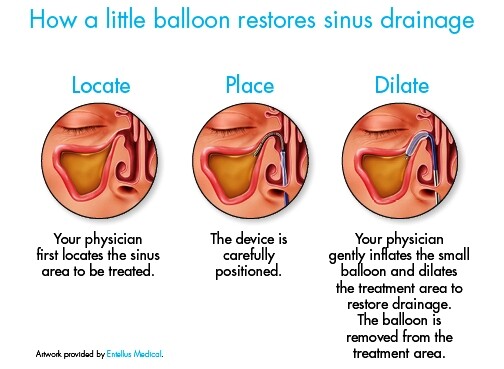
Transillumination (using a carefully positioned external light source to check for the presence of light transmitted though the hard palate or cheeks) and radiographic imaging are two diagnostic techniques which can help determine if the sinus cavity is filled with fluid or tissue.
Transillumination is difficult in the young child, said Wald, “but may be useful in diagnosing disease of the maxillary or frontal sinuses in patients over 10 years of age as long as interpretation is confined to the extremes of either normal transmission or no transmission.” Maxillary-sinus aspiration can also be helpful diagnostically, particularly when the child fails to respond to multiple courses of antibiotics or has severe facial pain or complications, but sedation or general anesthesia may be required in young children.
The main complications of acute sinusitis are subperiosteal abscess of the orbit (with eye swelling, exophthalmos, and impaired extraocular eye movements) and intracranial abscess (with focal neurologic deficits, increased intracranial pressure, and meningeal irritation). A CT scan is necessary for diagnosis, and antibiotic therapy and surgical drainage are usually required for successful treatment.
The mainstay of therapy for sinusitis is antibiotic treatment. The most common pathogens identified in acute and subacute sinusitis are Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. Other species of streptococcus have been identified, but S. pneumoniae accounts for 30-40% of all isolates. Although much rarer, Staphylococcus aureus and anaerobic organisms are recovered from children with severe sinus symptoms requiring surgical intervention, or with sinusitis lasting more than a year. Respiratory viral isolates include adenovirus, parainfluenza virus, influenza virus, and rhinovirus. The most common predisposing factor for recurrent sinusitis is repeated viral URI. Other predisposing conditions include allergic inflammation, cystic fibrosis, immunodeficiency, ciliary dyskinesia, or an anatomical problem.
Amoxicillin is the preferred antibiotic for most uncomplicated sinusitis said Wald, although both H. influenzae and M. catarrhalis may be resistant (35% of H. influenzae and 75% of M. catarrhalis were found to be beta-lactamase producers in one Pittsburgh study). Other regimens include amoxicillin-clavulanate (Augmentin / SmithKline Beecham), erythromycin-sulfisoxazole, trimethoprim-sulfamethoxazole, cefaclor (Ceclor / Lilly), and cefuroxime (Zinacef / Glaxo).
For patients who show rapid symptomatic improvement, 10 days of therapy is adequate. Slow responders should be treated until free of symptoms, and then for an additional seven days. The addition of a decongestant may decrease nasal airway resistance. Patients with allergies can also be treated with antihistamines, desensitization and nasal steroid therapy. Antimicrobial prophylaxis, which has proved to be of value for reducing recurrent episodes of acute otitis media, may help children with recurrent acute sinusitis.
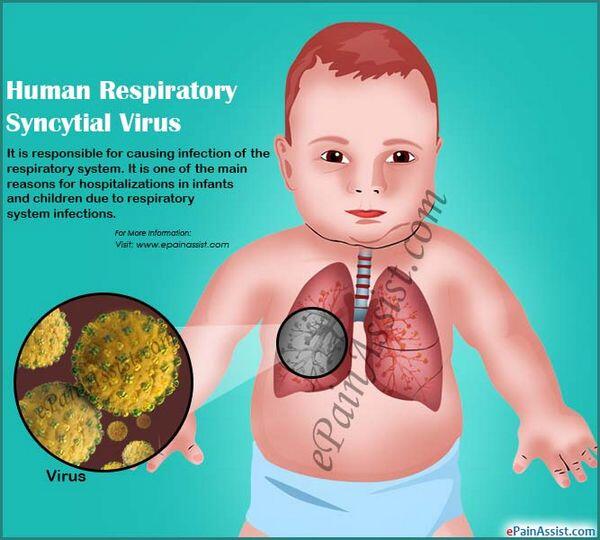
Managing Respiratory Syncytial Virus Infection
Respiratory syncytial virus (RSV) is a highly contagious ribonucleic acid virus of the paramyxovirus family. It is ubiquitous in all age groups. By age two, 95% of children have serologic evidence of past infection, and by adulthood virtually 100% of the population has been infected.
Reinfection is common, despite the presence of antibody, and is usually manifested by a common cold. However, in 40% of infants and young children the infection progresses from the upper to the lower respiratory tract. Bronchiolitis is the primary complication — RSV is responsible for 40-50% of hospitalizations for bronch-iolitis — but pneumonia and bronchopneumonia also occur. For hospitalized patients, mean stay is three days, but up to 11% of patients require intensive care and up to 8% require intubation and ventilation. More than 50% of hospitalizations are of in-fants one to three months of age (boys more often than girls); less than 5% are for neonates less than one month of age. These very young babies often have atypical respiratory syncytial virus infection with nonspecific symptoms (irritability, low-grade fever, apnea).
Two subtypes of the virus — designated A and B — appear to circulate together, although subtype A often predominates during a given season and is associated with more severe disease. The RSV season lasts about four months, peaking in February or March in temperate climates. Incubation period is five to eight days. Infection begins with runny nose, congestion, and low-grade fever, then progresses over the next two to five days from the upper to the lower respiratory tract with cough, dyspnea, and wheezing. Dehydration may occur due to poor oral intake. Diagnosis depends on seasonal occurrence and symptoms.
Several tests are available commercially to detect respiratory syncytial virus antigen in epithelial cells from nasopharyngeal secretions, bronchoalveolar lavage, or lung tissue. The virus is shed abundantly in respiratory secretions and is spread hand-to-eye or hand-to-nose rather than by aerosolization. Quick diagnosis in hospitalized patients can help prevent the nosocomial spread of respiratory syncytial virus, which most likely occurs via the unwashed and ungloved hands of health care workers and family members. Madge et al reported that rapid laboratory diagnosis, cohort nursing, and the wearing of gowns and gloves by all contacts with RSV-infected children significantly reduced the risk of nosocomial RSV infection.
Severe lower respiratory tract infection is more often seen in patients with impaired cardiopulmonary function (congenital heart disease, bronchopulmonary dysplasia, and cystic fibrosis) or immunodeficiency. Respiratory syncytial virus causes diffuse inflammation of the terminal bronchioles, with alveolitis and wheezing. Individuals infected during infancy have a higher incidence of wheezing years later. RSV also increases the concentration of several mediators of bronchospasm and bronchial hyperreactivity (IgE, histamine, and leukotrienes) that contribute to wheezing both during and after infection. These mediators do not develop in all children, so the host plays a role. Cytokines (including interleukins) are involved in coordinating the pathogen-specific immune response, and may play a role in reinfection.
Treatment of RSV infection is largely supportive. Oxygen and intravenous hydration are the mainstays of therapy for lower respiratory tract infection. Various drugs — beta-agonists, epinephrine, and possibly dexamethasone — have been shown to improve clinical scores.
Theophylline does not appear to be useful. Ribavirin (Virazole/ICN), the only antiviral agent licensed for the treatment of respiratory syncytial virus, improves clinical scores and decreases the amount and duration of viral shedding, although it has shown more promise in patients with cardiopulmonary and immunodeficiency diseases than in normal children. In one study of patients requiring mechanical ventilation, ribaviron reduced the need for assisted ventilation. Studies are underway evaluating the safety and efficacy of RSV immunoglobulin in high-risk infants.
Since respiratory syncytial virus infection causes some 91,000 hospitalizations annually at a cost of approximately $300 million, developing a vaccine should be a priority. In the meantime, it is important to reduce the nosocomial spread of RSV through rapid diagnosis and careful nursing.
Measles Upsurge
Measles is a very serious disease, particularly when it causes encephalitis. It strikes about 44 million children a year worldwide and kills 1.5 million of them. Fortunately all American children have access to an effective vaccine, with one dose given at 15 months of age and a second at entry to kindergarten or first grade (as recommended by the Immunization Practice Advisory Committee) or at entry to middle or junior high school (as recommended by the American Academy of Pediatrics).
With an effective vaccine available, why were 9,662 cases of measles were reported in 1991? The answer: only 14 of the infected individuals (0.1%) had received both doses of the vaccine, while a whopping 80% had received no vaccination at all. More than 25% of patients who contracted measles in 1991 had to be hospitalized for complications. Between 1986 and 1990, 2,700 cases of measles occurred college students at 160 campuses across the country. Currently, the Measles-Mumps- Rubella Action Group is promoting legislation that will require all college students to be fully immunized against measles.
If a measles vaccine were to be developed that could be given in only one dose, compliance would be improved. The World Health Organization has been studying such a vaccine — the Edmonston-Zagreb vaccine — but recently halted its use because vaccinated children, while well protected against measles, were dying faster from other infectious diseases such as pneumonia, diarrhea, and parasitic diseases. Interestingly, girls were at greater risk of dying than boys.
Since infection with the measles virus itself is known to cause a generalized immune suppression, it is thought that the vaccine may be doing the same thing. In the United States, only a few pilot programs used the Edmonston-Zagreb vaccine. The problem in this country is the failure of parents to take advantage of the effective vaccine currently available for their children. “Still reeling from the reemergence of tuberculosis,” wrote R. Weiss in Science, “experts are concerned that the country could be caught off guard by another highly infectious slumbering giant.”
How do antiarrhythmics induce arrhythmias?
Podrid and Fogel have proposed that coronary artery disease leads to a marked variation in perfusion pressures and blood flow within the myocardium. Such variations increase extracellular potassium concentrations, decrease tissue pH, and alter the electrical properties of the membrane. Variations in blood flow also result in differences in tissue concentrations of the antiarrhythmic drug, along with differences in drug distribution, binding, and clearance. Differences in potassium levels, pH, and electrophysiologic properties can alter drug action, and in turn can be altered by the drug.
According to Podrid and Fogel, “An antiarrhythmic drug that produces uniform effects under resting and nonischemic conditions may have variable effects during ischemia.” Moreover, an agent that is effective in the immediate postinfarction period could later on provoke an arrhythmia.
“This has important implications regarding the use of antiarrhythmic drugs in patients with underlying coronary artery disease likely to have transient, active ischemia that may be overt or silent,” said Podrid and Fogel. “In these patients antiarrhyth-mic therapy should be evaluated at rest, as well as during physical exertion. Exercise testing is a physiologic way of produc-ing ischemia and activation of the sympathetic nervous system, resulting in the metabolic, electrolyte, and electrophysical alterations that may interact with, potentiate, or interfere with antiarrhythmic drugs action.”

