General principles
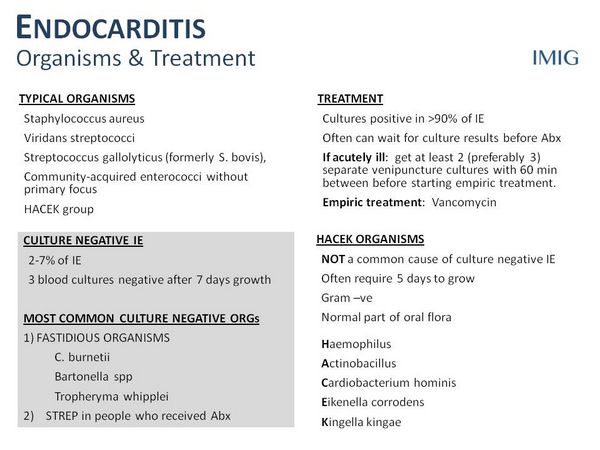
- The most important approach to treatment of Infective endocarditis includes isolation of the infecting pathogen and determination of antimicrobial susceptibilities, followed by high-dose, bactericidal antibiotics for an extended period.
- For most patients 4 to 6 weeks of therapy are required.
- Specific recommendations for treating Infective endocarditis caused by the most common organisms are discussed in this chapter.
- β- Lactam antimicrobials, such as penicillin G, nafcillin, and ampicillin, remain the drugs of choice for streptococcal, staphylococcal, and enterococcal endocarditis, respectively.
- For some pathogens, such as enterococci, the use of synergistic antimicrobial combinations (including an aminoglycoside) is essential to obtain a bactericidal effect.
Nonpharmacologic therapy
- Surgery is an important adjunct to management of endocarditis in certain patients. In most cases, valvectomy and valve replacement are performed to remove infected tissues and restore hemodynamic function. The most important indications for surgical intervention in the past have been heart failure in left-sided Infective endocarditis and persistent infections in right-sided Infective endocarditis.
Streptococcal endocarditis
- Viridans streptococci (Streptococcus mutans, S. sanguis, and S. mitis) are common cause of Infective endocarditis, especially in cases involving native valves. S. bovis is not a viridans streptococcus but is included here because it is penicillin sensitive and treatment regimens are the same as for viridans streptococci.
- Most viridans streptococci are exquisitely sensitive to penicillin G with minimal inhibitory concentrations less than or equal to 0.1 mcg/mL. The minimum inhibitory concentration should be determined for all viridans streptococci and the results used to guide therapy. Approximately 10% to 20% are moderately susceptible (minimum inhibitory concentration 0.1 to 0.5 mcg/mL).
- Recommended therapy in the uncomplicated case caused by fully susceptible strains is 4 weeks of either high-dose penicillin G or ceftriaxone, or 2 weeks of combined therapy with high-dose penicillin G plus an aminoglycoside (Table Suggested Regimens for Therapy of Native-Valve Endocarditis Due to Penicillin-Susceptible Viridans Streptococci and Streptococcus bovis).
- The following conditions should all be present to consider a 2-week treatment regimen:
- The isolate is penicillin sensitive (minimum inhibitory concentration less than or equal to 0.1 mcg/mL)
- There are no cardiovascular risk factors such as heart failure, aortic insufficiency, or conduction abnormalities
- No evidence of thrombotic disease
- Native valve infection
| TABLE. Suggested Regimens for Therapy of Native-Valve Endocarditis Due to Penicillin-Susceptible Viridans Streptococci and Streptococcus bovis (Minimum Inhibitory Concentration ≤0.1 mcg/mL)a | ||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||
-
- No vegetation greater than 5 mm diameter
- Clinical response is evident within 7 days.
- Vancomycin is effective and is the drug of choice for the patient with a history of immediate-type hypersensitivity reaction to penicillin.
- For patients with complicated infection or when the organism is relatively resistant (minimum inhibitory concentration = 0.1 to 0.5 Вµg/mL), combination therapy with penicillin and an aminoglycoside is recommended for 2 weeks followed by penicillin alone for an additional 2 weeks.
Staphylococcal endocarditis
- Staphylococcus aureus is the most common organism causing Infective endocarditis both among intravenous drug abusers and in persons with venous catheters. Coagulase-negative staphylococci (usually S. epidermidis) are prominent causes of prosthetic valve endocarditis.
- Management requires consideration of several factors:
- Is the organism methicillin resistant?
- Should combination therapy be used?
- Is the infection on a native valve or a prosthetic valve?
- Is the patient an intravenous drug abuser?
- Is the infection on the left or right side of the heart?
- The recommended therapy for patients with left-sided Infective endocarditis caused by methicillin-sensitive S. aureus is 4 to 6 weeks of nafcillin or oxacillin, often combined with a short course of gentamicin.
- If a patient has a mild, delayed allergy to penicillin, first-generation cephalosporins are effective alternatives but should be avoided in patients with an immediate-type hypersensitivity reaction.
- In a patient with appositive penicillin skin test or a history of immediate hypersensitivity to penicillin, vancomycin is the agent of choice. Vancomycin, however, kills S. aureus slowly and is generally regarded as inferior to penicillinase-resistant penicillins for methicillin-sensitive S. aureus.
- Rifampin may be added to vancomycin in refractory or complicated infections in patients with left-sided Infective endocarditis and, in some cases, addition of rifampin appeared to result in dramatic patient improvement.
- Vancomycin is the drug of choice for methicillin-resistant staphylococci since most methicillin-resistant S. aureus and most Coagulase-negative staphylococci are susceptible.
Treatment of Staphylococcus Endocarditis in Intravenous
Drug Abusers
- Infective endocarditis in intravenous drug abusers is most frequently (60% to 70%) caused by S. aureus, although other organisms may be more common in certain geographic locations.
- Standard treatment for methicillin-sensitive S. aureus consists of 4 weeks of therapy with a penicillinase-resistant penicillin.
- A 2-week course of nafcillin or oxacillin plus an aminoglycoside may be effective.
- Short-course vancomycin, in place of nafcillin or oxacillin appears to be ineffective.
Prosthetic valve endocarditis
- prosthetic valve endocarditis that occurs within 2 months of cardiac surgery is usually caused by staphylococci implanted at the time of surgery. Methicillin-resistant organisms are common. Vancomycin is the cornerstone of therapy.
| TABLE. Therapy for Native-Valve Endocarditis Due to Strains of Viridans Streptococci and Streptococcus bovis Relatively Resistant to Penicillin G (Minimum Inhibitory Concentration >0.1 mcg/mL and <0.5 mcg/mL)a | ||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| TABLE. Therapy for Endocarditis Due to Staphylococcus in the Absence of Prosthetic Materiala | ||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
- Because of the high morbidity and mortality associated with prosthetic valve endocarditis and refractoriness to therapy, combinations of antimicrobials are usually recommended.
- For methicillin-resistant staphylococci (both MRSA and Coagulase-negative staphylococci), vancomycin is used with rifampin for 6 weeks or more. An aminoglycoside is added for the first 2 weeks if the organism is susceptible.
- For methicillin-susceptible staphylococci, a penicillinase-stable penicillin is used in place of vancomycin.
Enterococcal Endocarditis
- Enterococci cause 5% to 18% of endocarditis cases and are noteworthy for the following reasons: (1) no single antibiotic is bactericidal; (2) inhibitory concentrations to penicillin are relatively high (1 to 25 mcg/mL); (3) they are intrinsically resistant to all cephalosporins and relatively resistant to aminoglycosides (i.e., «low-level» aminoglycoside resistance); (4) combinations of a cell wall-active agent, such as a penicillin or vancomycin, plus an aminoglycoside are necessary for killing; (5) resistance to all available drugs is increasing.
- Enterococcal endocarditis ordinarily requires 4 to 6 weeks of high-dose penicillin G or ampicillin, plus an aminoglycoside for cure (Table Standard Therapy for Endocarditis Due to Enterococcia). A 6-week course is recommended for patients with symptoms lasting longer than 3 months, recurrent cases, and patients with mitral valve involvement.
- In addition to isolates with high-level aminoglycoside resistance, β- lactamase-producing enterococci (especially Enterococcus faecium) are increasingly reported. If these organisms are discovered, use of vancomycin or ampicillin-sulbactam should be considered.
- Vancomycin-resistant enterococci, particularly E. faecium, are becoming more common.
Gram-negative Bacilli
- Endocarditis caused by gram-negative bacilli is relatively uncommon, although the incidence may be increasing. Patients at higher risk include intravenous drug abusers and those with prosthetic valves.
- The organism most commonly associated with gram-negative rod endocarditis in intravenous drug abusers is Pseudomonas aeruginosa. Other gram-negative bacilli causing Infective endocarditis include Salmonella spp., Escherichia coli, Citrobacter spp., Klebsiella-Enterobacter spp., Serratia marcescens, Proteus spp., and Providencia spp. Generally, these infections have a poor prognosis, with mortality rates as high as 60% to 80%.
- If medical management is implemented, large doses of a penicillin with activity against Pseudomonas (e.g. piperacillin 18 g/day) combined with an aminoglycosdie are necessary for an extended period (6 weeks).



