Description of Medical Condition
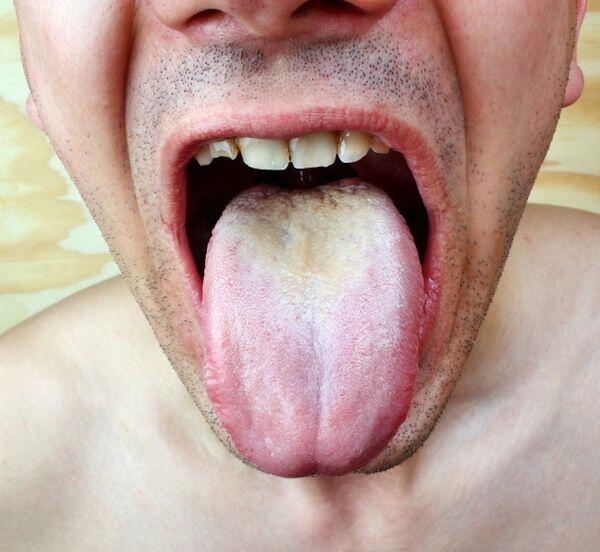
Candida albicans and related species cause a variety of infections. Cutaneous candidiasis syndromes include erosio interdigitalis blastomycetica, folliculitis, balanitis, intertrigo paronychia, onychomycosis, diaper rash, perianal candidiasis, and the syndromes of chronic mucocutaneous candidiasis. Mucous membrane infections include oral candidiasis (thrush), esophagitis, and vaginitis. The most serious manifestation of candidiasis is hematogenously disseminated invasive candidiasis (sometimes referred to as acute systemic candidiasis).
System(s) affected: Skin/Exocrine, Gastrointestinal, Reproductive, Pulmonary, Renal/Urologic
Genetics: N/A
Incidence/Prevalence in USA: Approximately 50/100,000. Hematogenously disseminated candidiasis affects at least 120,000 patients annually in the USA.
Predominant age: All ages are susceptible to hematogenously disseminated candidiasis. Premature neonates are at particularly high risk.
Predominant sex: Male = Female (hematogenously disseminated candidiasis)
Medical Symptoms and Signs of Disease
- Fever
- Malaise
- Tachycardia
- Hypotension
- Altered mental status
- Hepatosplenomegaly
- Maculopapular or nodular skin rash
What Causes Disease?
- Candida albicans is the most frequent pathogen. However, other important human pathogens include C tropicalis, C krusei, C. stellatoidea, C. pseudotropicalis, C. guilliermondi, C parapsilosis, C. lusitaniae, C. rugosa, C lambica, and Candida glabrata.
- Candida species colonize human mucocutaneous surfaces, and most infections are endogenously acquired from this reservoir
- Human-to-human transmission of Candida occurs in some settings
Risk Factors
For hematogenously disseminated invasive candidiasis:
- Oneutropenia
- Antibacterial chemotherapy
- Indwelling intravascular access devices
- Prior hemodialysis
- Mucocutaneous candidiasis
- Cardiothoracic or abdominal surgery
- Diabetes
- Hyperalimentation (TPN)
Non-albicans species are more prevalent in those with leukemia, neutropenia, and on fluconazole prophylaxis
Diagnosis of Disease
Differential Diagnosis
Includes a variety of cryptic bacterial infections and, in the neutro-penic host, multiple opportunistic infections
Drugs that may alter lab results: N/A
Disorders that may alter lab results: N/A
Pathological Findings
The charac teristic histopathology of lesions of Candida invasion of visceral organs is microabscess formation
Special Tests
- The diagnosis is established by isolating the causative organism from blood cultures (lysis/centrifugation blood cultures are superior to broth culture techniques for this purpose) or other normally sterile body sites, or by demonstration of organisms in histopathologic specimens of normally sterile tissues
- Isolation of Candida from multiple sites should raise the diagnostic suspicion of hematogenously disseminated invasive candidiasis
- Candida species isolated from a normally sterile site should be identified to the species level
- Fungal sensitivity testing should be employed in cases of persistent or recurrent Candida infections
- Azole resistant C. albicans species are reported with increasing frequency
- Fungal sensitivity testing should be employed for all cases of fungemia with Candida spp.
Imaging
Imaging techniques are generally not specifically useful in the diagnosis of hematogenously invasive disseminated candidiasis. However, in the syndrome of hepatosplenic candidiasis (chronic systemic candidiasis) imaging of the liver and spleen by liver scan, ultrasound, or CT (the most sensitive) may be useful in suggesting this syndrome as the cause of persistent fever and liver dysfunction in patients who have recently recovered from neutropenia.
Diagnostic Procedures
- If blood cultures remain consistently negative, exci-sional biopsy may be useful in diagnosis
- Aspiration and biopsy of skin lesions occasionally seen with hematogenously disseminated candidiasis is also useful
- Endoscopy with brushings and biopsy is useful in esophageal candidiasis
Treatment (Medical Therapy)
Appropriate Health Care
Inpatient for hematogenously invasive disseminated candidiasis
General Measures
- Fluid and electrolyte therapy is often required
- Hemodynamic and respiratory support may be required in seriously ill patients
- Removal of potentially infected intravascular access devices is imperative
Activity
As tolerated
Diet
No special diet
Patient Education
Patients should be advised of the nature of the infection and the toxicities associated with therapy
Medications (Drugs, Medicines)
Drug(s) of Choice
- Caspofungin (Cancidas)
- Useful as preferred therapy for candidemia in patients with prior azole therapy, immune compromised, neutropenia
- Initial therapy of choice for any patient with candidemia
- 70 mg IV load over 1 hour on day one followed by 50 mg IV daily
- Modify dose for severe hepatic insufficiency
- Fluconazole
- 400-800 mg IV daily for first week, followed by additional IV or oral therapy at the same dose for at least 2 weeks after last positive blood culture or last evidence of infection. Higher doses of fluconazole may be required if non-albicans species are known or suspected.
- Has been shown to be as effective as amphotericin B therapy and less toxic for treatment of candidemia in patients who are not neutropenic, do not have AIDS, and are not severely immunosuppressed by therapy after organ transplantation
- Amphotericin B
- Is an initial therapy of choice for any patient with candidemia and the preferred therapy for patients with neutropenia, severe immune compromise prior azole therapy
- Administer first in a test dose of 1 mg and then in incrementally increasing doses to 0.3-0.7 mg/kg/day. (Some authorities administer full dose after the test dose. In a critically ill patient, slow increase in dose is not warranted). Depending on host status and form of hematogenously invasive disseminated candidiasis. total dose requirement ranges from 200 mg to 2.0 gm over a therapeutic duration of 2-10 weeks.
Contraindications:
- The safety of amphotericin B therapy in pregnant patients has not been established
- Caspofungin is category C
Precautions:
- Amphotericin B
- Toxicity is formidable. Acute reactions occur commonly during initiation of therapy, including fever, rigors, and hypotension. These can be ameliorated or eliminated by premedication with acetaminophen, ibuprofen or hydrocortisone, and tend to decline over time with continuing daily therapy. Use meperidine if needed to abort rigors.
- Azotemia is a common complication and may be an indication for reducing therapy in some patients (to reduce toxicity, not because of renal elimination of drug). Generally recommended to hold drug if BUN > 40 mg/dL (14.3 mmol/L) or creatinine > 3.0 mg/dL (266 /jmol). Hold until above levels decline, then administer drug every other day. Maintenance of optimal fluid status and prevention of dehydration help minimize risk of azotemia. “Sodium loading” with 77 mEq (77 mmol) sodium daily (= 1 L1/2 normal saline) has been suggested by some authorities to decrease renal toxicity.
- Significant hypokalemia (often requires therapy) and renal tubular acidosis (rarely requires therapy) may develop. Significant hypomagnesemia may worsen hypokalemia.
- Anemia commonly develops in patients on protracted therapy but is almost always reversible
- Headache and phlebitis are common
- Leukopenia, thrombocytopenia, and liver function abnormalities are rarely encountered
- Itraconazole, voriconazole and caspofungin do not enter the urinary stream in sufficient concentrations to treat urinary tract infections
Significant possible interactions:
- Caspofungin — potentially important interactions with carbamazepine, phenytoin, cyclosporine, tacrolimus. sirolimus, NNRTIs, and rifampin
- Amphotericin B — concomitant therapy with cyclosporine or other nephrotoxic agents such as aminoglycoside or vancomycin may increase risk of amphotericin-induced nephrotoxicity
- Fluconazole — potentially important drug-drug interactions may occur in patients receiving oral hypoglycemics, coumarin-type anticoagulants, phenytoin, cyclosporine, rifampin, theophylline orterfenadine or astemizole. Drug-drug interactions are more likely with itraconazole and voriconazole
Alternative Drugs
- Liposomal preparations of amphotericin B appear to be less nephrotoxic
- Fluconazole therapy may be preferred for infections with C. lusitaniae, which may be resistant to amphotericin B
- Caspofungin or amphotericin B is preferred for infections with C. krusei which is likely resistant to fluconazole, as may be C. glabrata
- Other azole antifungals depending on activity and safety (itraconazole and voriconazole)
- Flucytosine may be used as adjunctive therapy with fluconazole for peritonitis
- Caspofungin in candidiasis. Data suggest that caspofungin is as effective as conventional amphotericin B for treatment of candidemia and is less frequently associated with adverse effects.
Patient Monitoring
Complete blood count, serum electrolytes, and serum creatinine should be measured at least twice weekly in patients on daily amphotericin B therapy. If blood cultures are positive, they should be repeated until negative.
Prevention / Avoidance
Fluconazole
liposomal amphotericin B and voriconazole reduce the incidence of candidiasis in patients undergoing induction therapy for acute leukemia or bone marrow transplantation
Possible Complications
- Of hematogenously disseminated candidiasis
- Pyelonephritis
- Endophthalmitis
- Endocarditis, myocarditis, pericarditis
- Arthritis, chondritis, osteomyelitis
- Pneumonitis
- Central nervous system infection
Expected Course / Prognosis
- Overall mortality for patients with hematogenously disseminated candidiasis is 40-75%, with mortality attributable to candidemia being 15-37%
Miscellaneous
Associated Conditions
See Risk Factors
Age-Related Factors
Pediatric: N/A
Geriatric: N/A
Pregnancy
N/A
International Classification of Diseases
112.5 Candidiasis, disseminated 112.9 Candidiasis of unspecified site
See Also
Candidiasis, mucocutaneous Vulvovaginitis, candidal
Other Notes
Other candidal infections: Intraperitoneal infection in patients with major abdominal surgery, biliary tract candidiasis, isolated lower urinary tract infection



