Essentials of Diagnosis
- Cigar-shaped yeast.
- Dimorphic: mycelial in nature, yeast in tissue.
- Associated with activities that involve contact with soil, sphagnum moss, decaying wood, or vegetation.
- Gardeners, forestry workers, miners, animal health care providers most at risk.
- Raised skin lesions with proximal spread along lymphatic channels.
- Recovery of microorganism from culture.
General Considerations
Epidemiology
Sporothrix schenckii, the causative agent of sporotrichosis, is a ubiquitous fungus commonly found in the soil, on sphagnum moss, on decaying wood, and on a variety of other vegetation. It is found worldwide but prefers a temperate or tropical climate with high humidity. Most cases of sporotrichosis are sporadic, but large human epidemics have been reported. Sporotrichosis has been reported in a variety of animal species including dogs, cats, horses, cows, camels, dolphins, goats, mules, birds, pigs, rats, and armadillo. Most human cases are secondary to vocational exposure. Gardeners, forestry workers, miners, laboratory workers, veterinarians, animal health technicians, and veterinary students are considered most at risk. Cases of zoonotic transmission as well as person-to-person transmission have been reported.
Microbiology
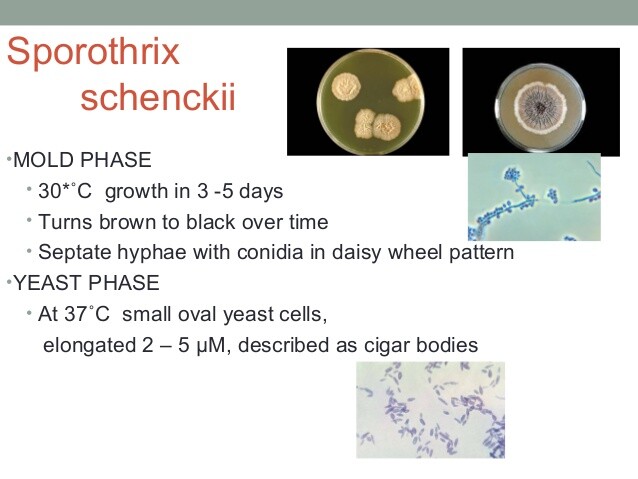
S schenckii is a dimorphic fungus. It forms mycelia (hyphal form) in vitro in temperatures <37 °C. It converts to its characteristic cigar-shaped yeast form in vivo and in cultures incubated at 37 °C. Colonies appear rapidly within 3-5 days of incubation. Moist and white at first, they develop a brown to black pigmentation with prolonged incubation.
Pathogenesis
Most cases of sporotrichosis result from direct inoculation of the fungus into the skin. Less frequently, access occurs through inhalation of spores leading to development of primary pulmonary infection.
CLINICAL SYNDROMES
S schenckii causes three distinct clinical syndromes: cutaneous, extracutaneous, and disseminated sporotrichosis (Box 1).
CUTANEOUS SPOROTRICHOSIS
Cutaneous sporotrichosis, the most common form of sporotrichosis, can present in one of two ways. In lymphangitic cutaneous sporotrichosis, lesions appear at the site of direct inoculation of the fungus into the skin. These initial lesions are often raised, erythematous, and warm. The organisms replicate locally, then advance proximally through the lymphatic channels, leading to the development of secondary lesions along these lymphatic channels. In the fixed form of cutaneous sporotrichosis, the organisms replicate locally but do not spread through the lymphatic channels.
Differential diagnosis includes skin infection caused by other fungi, skin infection caused by tuberculosis and atypical mycobacteria, bacterial skin infection, and foreign body granuloma.
EXTRACUTANEOUS SPOROTRICHOSIS
The main extracutaneous sites affected by sporotrichosis are the joints, lungs, and central nervous system. Other less commonly affected sites include the genitourinary tract, ocular adnexa, sinuses, larynx, and vocal cords.
OSTEOARTICULAR SPOROTRICHOSIS
The joints commonly affected are the joints of the hand, elbow, ankle, and knee. Onset is insidious, presenting with pain and swelling of a single joint with minimal fever or systemic toxicity. Over time, a sinus tract may develop and, if left untreated, other joints may be involved. Differential diagnosis includes rheumatoid arthritis, gout, and tuberculosis. Joint aspirations and synovial biopsies, often multiple, are required to establish the diagnosis.
PULMONARY SPOROTRICHOSIS
Pulmonary sporotrichosis can occur either as a primary lung infection subsequent to direct inhalation of S schenckii spores or in the setting of disseminated disease. Onset is insidious and associated symptoms include productive cough, fever, weight loss, fatigue, and malaise. Cavitary or nodular lesions involving the upper lobes, bilateral in about one third of the cases, are noted on chest roentgenograms. Conditions associated with pulmonary sporotrichosis include alcoholism, tuberculosis, chronic obstructive pulmonary disease, diabetes, sarcoidosis, steroid use, and malignancies.
CENTRAL NERVOUS SYSTEM SPOROTRICHOSIS
Central nervous system involvement is an uncommon complication of sporotrichosis and has been reported in the setting of alcoholism, AIDS, and Hodgkin’s disease. It presents as a chronic meningitis process with headache as the most common feature. Fever and neurologic deficits are unusual. Lymphocytic pleocytosis, a low glucose, and an elevated protein value are noted on cerebrospinal fluid analysis. Repeated lumbar punctures and cultures of large volume of cerebrospinal fluid are usually required to make a diagnosis.
DISSEMINATED SPOROTRICHOSIS
Immunosuppressed individuals, especially those with the acquired immunodeficiency syndrome and those with hematological malignancies, may present with widespread cutaneous disease as well as involvement of multiple organs, including the lungs, joints, and central nervous system. Blood cultures may occasionally be positive. Elevation of the erythrocyte sedimentation rate, anemia, and leukocytosis are noted on routine laboratory evaluation. Culture of skin lesions and joints is usually diagnostic.
Diagnosis
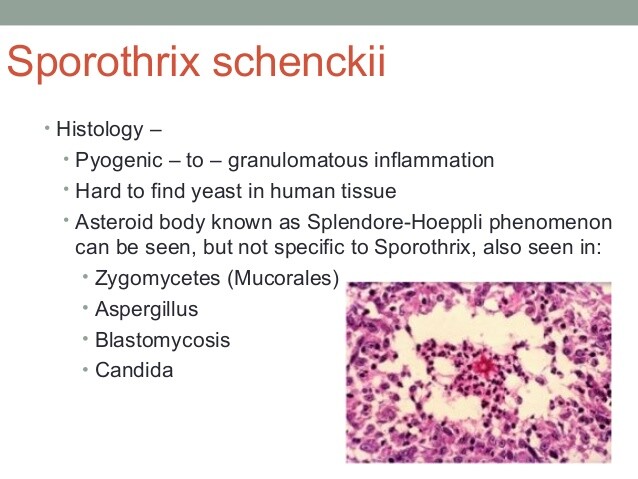
In patients with typical cutaneous syndrome of ascending lymphangitis, demonstration of the characteristic appearance of the microorganism on stains performed on tissue biopsy is highly suggestive of diagnosis. Definitive diagnosis requires recovery of microorganisms from culture. Multiple attempts to isolate the organisms may be necessary.
Several serologic testing procedures such as agglutination tests, ELISA, complement fixation, precipitation, and immunodiffusion tests have been developed to aid in the diagnosis of sporotrichosis. While these may prove to be useful, especially in the diagnosis of meningitis, methodologies have not been standardized, and they have not yet found wide clinical application.
Skin tests are useful only as an epidemiological tool.
Treatment
Several therapeutic modalities such as local treatment, systemic therapy, and surgery have been used for the treatment of sporotrichosis (Box 2).
A saturated solution of potassium iodide (SSKI) is an effective regimen for cutaneous disease. Its mechanism of action is not well understood. SSKI drops are taken orally, and the dose is progressively increased to a maximum tolerated dose. Treatment is continued until the resolution of the skin lesions.
More recently, itraconazole, a triazole antifungal agent, has become the drug of choice for treatment of lymphocutaneous sporotrichosis. As stated above, treatment should be continued until resolution of infection, which usually takes 3-6 months. Itraconazole has been shown to be effective therapy for cutaneous as well as visceral sporotrichosis, with the exception of meningitis.
Osteoarticular sporotrichosis requires treatment with itraconazole or amphotericin B, but relapses can occur. There have been reports of successful treatment of osteoarticular sporotrichosis with intra-articular instillation of amphotericin B. Patients with pulmonary sporotrichosis should be treated with either itraconazole or amphotericin B, depending on the severity of their infection. Surgical resection may be necessary. Patients with disseminated disease should be treated with intravenous amphotericin B. Itraconazole may be an acceptable alternative if they are not acutely ill.
Terbinafine, an allylamine antifungal agent, has successfully been used to treat both the fixed and lymphatic forms of cutaneous sporotrichosis. Treatment of meningitis caused by S schenckii requires the use of intravenous amphotericin B. The addition of 5-fluorocytosine may be necessary. There are no data on the role of azoles in this setting.
Sporotrichosis in the setting of AIDS responds poorly to all therapeutic modalities. Amphotericin B is the drug of choice; itraconazole can be used in less severe cases. After induction therapy with amphotericin B, treatment needs to be continued with itraconazole, indefinitely, to prevent relapse.
Local heat therapy (ie, application of heat, for example, in the form of a warm pack) directly on the affected skin lesion, can be useful either as an adjunct therapy to other forms of therapy or as an alternative treatment in pregnant women, in whom the use of SSKI and azoles is contraindicated.
Prognosis
Prognosis is variable and difficult to generalize. Disseminated sporotrichosis, if untreated, causes death.
Prevention & Control
Avoiding direct skin contact with known sources of S schenckii (eg, sphagnum moss) and wearing protective gloves and long sleeves in occupational or recreational activities, such as handling of rose bushes, wires, decayed wood, and vegetation, may help prevent sporotrichosis (Box 3).
BOX 1. Syndromes in Sporothricosis
More Common
- Cutaneous sporothricosis: lymphangitic form and fixed form
Less Common
- Extracutaneous sporothricosis: osteoarticular, pulmonary, and central nervous system
- Disseminated
BOX 2. Treatment of Sporothricosis
Cutaneous
Osteoarticular
Pulmonary
Central Nervous
System
Disseminated
First Choice
- Itraconazole (100-200 mg once daily)
- Itraconzaole (200 mg twice daily)
- Itraconazole (200 mg twice daily)
- Amphotericin B (1-2 g) total
- Amphotericin B (1-2 g) total
Second Choice or Adjunct
- SSKI, 5-10 drops orally 3 times/d; advance gradually to 40-50 drops 3 times/d (for adults)
- Terbinafine (250 mg twice daily)
- Hyperthermia
- Amphotericin B (1-2 g) total2
- Amphotericin B (1-2 g) total
- Surgical resection
- Itraconazole (200 mg twice daily)3
- Itraconazole (200 mg twice daily)
1The addition of 5-fluorocytosine may be necessary.
2Intra-articular amphotericin B is used occasionally. Total doses of amphotericin B are required at a minimum.
3No data are available on the use of itraconazole for central nervous system infections.
BOX 3. Sporotrichosis: Prevention
Precautions
Avoid direct skin contact with and wear gloves and long sleeves when handling known sources of schenckii, eg decayed wood or vegetation.
Prophylaxis
AIDS patients with sporotrichosis who have completed initial therapy should receive life-long suppressive treatment with itraconazole.