Description of Medical Condition
Amebiasis is caused by the intestinal protozoan, Entamoeba histolytica. Infection results from ingestion of fecally contaminated food, such as garden vegetables or by direct fecal-oral transmission. Most persons are asymptomatic or have minimal diarrheal symptoms. In a few patients, invasive intestinal or extraintestinal (e.g., liver, and less commonly kidney, bladder, male or female genitalia, skin, lung, brain) infection results. Amebic abscess of the liver may develop during the acute attack or 1 -3 months later; symptoms may be abrupt or insidious. Entamoeba histolytica has been divided into ‘pathogenic” and “nonpathogenic” strains. The pathogenic strains commonly cause invasive infection while the noninvasive strains cause only asymptomatic intestinal infection. More recently, the nonpathogenic strains have been assigned to a separate species, E. dispar. Unfortunately, the species cannot be distinguished in a routine clinical laboratory.
System(s) affected: Gastrointestinal, Renal/Uro-logic, Reproductive, Skin/Exocrine, Nervous
Genetics: N/A
Incidence/Prevalence in USA: Probably <1% overall, but much higher in some risk groups, such as areas with large immigrant populations
Predominant age: All
Predominant sex: Male > Female; probably because of greater occupational exposure
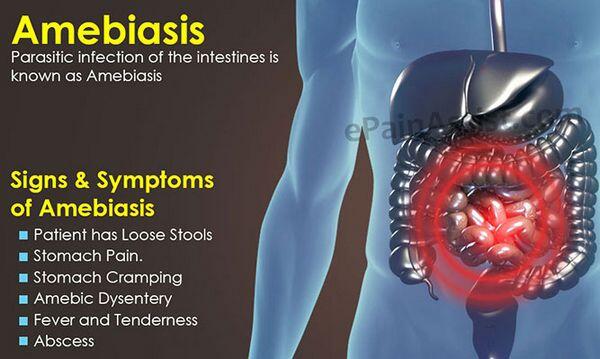
Medical Symptoms and Signs of Disease
- Noninvasive infection (up to 99%)
- Asymptomatic (90%)
- Mild diarrhea
- Abdominal discomfort
- Invasive intestinal infection
- Abdominal pain and tenderness
- Rectal pain
- Diarrhea
- Bloody stools
- Fever (30%)
- Systemic toxicity
- Extraintestinal infection
- Fever
- Systemic toxicity
- RUQ abdominal pain and tenderness
- Nausea and vomiting
- Diarrhea (50%)
- Hematuria, dysuria, urinary frequency and urgency
What Causes Disease?
Infection with Entamoeba histolytica is transmitted through contaminated food or water, or through person-to-person contact
Risk Factors
- Low socioeconomic status
- Institutional living
- Male homosexuality
- Invasive disease is more common in certain geographic locations, including some parts of Mexico, South Africa, and India
Diagnosis of Disease
Differential Diagnosis
- Other infectious causes of colitis, including shigellosis. Campylobacter infection, pseudomembranous colitis, and occasionally salmonellosis or Yersinia infection
- Noninfectious causes of colitis include ulcerative colitis. Crohn colitis and ischemic colitis
- Hepatic amebiasis must be distinguished from pyogenic liver abscess or superinfection of amebic abscess
Laboratory
- Stool for ova and parasites (unfortunately, the sensitivity of this exam is poor). Diarrheal stool should be examined immediately for trophozoites in addition to fixed stool specimens (repeated as necessary). In invasive intestinal infection, stools are bloody, but fecal leukocytes are usually absent.
- Serologic tests (especially indirect hemagglutination [HA]), positive in 85% of colitis patients and most patients with extraintestinal disease. Serologic tests should be done in patients with idiopathic inflammatory bowel disease to rule out amebiasis.
- In bladder infections-amoebae and/or cysts in urine
- Liver enzymes and alkaline phosphatase may be elevated in hepatic disease
Drugs that may alter lab results: Many drugs interfere with stool exams
Disorders that may alter lab results: N/A
Pathological Findings
- Colon biopsy
- Lysis of mucosal cells (flask ulcers)
- PAS-stained trophozoites
- Oneutrophils at the periphery
- Liver biopsy
- Onecrosis surrounded by a rim of trophozoites
- Liver aspirate — red-brown material (anchovy paste)
Imaging
CT scan or ultrasound for hepatic infection
Diagnostic Procedures
- Rectosigmoidoscopy with biopsy
- Needle aspirate of hepatic lesions may be needed to rule out pyogenic infection or superinfection
Treatment (Medical Therapy)
Appropriate Health Care
Outpatient
General Measures
- Fluids and nutrition
- Electrolyte management
Surgical Measures
With severe amebic colitis, surgery may be necessary
Activity
In accordance with illness of patient
Diet
As tolerated
Patient Education
Avoid conditions of re-exposure
Medications (Drugs, Medicines)
Drug(s) of Choice
- Noninvasive infection
- Diiodohydroxyquin [also called iodoquinol] 650 mg tid for 20 days
- Invasive infection
- Metronidazole (Flagyl) 750 mg tid for 5-10 days, followed by a 20 day course of diiodohydroxyquin to eliminate intestinal carriage
- Tinidazole (Tindamax) 2 gm daily for 3 days with food for intestinal infection and 2 gm daily for 3-5 days for liver abscess
Contraindications:
- Diiodohydroxyquin — use cautiously in patients with thyroid diseases. Contraindicated in hepatic or renal dysfunction. May cause optic neuritis or peripheral neuropathy.
- Known allergy to given medication
Precautions: None of the agents are proven safe in pregnancy, but pregnant women with invasive disease should still be treated
Significant possible interactions:
- Metronidazole-ethanol: disulfiram reaction
Alternative Drugs
- Noninvasive infection
- Diloxanide 500 mg tid for 10 days
- Paromomycin 500 mg tid for 10 days
- Invasive infection
- Dehydroemetine (as effective as metronidazole, but cardiotoxic) 1-1.5 mg/kg/day IM for 5 days
- Chloroquine (less effective) 600 mg base/day for 2 days, then 200 mg/day for 2-3 weeks. Children 10 mg/kg/day up to maximum of 300 mg/day.
Patient Monitoring
Patient signs and symptoms, stool for ova and parasite
Prevention / Avoidance
Avoid risk factors when possible
Possible Complications
- Toxic megacolon with rupture
- Rupture of hepatic abscess which may perforate into subphrenic space, right pleural cavity or other nearby organs
- Bladder perforation, urethral strictures, vesicointestinal fistula
Expected Course / Prognosis
Untreated invasive amebiasis is frequently fatal. With treatment, improvement usually occurs within a few days. Some patients with amebic colitis have irritable bowel symptoms for weeks after successful treatment. Relapses possible.
Miscellaneous
Associated Conditions
N/A
Age-Related Factors
Pediatric: More severe in neonates
Geriatric: More severe in elderly
Others: More severe in patients on corticosteroids and other immunocompromised patients
Pregnancy
More severe in pregnancy. Most agents are avoided in pregnancy (especially first trimester) because of concerns of teratogenicity, but invasive disease must still be treated. Paromomycin is sometimes recommended for noninvasive disease because it is not absorbed. Infectious disease consultation should be obtained.
Synonyms
- Amebic colitis
- Amebic dysentery
International Classification of Diseases
006.0 Acute amebic dysentery without mention of abscess
006.3 Amebic liver abscess
006.4 Amebic lung abscess
006.5 Amebic brain abscess
006.6 Amebic skin ulceration
006.8 Amebic infection of other sites
006.9 Amebiasis, unspecified
See Also
Diarrhea, acute Diarrhea, chronic



