Description of Medical Condition
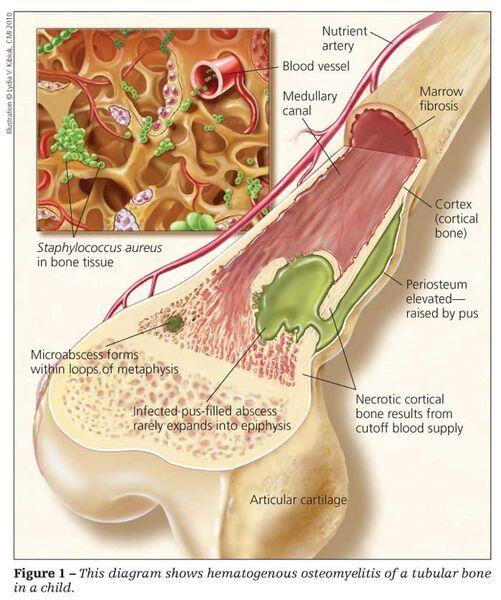
Osteomyelitis is an acute or chronic infection of the bone and its structures caused most commonly by bacteria and rarely by other microorganisms. This infection may be acquired either by hematogenous, contiguous, or direct inoculation such as trauma or surgery.
System(s) affected: Musculoskeletal
Genetics: There is no genetic predisposition known in this disease
Incidence/Prevalence in USA: Uncommon
Predominant age: This infection is commonly seen in older adults; hematogenous is bimodal, also seen in infants and children
Predominant sex: Males > Females
Medical Symptoms and Signs of Disease
- Hematogenous long bone infection in children
- Abrupt onset of high fever
- Irritability
- Malaise
- Restriction of movement of the involved extremity
- Signs of localized inflammation
- Hematogenous vertebral infection in adults
- Illness is insidious and behaves more like a chronic infection
- History of an acute bacteremic episode associated with infection of a specific organ may be found in some patients
- Contiguous and vascular insufficiency associated infection
- Acute constitutional manifestations are seldom seen
- Localized signs and symptoms of inflammation with or without drainage frequently found
- Chronic osteomyelitis
- Non-healing ulcer or draining sinus
- Constitutional symptoms, when present, indicate acute suppurative condition in the bone or surrounding tissues
- Prosthetic device associated infection
- Infection may be acquired either by hematogenous route, or by contiguous foci such as local infection, operative contamination, or postoperative infection
- Acute postoperative infection may present as fever, localized swelling, tenderness, and drainage
- Chronic infection is characterized by joint discomfort, swelling, erythema, and joint dysfunction
What Causes Disease?
- Acute hematogenous osteomyelitis
- Staphylococcus aureus (most common)
- Streptococcus, coagulase negative Staphylococcus. Haemophilus influenzae, and gram negative organisms (less common)
- Vertebral osteomyelitis
- Staphylococcus aureus and gram negative enteric organisms (common)
- Other microorganisms to consider include Mycobacterium tuberculosis, and fungi
- Contiguous focus osteomyelitis and vascular insufficiency osteomyelitis
- Mixed aerobic/anaerobic microorganisms are frequently found
- Prosthetic device infection
- Coagulase negative Staphylococcus, and S. aureus (most common)
- Diphtheroids, and gram negative bacteria (less common)
Risk Factors
- Diabetes mellitus
- Sickle cell disease
- Other conditions which predispose to bone infarcts
- IV drug use
- Hemodialysis
- Local trauma
- Open fractures
- Presence of prosthetic orthopedic implant
- Vascular insufficiency
- Neuropathy
Diagnosis of Disease
Differential Diagnosis
- Systemic infection from other source
- Aseptic bone infarction
- Localized inflammation or infection of overlying skin and soft tissues
- Neuropathic joint disease
- Fractures
- Gout
Laboratory
- Definitive diagnosis is made by needle aspiration or bone biopsy and demonstration of the microorganism by culture or histology
- Blood culture may be positive in about 50% of younger patients with acute hematogenous disease
- Leukocyte count is usually elevated in the acute cases, but not in the chronic cases
- Sedimentation rate or c-reactive protein is usually elevated, but non-specific
Drugs that may alter lab results: Antimicrobial agents given before bone culture
Disorders that may alter lab results:
- Cultures from the sinus tract are unreliable because of frequent contamination
- Superficial cultures only helpful in identifying methicillin-resistant S. aureus
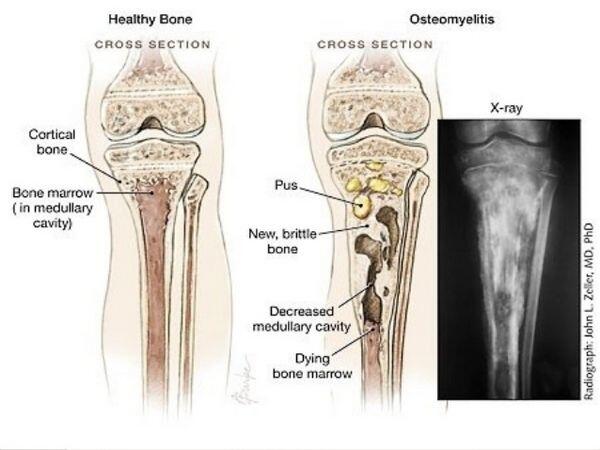
Pathological Findings
Inflammatory process of the bone with pyogenic bacteria
Imaging
- No technique can absolutely confirm or exclude osteomyelitis
- Radiographic — routine x-ray (findings on plain x-ray often delayed for 10-14 days in acute infection)
- Radionuclide scanning (technetium, indium, or gallium) are also useful, but limited by low specificity
- CT with good resolution, artifact may decrease specificity
- MRI excellent, more expensive than other radiologic tests
Diagnostic Procedures
Needle biopsy or open bone biopsy for bacterial culture (which is the “gold standard”). However, antibiotic therapy within the past 2-4 weeks may prevent isolation of a specific pathogen.
Treatment (Medical Therapy)
Appropriate Health Care
Hospital ize the patient with suspected acute osteomyelitis for diagnostic work-up and initial treatment
General Measures
Symptomatic treatment of pain
Surgical Measures
- Surgical drainage and removal of necrotic tissues are of utmost importance to effect cure
- In patients with vascular insufficiency or severe gangrenous infection, amputation may be the only effective treatment
- Revascularization may be an option for some patients
Activity
Bedrest and immobilization of the involved bone and joint
Diet
No restriction
Patient Education
Stress need for long-term treatment and follow up
Medications (Drugs, Medicines)
Drug(s) of Choice
These are essentially empiric choices; recommendations based on data from a small number of studies. Antimicrobial agent/agents based on susceptibility testing and known clinical efficacy. The duration of therapy for acute osteomyelitis should be at least 4-6 weeks. In chronic osteomyelitis, longer duration of therapy may be needed.
- Staphylococcus aureus and coagulase negative staphylococcus: nafcillin 2 g IV q4-6h. Vancomycin 1 g q12h for methicillin resistant Staph.
- Streptococcus spp.: penicillin G 2-4 million units q4h IV
- Enteric gram negative bacilli and Pseudomonas aerugi-nosa: piperacillin 4 g q4-6h IV, plus aminoglycoside
- Mixed aerobic/anaerobic infection (diabetic foot, bite wound): beta-lactamase inhibitor combination (ticarcil-lin-clavulanate 3.1 g q6h IV; ampicillin-sulbactam 3 g q6h IV); piperacillin-tazobactam 3.375 g q6h IV
Contraindications: Allergy
Precautions: In patients with renal or hepatic insufficiency, antimicrobial dose may need adjustment
Significant possible interactions: Refer to manufacturer’s literature
Alternative Drugs
- Staphylococcus aureus and coagulase negative staphylococcus: clindamycin 600 mg IVq6h, nafcillin 2 g q4h, or cefazolin 1 g q8h IV, or vancomycin 1 gq12h or linezolid (Zyvox) 600 mg po bid or IV bid
- Streptococcus spp.: penicillin G 2 million units q4h, cefazolin 1 g q8h IV, or clindamycin 600 mg q6h IV
- Enteric gram negative bacilli and Pseudomonas aeru-ginosa: ceftazidime 1 g q8h IVorciprofloxacin [or other quinolone] 750 mg q12h orally.
- Mixed aerobic/anaerobic infection (diabetic foot, bite wound): clindamycin plus third generation cephalospo-rin or quinolone
- Home therapy often used — consider a simplified antibiotic regimen for outpatient use or oral therapy
- Some published studies recommend use of hyperbaric oxygen (HBO), but none are randomized, controlled trials
Patient Monitoring
Blood level of antimicrobial agents, serum antibacterial titers, sedimentation rate, repeat plain x-ray, CT or MRI to confirm healing
Prevention / Avoidance
Avoid further stress and weight bearing until healing
Possible Complications
- Abscess formation
- Bacteremia
- Fracture
- Loosening of the prosthetic implant
- Postoperative infection
Expected Course / Prognosis
- Cure of osteomyelitis with medical treatment is notoriously unpredictable especially when not accompanied by surgical debridement
- In patients with acute hematogenous osteomyelitis, the prognosis is usually good even without surgery. Cure takes about 6 weeks. X-ray improvement may take 3-6 months.
- The prognosis is improved if all infected bone has been removed
Miscellaneous
Associated Conditions
Listed with Causes
Age-Related Factors
Pediatric:
Occurs most often in 5-14 age group and more frequently in boys
Geriatric:
- Vertebral osteomyelitis more common
- Contiguous focus of infection more common
- Vascular insufficiency is most common cause of osteomyelitis in 50-70 age group (usually due to presence of associated conditions)
Pregnancy:
N/A
International Classification of Diseases
730.00 Acute osteomyelitis, site unspecified
730.10 Chronic osteomyelitis, site unspecified
526.4 Inflammatory conditions of jaws
376.03 Orbital osteomyelitis





