Description of Medical Condition
PID is a clinical syndrome caused by the ascent of microorganisms from the vagina and endocervix to the endometrium, fallopian tubes, ovaries, and contiguous structures. PID is a broad term that includes a variety of upper genital tract infections, unrelated to pregnancy or surgical procedures, such as salpingitis, salpingo-oophoritis, endometritis, tubo-ovarian inflammatory masses, and pelvic or diffuse peritonitis.
Pathogenesis
The precise mechanism by which microorganisms ascend from the lower genital tract is not known. One possibility is that chlamydial or gono-coccal endocervicitis alters the defense mechanisms of the cervix allowing ascent of the vaginal flora with or without the original pathogen. Other possibilities suggest that polymicrobial infection can occur without N. gonorrhoeae or C. trachomatis. Factors that predispose to the ascent of bacteria include the use of an intrauterine device (IUD) and the hormonal and physical changes associated with menstruation.
System(s) affected: Reproductive
Genetics: N/A
Incidence/Prevalence in USA: Estimated 1 million women are treated each year; 100-200/100,000
Predominant age: One-third younger than 20 years, two-thirds younger than 25 years
Predominant sex: Female only
Medical Symptoms and Signs of Disease
- May be asymptomatic
- Lower abdominal pain
- Fever and malaise
- Vaginal discharge
- Irregular bleeding
- Urinary discomfort, proctitis
- Nausea and vomiting
- Abdominal tenderness
- Tenderness with cervical motion
- Adnexal tenderness
- Unilateral or bilateral tender adnexal mass
What Causes Disease?
Bacteriology — multiple organisms act as etiologic agents in PID and most cases are polymicrobial. Chlamydia trachomatis, Neisseria gonorrhoeae, and a wide variety of aerobic and anaerobic bacteria are recognized as etiologic agents. Myco-plasmas have also been implicated but their role is less clear. The proportion of cases infected with chlamydia or gonorrhea varies widely depending on the population studied. The most common anaerobes include Bacteroides, Peptostreptococcus, and Peptococcus species. The organisms involved in bacterial vaginosis are similar to the nongonococcal, nonchlamydial bacteria often found in the upper genital tract of women with PID, but the relationship between these conditions is unclear.
Risk Factors
- Sexually active, reproductive age
- Most common in adolescents
- Multiple sexual partners
- Use of an IUD, greatest risk in first few months after insertion
- Previous history of PID; 20-25% will have a recurrence
- Chlamydial or gonococcal cervicitis; 8-10% will develop PID
- Gonococcal salpingitis occurs commonly within 7 days of onset of menses
- Condoms and vaginal spermicides lessen the risks of PID
- Oral contraceptives may reduce the risk of PID
Diagnosis of Disease
Differential Diagnosis
- Appendicitis
- Ectopic pregnancy
- Ovarian torsion
- Hemorrhagic or ruptured ovarian cyst
- Endometriosis
- Irritable bowel syndrome
- Somatization disorder
Laboratory
- Pregnancy test
- Leukocyte count greater than 10,000 cells per mm3
- Endocervical gram stain for gram-negative intracellular diplococci
- ESR of 15 mm/hour or higher
- Endocervical culture for gonorrhea
- Endocervical culture or antigen test for chlamydia
- Plasma cell endometritis on endometrial biopsy
Drugs that may alter lab results: N/A
Disorders that may alter lab results: N/A
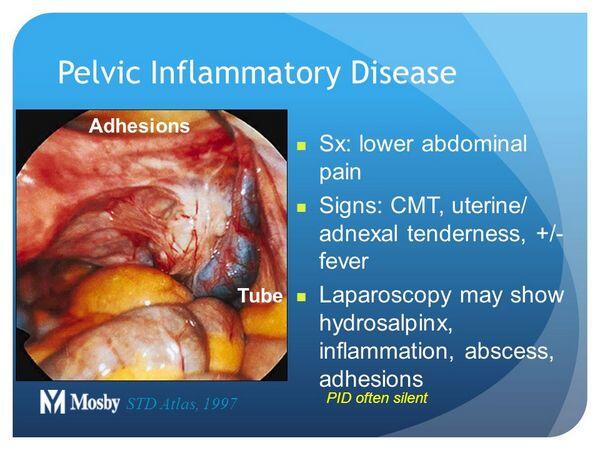
Pathological Findings
N/A
Special Tests
- Culdocentesis with culture of aspirated material
- Diagnostic laparoscopy with culture of fallopian tubes
Imaging
Pelvic ultrasound
Diagnostic Procedures
- PID diagnosis is elusive and even asymptomatic patients are at risk for sequelae. Diagnosis incorrect in up to a third of women diagnosed. Laparoscopic diagnosis best but impractical as routine and generally reserved for problem situations. In general, wiser to over-treat lower tract genital infection than to miss an upper tract infection.
- Suggested criteria for diagnosis (sufficient for empiric treatment):
- Uterine/adnexal tenderness, or
- Cervical motion tenderness
- Additional criteria:
- Temperature greater than or equal to 38°C
- WBC greater than or equal to 10,500/mm3
- Purulent material by culdocentesis
- Adnexal mass
- ESR > 15 mm/hour
- Laboratory evidence of gonorrhea or chlamydia
- Elevated C-reactive protein
- Definitive criteria:
- Histopathologic endometritis on biopsy
- Adnexal abscess on sonography
- Laparoscopic evidence of PID
Treatment (Medical Therapy)
Appropriate Health Care
- Outpatient, normally
- Hospitalization recommended in the following situations:
- Uncertain diagnosis
- Surgical emergencies cannot be excluded, e.g., appendicitis
- Suspected pelvic abscess
- Pregnancy
- Adolescent patient with uncertain compliance with therapy
- Severe illness
- Cannot tolerate outpatient regimen
- Failed to respond to outpatient therapy
- Clinical follow-up within 72 hours of starting antibiotics cannot be arranged
- HIV-infected
General Measures
- Avoidance of sex until treatment is completed
- Insure that sex partners are referred for appropriate evaluation and treatment. Partners should be treated, irrespective of evaluation, with regimens effective against chlamydia and gonorrhea.
Surgical Measures
- Reserved for failures of medical treatment and for suspected ruptured adnexal abscess with resulting acute surgical abdomen
- Conservative surgery preferred. This allows a 10-15% postoperative fertility rate.
- Hysterectomy and adnexectomy for older patients with completed childbirth
- Failure of medical therapy generally associated with adnexal abscess which may be amenable to trans-abdominal ortransvaginal drainage under guidance by ultrasonography, computerized tomography, or laparoscopy
Activity
According to severity of illness
Diet
According to severity of illness
Medications (Drugs, Medicines)
Drug(s) of Choice
Several antibiotic regimens are highly effective with no single regimen of choice, but coverage should include chlamydia, gonorrhea, anaerobes, gram-negative rods, and streptococci. The CDC regimens that follow are recommendations and the specific antibiotics named are examples.
- Parenteral; regimen A
- Cefoxitin 2 g IV every 6 hours or cefotetan IV 2 g every 12 hours (or other cephalosporins such as ceftizoxime, cefotaxime, and ceftriaxone) plus doxycycline 100 mg orally or IV every 12 hours
- Therapy for 24 hours after clinical improvement and doxycycline continued after discharge for a total of 10-14 days
- Parenteral; regimen B
- Clindamycin 900 mg IV every 8 hours plus gentami-cin loading dose IV or IM (2 mg/kg of body weight) followed by a maintenance dose (1.5 mg/kg) every 8 hours
- Therapy for 24 hours after clinical improvement with doxycycline after discharge as above, or clindamycin 450 mg orally qid for a total of 14 days
- Outpatient treatment; regimen A
- Ofloxacin 400 mg orally bid for 14 days or levo-floxacin 500 mg orally once daily for 14 days with or without metronidazole 500 mg orally bid for 14 days
- Outpatient treatment; regimen B
- Cefoxitin 2 g IM plus probenecid, 1 g orally, concurrently or ceftriaxone 250 mg IM or equivalent cepha-losporin plus doxycycline 100 mg orally bid for 10-14 days with or without metronidazole 500 mg orally bid for 14 days
Contraindications: Refer to manufacturer’s profile of each drug
Precautions: Refer to manufacturer’s profile of each drug
Significant possible interactions: Refer to manufacturer’s profile of each drug
Alternative Drugs
Many other antibiotic regimens have been proposed and used with success. For example, tobramycin in place of gentamicin, tetracycline in place of doxycycline.
Patient Monitoring
- Close observation of clinical status, in particular for fever, symptoms, level of peritonitis, white cell count
- Follow adnexal abscess size and position with ultraso-nography
Prevention / Avoidance
- Educational programs about safe sex practices
- Education, particularly for those who have had an episode of PID
- IUD contraindicated in women with history of PID or lifestyle associated with STD
- Oral contraceptive appears to decrease risk of PID in cases with cervicitis and the PID cases which do occur are generally less severe
- Barrier contraceptives, especially condoms, and spermicidal creams or sponges provide protection, the extent of which is not well documented
- Insure evaluation and treatment of sex partners
- Comply with management instructions
- Seek medical care early when genital lesions or discharge appear
- Seek routine check-ups for STD if in non-mutually monogamous relationship(s)
Possible Complications
- A tubo-ovarian abscess will develop in approximately 7-16% of patients
- Recurrent infection occurs in 20-25% of patients
- Risk of ectopic pregnancy increased by 7-10-fold to about 8% of women who have had PID
- Tubal infertility in 15, 35, and 55% of women after one, two, and three episodes of PID, respectively
- Chronic pelvic pain in 20% related to adhesion formation, chronic salpingitis, or recurrent infections
Expected Course / Prognosis
- Wide variation with good prognosis if early, effective therapy instituted and further infection avoided
- Poor prognosis related to late therapy and continued unsafe lifestyle
Miscellaneous
Associated Conditions
- In PID patients with an IUD in situ, especially if an adnexal abscess is present, the possibility of actinomyces infection requiring penicillin treatment must be kept in mind
- The IUD is contraindicated in women with a previous episode of PID
- Rupture of an adnexal abscess is rare but life-threatening. Early surgical exploration is mandatory.
- Chlamydia or gonococcal perihepatitis may occur with PID. This combination is termed the Curtis-Fitz-Hugh Syndrome.
Age-Related Factors
Pediatric:
- PID is rare before puberty
- Adolescents are highly vulnerable to sexually transmitted diseases (STD) including PID. Early vigorous therapy to prevent infertility is especially important in this age group.
Geriatric:
PID is rare after menopause, although postmenopausal adnexal abscess is a well-documented entity
Pregnancy
PID is rare during pregnancy but occurs occasionally and the possibility must be kept in mind
Synonyms
- Salpingitis
- Salpingo-oophoritis
- Adnexitis
- Pyosalpinx
- Tubo-ovarian abscess
- Pelvic peritonitis
International Classification of Diseases
614.9 Unspecified inflammatory disease of female pelvic organs and tissue
See Also
Chlamydial sexually transmitted diseases
Gonococcal infections
Syphilis




