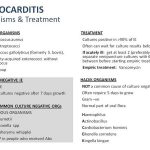
The most important approach to treatment of Infective endocarditis includes isolation of the infecting pathogen and determination of antimicrobial susceptibilities, followed by high-dose, bactericidal antibiotics for an extended period.
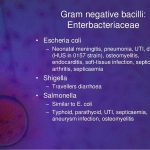
Central nervous system infections include a wide variety of clinical conditions and etiologies: meningitis, meningoencephalitis, encephalitis, brain and meningeal abscesses, and shunt infections. The focus of this chapter is meningitis. N. meningitidis meningitis is the leading cuase of bacterial meningitis in children and young adults in the United States.
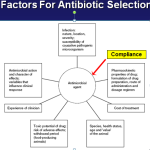
A generally accepted systematic approach to the selection and evaluation of an antimicrobial regimen is shown in Table Systematic Approach for Selection of Antimicrobials. An «empiric» antimicrobial regimen is begun before the offending organism is identified, while a «definitive» regimen is instituted when the causative organism is known. The use of combinations to prevent the emergence of resistance is widely applied but not often realized. The only circumstance where this has been clearly effective is in the treatment of tuberculosis.
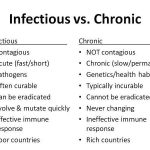
Infectious diseases comprise those illnesses that are caused by microorganisms or their products. Clinical manifestations of infection occur only when sufficient tissue injury has been inflicted directly by microbial products (e.g., endotoxins and exotoxins), or indirectly by host responses (e.g., cytokines and hydrolytic enzymes released by polymorphonuclear leukocytes). Despite the extraordinary recent advances that have occurred in therapeutics for infectious diseases, a number of basic principles should be followed to prescribe antimicrobials and vaccines is an optimal manner.
Before appropriate therapy can be given for an infectious disease, consideration of epidemiologic factors is essential. This section does not fully discuss the epidemiology (the determinants, occurrence, distribution, and control of health and disease) of infectious diseases. However, a number of basic principles and historical points are worth emphasizing.
A wide variety of antimicrobial agents is available to treat established infections caused by bacteria, fungi, viruses, or parasites. This section will cover the general principles of antimicrobial therapy and will also include illustrative clinical problems to emphasize proper decision-making in using antimicrobials.
The mechanisms associated with common adverse reactions to antimicrobials include dose-related toxicity that occurs in a certain fraction of patients when a critical plasma concentration or total dose is exceeded, and toxicity that is unpredictable and mediated through allergic or idiosyncratic mechanisms. For example, certain classes of drugs such as the aminoglycosides are associated with dose-related toxicity.
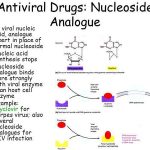
Nucleoside analog reverse transcriptase inhibitors have formed the backbone of anti-human immunodeficiency virus therapy for the last decade (see Table Characteristics of Nucleoside Reverse Transcriptase Inhibitors). Reverse transcription is necessary for human immunodeficiency virus RNA to be used as a template to produce viral DNA, which can be integrated into the cellular genome.