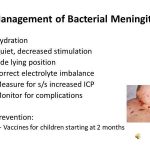
Meningitis used to be a disease that occurred primarily in children younger than 12 years. The advent of a vaccine for Haemophilus influenzae has led to a marked change in the epidemiology of meningitis in developed countries.
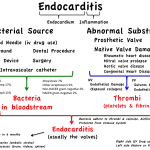
Infective endocarditis is a microbial infection of the endothelial lining of the heart. The characteristic lesion is a vegetation (a mass comprised of fibrin, platelets, microorganisms and their product or products on a valve leaflet). Multiple valves may be involved, as may any part of the endothelium of the heart.
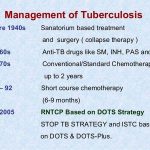
Tuberculosis was a disappearing disease in North America until the early 1980s. However, the spread of human immunodeficiency virus infection has changed that. From 1985 to 1992 there was an increase in the number of cases of tuberculosis reported in the United States, and most of these cases were in New York, New Jersey, Texas, Florida, and California. The other major change in the epidemiology of tuberculosis has been the emergence of multidrug-resistant disease.
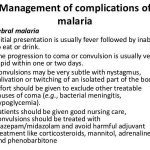
Malaria is a protozoan (genus Plasmodium) infection transmitted by the bite of an infected female Anopheles mosquito and rarely via a contaminated blood transfusion. It is extremely common, affecting more than 500 million persons and resulting in more than 1 million deaths each year. There are four species of the genus Plasmodium that cause malaria in man.
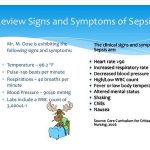
Sepsis, sepsis syndrome, septic shock, and multiorgan dysfunction are all part of a continuum of infection-related systemic illness. Table Definitions for Sepsis, Sepsis Syndrome, Septic Shock and Multiorgan Dysfunction Syndrome gives definitions for each of these entities. The pathogenesis of sepsis is very complex, involving a large number of mediators.
Adequate response to immunization is most frequently judged by measuring the development of specific serum immunoglobulins (e.g., antibodies) following a course of administration of vaccine. The concentration of specific immunoglobulin in plasma is usually proportional to the degree of protection from the viral agent.
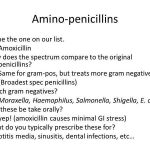
Penicillin G is an acid that is combined with sodium, potassium, procaine, or benzathine to increase its stability or to regulate its absorption. The latter two are “long-acting” forms. Penicillin G is useful in the treatment of streptococcal infections due to S. pyogenes (group A), S. agalactiae (group B), S. pneumoniae, viridans streptococci, Corynebacterium diphtheria, N. meningitidis, many strains of N. gonorrhea, Treponema pallidum, and many anaerobic streptococci, such as peptococcus and peptostreptococcus.
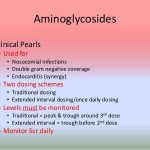
Aminoglycosides are very potent bactericidal antibiotic agents that are active against susceptible aerobic microorganisms. They kill by inhibiting protein synthesis and to some extent by lysing the cell envelope. All the aminoglycosides (streptomycin, kanamycin, neomycin, gentamicin, amikacin, tobramycin, sisomicin, and netilmicin) share common structural features. Streptomycin is used once a day in combination with other antibiotics to treat mycobacterial infections.
Vancomycin and teicoplanin are the only members of this class of antibiotics. Vancomycin is a high-molecular-weight glycopeptide that is bactericidal for gram-positive microorganisms. It inhibits cell-wall synthesis. Given parenterally, it is the drug of choice for methicillin-resistant staphylococcal infections.