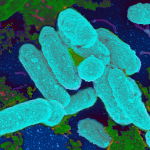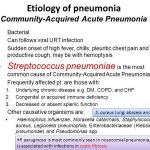
The upper respiratory tract is colonized by several bacterial species that make up the normal flora. Although these commensal organisms can cause disease in certain situations (e.g., in immunocompromised persons), they generally serve a protective function by limiting the growth of other pathogenic bacteria in the respiratory tract. In the lower respiratory tract (LRT), macrophages that can clear foreign particles reside within the alveoli and serve as the final defense against infection.