Description of Medical Condition
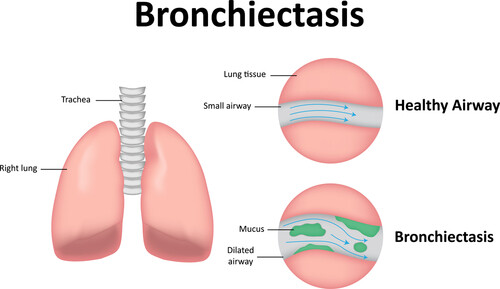
Chronic irreversible, abnormal dilatation of the bronchi, usually accompanied by infection and productive cough System(s) affected: Pulmonary Genetics: Associated with many conditions including some that are congenital or hereditary Incidence/Prevalence in USA:
- No reliable figures available
- Less common than it once was, probably due to more effective treatment of childhood respiratory infections
Predominant age: Begins most often in early childhood, but symptoms may not appear until later in life Predominant sex: Male = Female
Medical Symptoms and Signs of Disease
- Cough
- Sputum — copious and purulent
- Hemoptysis
- Wheezing
- Coarse or moist crackles
- Cyanosis
- Digital clubbing
- Dyspnea
- Barrel chest
- Emaciation
- Fatigue
- Fever
- Recurrent pneumonia
- Tachycardia
- Tachypnea
What Causes Disease?
- Alpha-1 -antitrypsin deficiency
- Allergic bronchopulmonaty aspergillosis
- Bronchial obstruction
- Cystic fibrosis
- Dyskinetic cilia syndromes
- Hypogammaglobulinemia
- Inhaling noxious chemicals
- Kartagener syndrome (situs inversus, sinusitis, immotile spermatozoa, bronchiectasis)
- Necrotizing pulmonary infections
- Pulmonary abscess
- Severe lung infection in childhood (measles, adenovi-rus, influenza, pertussis, or bronchiolitis)
- Tuberculosis
- Congenital immunodeficiency syndromes
- Chronic aspiration
- Rheumatic diseases
- Transplant graft rejection
Risk Factors
- Repeated bouts of pneumonia
- Any chronic respiratory illness
- Retained foreign body
- Immunodeficiency
- Gastroesophageal reflux
- Sinusitis
Diagnosis of Disease
Differential Diagnosis
- Chronic bronchitis
- Chronic obstructive pulmonary disease
- Cystic fibrosis
- Pulmonary tuberculosis
- Allergic bronchopulmonary aspergillosis
Laboratory
- Positive sputum culture (yields H. influenzae, Streptococcus pneumoniae, staphylococcal, klebsiella, pseudomonas, or anaerobes)
- Hypoxemia
- Leukocytosis, usually
- Serum immunoglobulins — check for hypogammaglobulinemia, IgE level helpful
Drugs that may alter lab results: N/A Disorders that may alter lab results: N/A
Pathological Findings
- Bronchial dilation
- Inflamed bronchi
- Purulent bronchorrhea
- Necrosis of bronchial mucosa
- Peribronchial scarring
Special Tests
- Sweat test
- Skin test for aspergillus
- Bronchoscopy useful in locating bleeding site and to exclude adenoma or foreign body
- Ciliary biopsy with electron microscopy (EM)
- Pulmonary function tests show variable obstruction and restriction; include test for reversible component
- Sputum culture/sensitivity, AFB, fungus
Imaging
- CT scan
- Shows dilation and truncation of airways with signet rings prominent in lower lobes
- High resolution CT is best to establish diagnosis and extent of disease
- Spiral CT helpful for questionable findings
- Bronchography has limited role
- Chest x-ray
- Can be normal
- Coarse lung markings — honeycomb/tram tracks
- Air-fluid level
- Cystic lesions
- Atelectasis
Diagnostic Procedures
Fiberoptic bronchoscopy
- Recommended when disease is of recent onset or is unilateral
- May be combined with bronchography
- Obtain culture
Treatment (Medical Therapy)
Appropriate Health Care
Outpatient except for possible surgery
General Measures
- Airway clearance techniques
- Chest physical therapy
- Percussion (mechanical)
- Postural drainage
- Hyd ration
- Onebulized saline
- Pulmonary rehabilitation with inspiratory muscle training
- Noninvasive positive pressure ventilation, nocturnal or chronic
- Bronchoscopy may be required for extraction of mucus or mycelial plugs, or if physiotherapy has failed
- Pulmonary rehabilitation to improve functional status
- Bronchial artery embolization may be lifesaving for massive pulmonary hemorrhage
- Avoid cigarette smoking
- Treat acid reflux if needed
Surgical Measures
Segmental pulmonary resection for localized disease or refractory hemoptysis
Activity
As fully active as possible
Diet
No restrictions
Patient Education
Printed patient information available from: American Lung Association, 1740 Broadway, New York, NY 10019, (212)315-8700
Medications (Drugs, Medicines)
Drug(s) of Choice
- Bronchodilators
- Use chronically to enhance sputum clearance; particularly beneficial with asthma or aspergillosis
- Beta-adrenergic agonists (e.g., albuterol) given by metered dose inhaler with use of a spacer (reservoir device)
- Inhaled corticosteroids
- Use chronically to enhance sputum clearance
- Beclomethasone, fluticasone, etc., given by metered dose inhaler
- Antibiotics. Use early for exacerbations. Continue minimum of 7-10 days. May use culture to guide choice. Chronic prophylaxis not recommended.
- Ciprofloxacin, levofloxacin
- Ampicillin: 250-500 mg orally q 6 hours (50 mg/kg/day in divided doses q 6-8 hours in children less than 20 kg) Trimethoprim-sulfamethoxazole: DSq12h
- Tetracycline: 250-500 mg orally q 6 hours
- Onebulized aminoglycosides — tobramycin 300 mg by aerosol bid
- Steroids
- Consider for patients with bronchopulmonary aspergillosis. IgE level guides steroid dosing.
Contraindications:
Tetracycline: not for use in pregnancy or children < 8 years.
Precautions:
Tetracycline: may cause photosensitivity; sunscreen recommended.
Significant possible interactions:
- Tetracycline: avoid concurrent administration with antacids, dairy products, or iron.
- Broad-spectrum antibiotics: may reduce the effectiveness of oral contraceptives; barrier method recommended.
Alternative Drugs
- For chronic persistent infection, long-term high dose of amoxicillin 3 g every 12 hours may be useful. It does not provide relief for everyone and has more side effects.
- Other broad-spectrum antimicrobials including anti-pseudomonals if required. Choice would depend on pathogen and susceptibility.
- Inhaled corticosteroids if reversible obstruction present
- Oxygen — if P02 < 60 mm Hg
- Nicotine replacement, consider to aid smoking cessation
Patient Monitoring
- Frequent followupfor progress of illness, prevention of infection, smoking cessation, and to check on physiotherapy
- Pulmonary function and C-reactive protein may be monitored to assess inflammation and disease progression
- At some point in followup, need to discuss with patient the possibility of mechanical ventilation and cardiopulmonary resuscitation in the future. The patient, family and provider should determine if this type of treatment is appropriate.
Prevention / Avoidance
- Treat all pneumonias adequately
- Immunizations for viral illnesses (e.g., influenza)
- Immunization for pneumococcal pneumonia
- Routine childhood immunizations (e.g., pertussis, measles, Hib)
- Genetic counseling if inherited etiology
Possible Complications
- Recurrent pulmonary infections
- Pulmonary hypertension
- Secondary amyloidosis
- Cor pulmonale
- Brain abscess
- Massive hemoptysis
- Atelectasis
- Lung abscess
Expected Course / Prognosis
- Chronic. Surgery may be curative if disease localized.
- Average life expectancy — 55 years
- 10% of patients have a rapidly progressive course
Miscellaneous
Associated Conditions
- Sinusitis
- Cor pulmonale
- Kartagener syndrome
- Cystic fibrosis
- Ulcerative colitis
- Marian syndrome
- Ehlers-Danlos syndrome
- Yellow nail syndrome
Age-Related Factors
Pediatric: Cystic fibrosis and other congenital disorders Geriatric: Elderly more likely to need hospitalization for treatment
Pregnancy
N/A
International Classification of Diseases
494.0 Bronchiectasis without acute exacerbation 494.1 Bronchiectasis with acute exacerbation
See Also
Aspergillosis Bronchiolitis obliterans & organizing pneumonia Cystic fibrosis Lung abscess Kartagener syndrome
Other Notes
Conditions that may lead to bronchiectasis include severe pneumonia (especially measles, pertussis, adenoviral infections in children), necrotizing infections due to Klebsiella, staphylococci, influenza virus, fungi, mycobacteria, mycoplasma, bronchial obstruction from any cause (foreign body, carcinoma, enlarged mediastinal lymph nodes.





