Description of Medical Condition
Chronic cough is defined as cough of >3 weeks duration. Patients present for fear of underlying pathology (eg, cancer), annoyance, self-consciousness, hoarseness. Patients with stress urinary incontinence may find cough particularly troubling. COPD and smoking-related cough are most common etiologies at the primary care level.
System(s) affected: Pulmonary, Gastrointestinal
Genetics: N/A
Incidence/Prevalence in USA: Prevalence of 14-23% in nonsmokers
Predominant age: All age groups
Predominant sex: Male = Female
Medical Symptoms and Signs of Disease
- Variable and related to the underlying cause
- Usually nonproductive cough with no other signs or symptoms. May persist up to 6 weeks after resolution of viral illness.
- Possible signs and symptoms of allergic diathesis, rhinitis, sinusitis, GERD, CHF, connective tissue disorders
What Causes Disease?
Often multiple etiologies, but most are related to bronchial irritation. Up to 42% of patients have more than one cause. Most frequent (account for 94% of cases)
- Postnasal drip (PND)
- Asthma
- Gastroesophageal reflex disease (GERD)
- Chronic bronchitis
Other causes:
- Aberrant innominate artery OACE inhibitor therapy
- Aspiration
- Bronchiectasis
- Congestive heart failure
- Cystic fibrosis
- Eosinophilic lung disease
- External auditory canal irritation
- Laryngeal cancer
- Laryngotracheomalacia
- Lung neoplasm (e.g.,, bronchogenic carcinoma)
- Pertussis
- Post-viral bronchial hyperresponsiveness
- Psychogenic (habit cough)
- Restrictive lung disease
- TB, atypical mycobacterium, and other chronic lung infections
Risk Factors
- Smoking
- Stress (particularly school stress in children)
Diagnosis of Disease
Differential Diagnosis
N/A
Drugs that may alter lab results: N/A
Disorders that may alter lab results: N/A
Pathological Findings
Specific to underlying etiology
Special Tests
- Sputum for eosinophils and cytology
- Purified protein derivative (PPD) skin testing
- Pulmonary function testing with beta-2 agonist
- Sweat chloride testing
Imaging
- Chest x-ray
- Chest CT if needed
- Upper Gl series
- Sinus series or sinus CT
Diagnostic Procedures
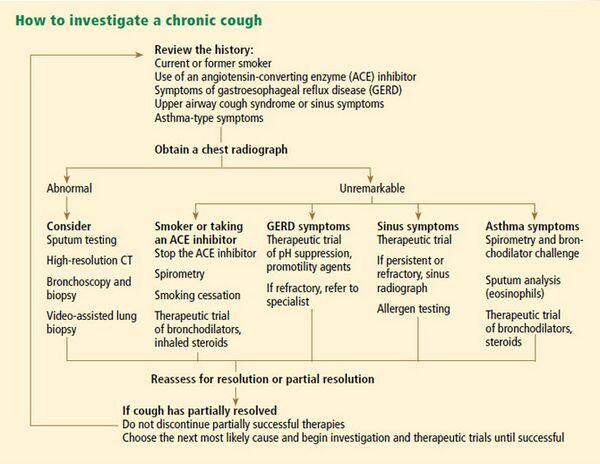
- History and physical
- Age of the patient, presence of associated signs/ symptoms, medical history, medication (ACE inhibitor), environmental exposures, smoking history may make some causes more likely
- Absence of additional signs/symptoms of a particular condition not necessarily helpful (eg, 75% of GERD patients have no other signs or symptoms)
- Character of cough is rarely helpful
- 24 hour pH probe
- Rarely bronchoscopy
- Extensive testing only if indicated by the history and physical. Simple testing (chest x-ray, sinus studies) followed by empiric therapy directed at likely underlying etiology.
Treatment (Medical Therapy)
Appropriate Health Care
Outpatient
General Measures
- Directed at most likely etiology
- Eliminate smoking and ACE inhibitors
- Often empiric treatment of PND and GERD
- Attempt maximal therapy for single most likely cause for several weeks, then search for coexistent etiologies
Surgical Measures
- Fundoplication is often effective for cough secondary to refractory GERD
- Cough secondary to chronic sinusitis may improve post-surgically
Activity
GERD patients may benefit from elevation of head of the bed and elimination of pre-bedtime meals
Diet
GERD patients may benefit from avoidance of EtOH, caffeine, nicotine, citrus, fatty foods
Patient Education
- Reassurance that vast majority of causes are not life threatening, and they can be managed effectively
- Counsel — that several weeks-months may be required for significant reduction or elimination of cough
- Prepare for the possibility of multiple diagnostic tests and therapeutic regimens as treatment is often empiric
Medications (Drugs, Medicines)
Drug(s) of Choice
- Antitussives
- Dextromethorphan (Delsym) 30mg bid, age > 6 years
- Narcotics: codeine 15-30 mg q6h, hydrocodone (Vicodin) 5mg q6h
- Other treatments (antacids, bronchodilators, antibiotics, etc.) directed at etiology of cough
Contraindications: N/A
Precautions: N/A
Significant possible interactions: N/A
Alternative Drugs
N/A
Patient Monitoring
- Frequent followup to assess effectiveness of treatment and addition of other medications as needed
- Consider stepwise withdrawal of medications after resolution of cough
Prevention / Avoidance
N/A
Possible Complications
- Tussive syncope
- Tussive headache
- Stress urinary incontinence
- Abdominal and intercostal muscle strain
- Inguinal hernia
- Pneumothorax
- Medication side-effects
Expected Course / Prognosis
- Most patients (>90%) can be effectively diagnosed and treated with a systematic approach
- Cough from any cause may take weeks to months until resolution, and resolution is highly dependent on efficacy of treatment directed at underlying etiology
Miscellaneous
Associated Conditions
N/A
Age-Related Factors
Pediatric: Habit cough more likely in school-aged children
Geriatric: N/A
Pregnancy
N/A
International Classification of Diseases
786.2 Cough
306.1 Physiological malfunction arising from mental factors, respiratory
491.0 Simple chronic bronchitis
493.90 Asthma, unspecified
See Also
Asthma
Bronchiectasis
Congestive heart failure
Eosinophilic pneumonias
Gastroesophageal reflux disease
Laryngeal cancer
Lung, primary malignancies
Pertussis
Pulmonary edema
Rhinitis, allergic
Sinusitis
Tuberculosis
Other Notes
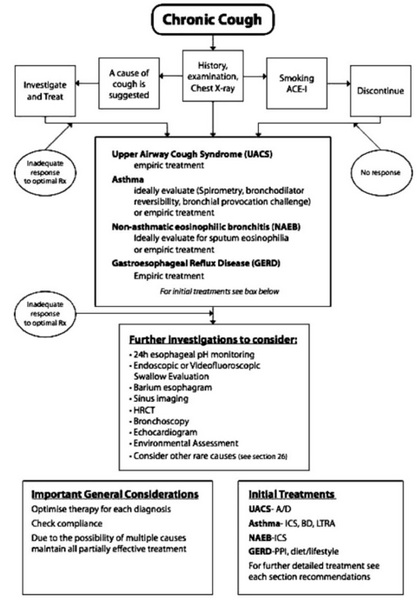
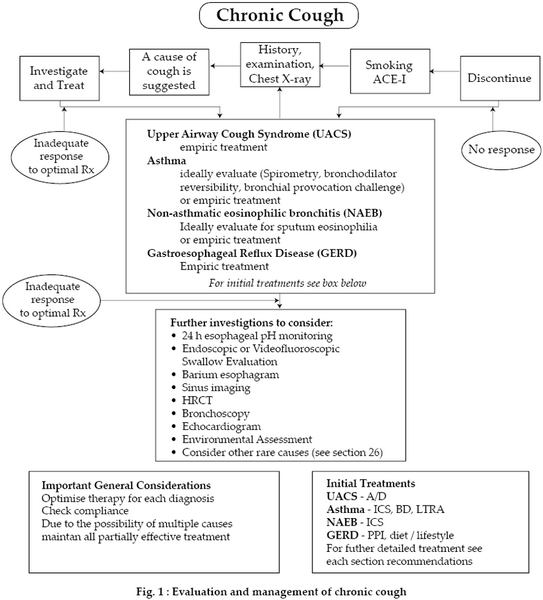
Algorithms for diagnosis and treatment can be found in references
Abbreviations
GERD = Gastroesophageal reflux disease PPI = Proton pump inhibitor MAI = mycobacterium avium-intracellulare PND = Postnasal drip