Description of Medical Condition
Inflammation of the nasal passages due to any number of respiratory viruses. Usually not serious; vast majority are self-treated.
System(s) affected: Pulmonary
Genetics: American Indians and Eskimos at higher risk than other ethnic groups and have more frequent complications such as otitis media; individuals with certain alpha-1-antitrypsin genotypes may be unusually susceptible to the common cold.
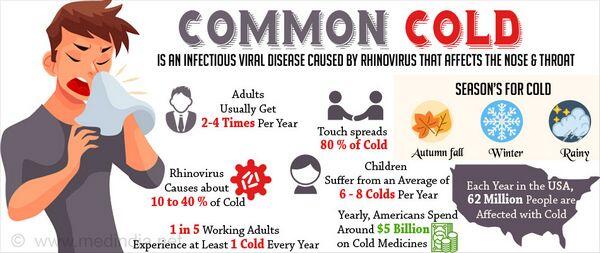
Incidence/Prevalence in USA: Preschool children 6-10 colds/yr; kindergarten 12/yr; schoolchildren 7/yr; adolescents/adults 2-4/yr. National Ambulatory Survey: 31 episodes/100 persons/year (counting only colds that lead to medical attention or at least one day of restricted activity).
Predominant age: Children > adults
Predominant sex: Male = Female
Medical Symptoms and Signs of Disease
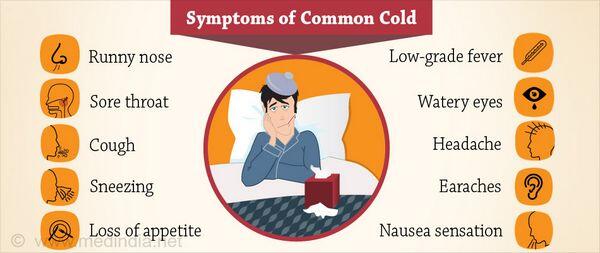
- Nasal stuffiness and/or obstruction (80-100%)
- Sneezing (50-70%)
- Scratchy throat (50%)
- Cough (40%)
- Hoarseness (30%)
- Malaise (20-25%)
- Headache (25%)
- Fever>100°F/37.7°C(0-1%)
What Causes Disease?
Usually due to one of 200 virus strains from six virus families; many strains present within the same geographic region or family
- Rhinovirus (> 200 serotypes)
- Influenza A, B, C viruses
- Parainfluenza viruses
- Respiratory syncytial viruses
- Coronavi ruses
- Adenovi ruses
- Certain ECHO viruses
In 40% of cases, no agent can be identified
Risk Factors
- Exposure to infected individuals
- Touching one’s nose or conjunctiva with contaminated fingers
- Allergic disorders
Diagnosis of Disease
Differential Diagnosis
- Allergic rhinitis
- Mumps
- Rubeola
- Cytomegalovirus
- Epstein-Barr virus
- Mycoplasma pneumonia
- Influenza — systemic symptoms including myalgias, malaise, severe headache and ocular symptoms overshadow the respiratory complaints
Laboratory
- CBC if symptoms persist for more than 10 days or with fever >100°F(37.8°C)
- Nasal smear for eosinophilia may be useful in select individuals
Drugs that may alter lab results: N/A
Disorders that may alter lab results: N/A
Pathological Findings
- Rhinovirus infects the ciliated epithelium lining the nose. Edema and hyperemia of nasal mucous membranes results.
- Exudation of serous and mucinous fluid containing immunoglobulins
- Histology: edema of subepithelial connective tissue, and a scanty cellular infiltrate containing neutrophils. plasma cells, lymphocytes, and eosinophils
- Rhinovirus causes a “non-destructive” inflammation of the mucous membranes, in contrast to influenza and parainfluenza which denude epithelium to the basement membrane
Special Tests
In some centers, rapid antigen tests for various respiratory viruses are available for patients requiring hospitalization or for research purposes
Imaging
Not indicated unless there is concern for bacterial superinfection of the sinuses, supraglottic region, trachea, or lungs
Diagnostic Procedures
In rare cases, may want to attempt to culture virus from nasal washings or identify by ELISA or RIA methods
Treatment (Medical Therapy)
Appropriate Health Care
Outpatient self-care
General Measures
- Rest, fluids, and symptomatic measures
- Reassure that usual course is 6-10 days
- Humidify inspired air
- Discontinue tobacco and alcohol products (if not already done)
- In infants, clear nasal passages with a bulb syringe, position mattress at 45°, use saline nasal drops
Activity
Up as tolerated with increased rest in the first few days
Diet
Encourage fluids
Patient Education
- Reassure that colds are ubiquitous and a normal part of human existence
- Spread is primarily via hand-to-hand transmission of virus contaminated nasal secretions; persons with colds touch their nose and eyes and then touch others
- Small-particle aerosols released in talking, coughing, and sneezing do not travel very far and contain only a low concentration of rhinovirus
- Rhinovirus survives for hours on the hands and hard surfaces, but does not survive long on porous surfaces such as tissues
- Individual susceptibility to colds, depends in large part, on pre-existing antibody levels
- Serum immunity lasts for years, but most individuals gain little protection against future colds due, in part, to the large number of viral serotypes and the antigenic drift that occurs over time in some viral types (rhinovirus, influenza)
- Educate about the expected course and symptomatic measures
- Advise patients to contact you if they develop dyspnea, productive cough, temperature > 102°F (38.9°C), or shaking chills
- Patient informationatwww.niaid.nih.gov/factsheets/ cold.htm
Medications (Drugs, Medicines)
Drug(s) of Choice
- No cure or practical preventive measure documented. Medications targeting a particular symptom reduce the likelihood of adverse systemic effects
- Topical decongestants (sympathomimetics) reduce edema and swelling of the nasal mucosa, promote drainage, and reduce nasal airflow resistance. Preferred over oral because of minimal systemic effects. Sprays preferred over drops in ages > 6. Oxymetazoline
- Adults and children ages 6-12:0.05% solution, 2 or 3 sprays in each nostril bid
- Children ages 2-6: 0.025% solution, 2 or 3 drops in each nostril bid
- Rebound congestion (rhinitis medicamentosa) unlikely if used < 5 days • Topical anticholinergics. Control rhinorrhea but do not relieve nasal congestion or sneezing Olpratropium: Adults and children>11: 0.06%solution, 2 sprays to each nostril TID for 4 days
- Oral decongestants (sympathomimetics). Advantages over topical decongestants: longer duration of action, lack of local irritation and no risk of rhinitis medicamentosa
- Pseudoephedrine
- Adults: 60 mg q4-6h (120 mg sustained release q12h)
- Children ages 6-12:30 mg q4-6h
- Children 2-5:15 mg q4-6h
- Antihistamines. Histamine does not play a significant role in the common cold, but are safe and effective in alleviating sneezing and rhinorrhea. Their perceived benefit may come from anticholinergic effects, drying nasal and pharyngeal secretions and sedative effects promoting rest.
- Chlorpheniramine
- Adults: 4 mg q4-6h (or 8 mg tid, 12 mg bid)
- Children ages 6-12:2 mg q4-6h
- Children ages 2-6:1 mg q4-6h
- Cough suppressants. Cough most likely due to irritation of tracheobronchial receptors by post-nasal drip and may therefore benefit from decongestants. If nonproductive or interferes with sleep or normal activities, a cough suppressant is indicated. Codeine and dextromethorphan exhibit comparable efficacy. Adverse effects: drowsiness and Gl upset.
- Codeine
- Adults: 10-20 mg q4-6h
- Children ages 6-12:5-10 mg q4-6h
- Children ages 2-6: 2.5-5 mg q4-6h
- Dextromethorphan
- Adults: 10-30 mg q4-8h
- Children ages 6-12:15 mg q6-8h
- Children ages 2-6: 2.5-7.5 mg q4-8h
- Expectorants. Though commonly employed, efficacy not proven
- Guaifenesin
- Adults: 100-400 mg q4h
- Children ages 6-12:100-200 mg q4h
- Children ages 2-5: 50-100 mg q4h
Contraindications:
- Oral decongestants — monoamine oxidase inhibitors or selegiline
Precautions:
- Oral decongestants
- Affect all vascular beds and may increase blood pressure. They are cardiac stimulants and may result in arrhythmias. They may increase glucose levels in individuals with glucose intolerance or diabetes mellitus.
- Other adverse effects include headache, nervousness, sleeplessness, and dizziness
- Should be used with caution in patients taking guanethidine
- Antihistamines
- Nasal blockage and sinus congestion may worsen
- Cough suppressants
- Misuse and dependence can occur with codeine, but dextromethorphan abuse by adolescents is reported
- Expectorants
- Liquid preparations may contain high concentrations of alcohol
- Nausea, vomiting or abdominal pain are common adverse effects
Significant possible interactions: See manufacturer’s literature
Alternative Drugs
- Many mouthwashes, gargles and lozenges are promoted to relieve the pain of sore throat. The demulcent effects of hard candy, gargling with warm saline, and products with anesthetics (e.g., benzocaine or phenol), may provide pain relief.
- Aromatic oils (e.g., menthol, camphor, eucalyptus), when applied topically or taken in a lozenge, produce a sensation of increased airflow in the absence of a significant change in airflow resistance.
- Antibacterials are of no value
- Antivirals
- Interieron. Prevents viral invasion of mucosa to prevent colds; side effects include nasal irritation or bleeding in about 10% of patients; may be useful in groups that have close contact
- Zinc chloride. Prevents viral replication in vitro, but efficacy of lozenges unproven
- Vitamin C (ascorbic acid)
- No preventative effects and only a modest (average 23%) reduction in the severity and duration of symptoms.
- Precipitation of urate, oxalate, or cystine stones has been seen, and urine glucose monitoring may be inaccurate in individuals taking large doses
- Interferes with stool guaiac testing
Patient Monitoring
Patients should contact their physician if they develop fever associated with systemic symptoms, difficulty breathing, dyspnea, and/or purulent drainage
Prevention / Avoidance
Frequent hand washing and avoiding touching the face may help prevent colds
Possible Complications
- Lower respiratory tract infection
- Bronchial hyperreactivity
- May lead to decompensation in patients with asthma and chronic lung disease
- Otitis media (2% of colds)
- Acute sinusitis (0.5% of colds)
- Pneumonia
- Rhinitis medicamentosa
Expected Course / Prognosis
Complete recovery expected within 3-10 days
Miscellaneous
Associated Conditions
- Pharyngitis
- Sinusitis
- Bronchitis
- Bronchiolitis
- Pneumonia
- Croup
- Asthma
Age-Related Factors
Pediatric:
- Medications are likely to produce adverse effects or toxicity in young children
- Incidence of colds is highest
Geriatric:
Medications commonly produce adverse effects in the elderly
Pregnancy
- Decongestants: no clear association between drug use and congenital defects
- Antihistamines: no clear association between drug use and congenital defects
- Codeine: indiscriminate use during pregnancy may pose a risk to the fetus
Synonyms
- URI
- Upper respiratory infection
International Classification of Diseases
460 Acute nasopharyngitis (common cold)
See Also
Pharyngitis Mumps
Measles, rubeola Rhinitis, allergic
Cytomegalovirus inclusion disease Epstein-Barr virus infections Pneumonia, mycoplasma Influenza
Abbreviations
- ELISA = enzyme linked immunosorbent assay
- RIA = radioimmunoassay
- URI = upper respiratory infection


