Neisseria gonorrhoeae is a gram-negative diplococcus estimated to cause up to 600,000 infections per year in the United States.
Clinical presentation
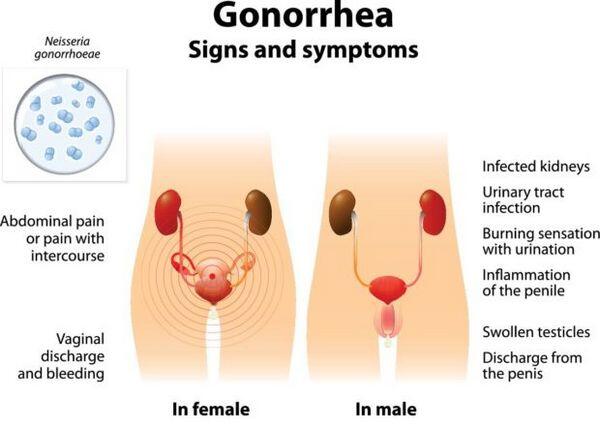
- Infected individuals may be symptomatic or asymptomatic, have complicated or uncomplicated infections, and have infections involving several anatomic sites.
- Approximately 15% of women with gonorrhea develop pelvic inflammatory disease. Left untreated, pelvic inflammatory disease can be an indirect cause of infertility and ectopic pregnancies.
- In 0.5% to 3.0% of patients with gonorrhea, the gonococci invade the bloodstream and produce disseminated disease.
- The usual clinical manifestations of disseminated gonnococcal infection are tender necrotic skin lesions, tenosynovitis, and monoarticular arthritis.
Diagnosis
- Diagnosis of gonococcal infections can be made by gram-stained smears, culture (the most reliable method), or newer methods based on the detection of cellular components of the gonococcus (e.g., enzymes, antigens, DNA, or lipopolysaccharide) in clinical specimens.
- Culture of exposed body areas is the most reliable means of diagnosing gonococcal infection.
- Alternative methods of diagnosis include enzyme immunoassay (enzyme immunoassay), DNA probes, and nucleic acid amplification techniques employing polymerase chain reaction and ligase chain reaction.
Treatment
- All currently recommended regimens are single-dose treatments with various oral or parenteral cephalosporins and fluoroquinolones (Table Treatment of Gonorrhea).
- Ceftriaxone (125 mg intramuscularly) is the only parenteral agent recommended by the Centers for Disease Control as a first-line agent for treatment of gonorrhea.
- Coexisting chlamydial infection, which is documented in up to 50% of women and 20% of men with gonorrhea, constitutes the major cause of postgonococcal urethritis, cervicitis, and salpingitis in patients treated for gonorrhea. As a result, concomitant treatment with doxycycline or azithromycin is recommended in all patients treated for gonorrhea. A single dose of azithromycin (2g) is highly effective against chlamydia.
- Pregnant women infected with Neisseria gonorrhoeae should be treated with either a cephalosporin or spectinomycin, because fluoroquinolones are contraindicated. Erythromycin or amoxicillin is the preferred treatment for presumed Chlamydia trachomatis infection.
- Treatment of gonorrhea during pregnancy is essential to prevent ophthalmia neonatorum. The American Academy of Pediatrics recommends that either silver nitrate (1%), tetracycline (1%), or erythromycin (0.5%) be instilled in each conjunctival sac immediately postpartum to prevent ophthalmia neonatorum.
- Infants born to infected mothers should also receive an intramuscular or intravenous injection of ceftriaxone, 50 mg/kg, for 7 days.
Evaluation of therapeutic outcomes
- Combination gonorrhea/chlamydia therapy rarely results in treatment failures, and routine follow-up of patients treated with a regimen included in the Centers for Disease Control guidelines is not recommended.
Persistence of symptoms following any treatment requires culture of the site(s) of gonorrheal infection, as well as susceptibility testing if gonococci are isolated.



