- The causative organism of syphilis is Treponema pallidum, a spirochete.
- Syphilis is usually acquired by sexual contact with infected mucous membranes or cutaneous lesions, although on rare occasions it can be acquired by nonsexual personal contact, accidental inoculation, or blood transfusion.
Clinical presentation
The clinical presentation of syphilis is varied, with progression through multiple stages possible in untreated or inadequately treat patients (Table Presentation of Syphilis Infections).
Primary Syphilis
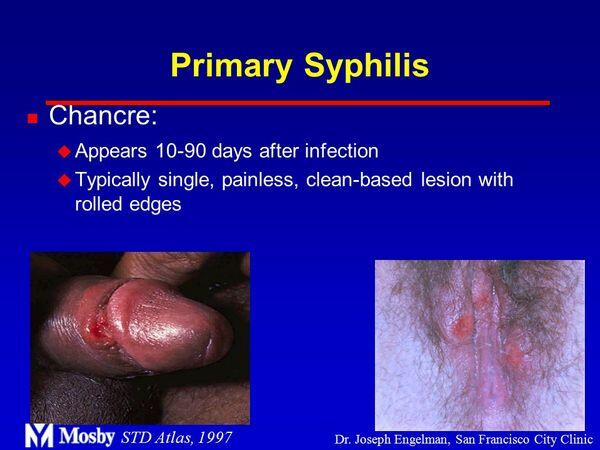
Primary syphilis is characterized by the appearance of a chancre on cutaneous or mucocutaneous tissue. Chancres persist only for 1 to 8 weeks before spontaneously disappearing.
| TABLE. Treatment of Gonorrhea | ||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| TABLE. Presentation of Syphilis Infections | ||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
Secondary Syphilis
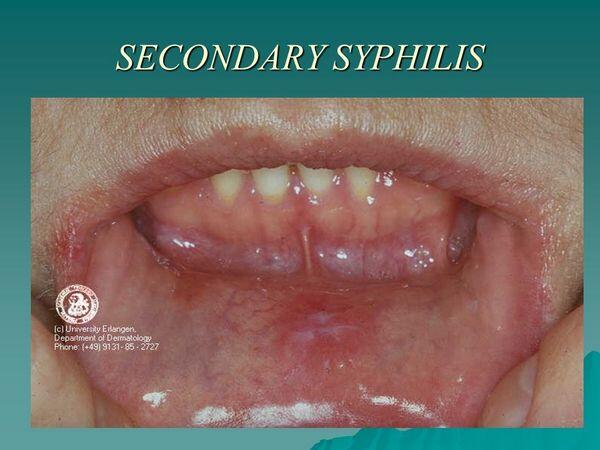
- The secondary stage of syphilis is characterized by a variety of mucocutaneous eruptions, resulting from widespread hematogenous and lymphatic spread of T. pallidum.
- Signs and symptoms of secondary syphilis disappear in 4 to 10 weeks; however, in untreated patients, lesions may recur at any time within 4 years.
Latent Syphilis
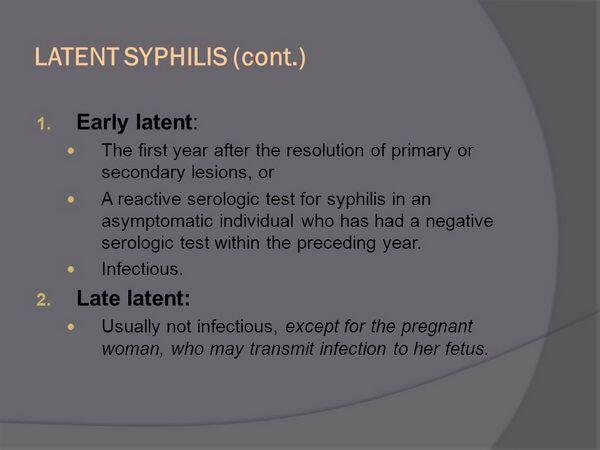
- Persons with a positive serologic test for syphilis but with no other evidence of disease have latent syphilis.
- Most untreated patients with latent syphilis have no further sequelae; however, approximately 25% to 30% progress to either neurosyphilis or late syphilis with clinical manifestations other than neurosyphilis.
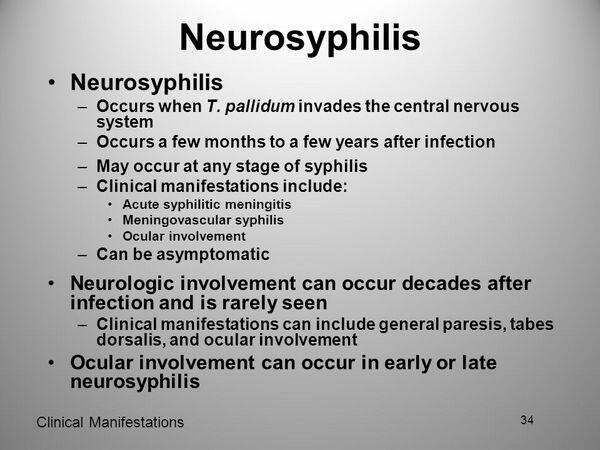
Tertiary Syphilis and Neurosyphilis
Forty percent of patients with primary or secondary syphilis exhibit central nervous system (central nervous system) infection.
Diagnosis
- Because T. pallidum is difficult to culture in vitro, diagnosis is based primarily on dark-field or direct fluorescent antibody microscopic examination of serous material from a suspected syphilitic lesion or on results from serologic testing.
- Serologic tests are the mainstay in the diagnosis of syphilis and are categorized as nontreponemal or treponemal. Commonly used nontreponemal tests include the Venereal Disease Research Laboratory slide test, the rapid plasma reagin card test, the unheated serum regain test, and the tuluidine red unheated serum test
- Treponemal tests are more sensitive than nontreponemal tests and are used to confirm the diagnosis (i.e., the fluorescent treponemal antibody absorption [FTA-ABS]).
Treatment
- Treatment recommendations from the Centers for Disease Control for syphilis are presented in Table Drug Therapy and Follow-up of Syphilis. Parenteral penicillin G is the treatment of choice for all stages of syphilis. Benzathine penicillin G is the only penicillin effective for single-dose therapy.
- Patients with abnormal cerebrospinal fluid findings should be treated as having neurosyphilis.
- For pregnant patients, penicillin is the treatment of choice at the dosage recommended for that particular stage of syphilis. To ensure treatment success and prevent transmission to the fetus, some experts advocate an additional intramuscular dose of benzathine penicillin G, 2.4 million units, 1 week after completion of the recommended regimen.
- The majority of patients treated for primary and secondary syphilis experience the Jarisch-Herxheimer reaction after treatment, characterized by flulike symptoms such as transient headache, fever, chills, malaise, arthralgia, myalgia, tachypnea, peripheral vasodilation, and aggravation of syphilitic lesions.
- The Jarisch-Herxheimer reaction should not be confused with penicillin allergy. Most reactions can be managed symptomatically with analgesics, antipyretics, and rest.
Evaluation of therapeutic outcomes
- Centers for Disease Control recommendations for serologic follow-up of patients treated for syphilis are given in Table Drug Therapy and Follow-up of Syphilis. Quantitative nontreponemal tests should be performed at 6 and 12 months in all patients treated for primary and secondary syphilis and at 6, 12, and 24 months for early and late latent disease.
- For women treated during pregnancy, monthly quantitative nontreponemal tests are recommended in those at high risk of reinfection.



