Description of Medical Condition
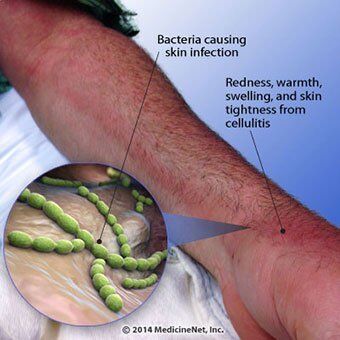
An acute, spreading infection of the dermis and subcutaneous tissue. Several entities are recognized:
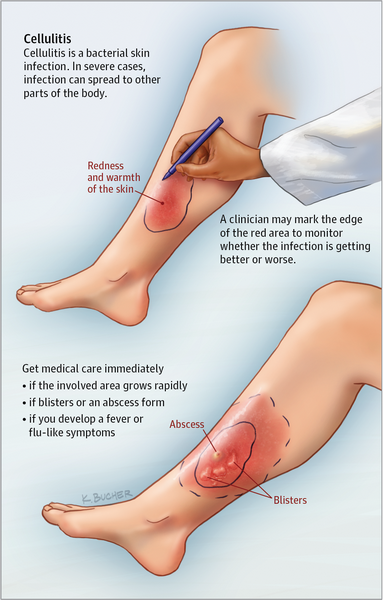
- Cellulitis of the extremities — characterized by an expanding, red, swollen, tender or painful plaque with an indefinite border that may cover a wide area
- Recurrent cellulitis of the leg after saphenous venectomy — patients have an acute onset of swelling, erythema of the legs arising months to years after coronary artery bypass. (Surgery using lower extremity veins for bypass grafts.)
- Dissecting cellulitis of the scalp — recurrent painful, fluctuant dermal and subcutaneous nodules
- Facial cellulitis in adults — a rare event. Patients usually develop pharyngitis, followed by high fever, rapidly progressive anterior neck swelling, tenderness and erythema associated with dysphagia.
- Facial cellulitis in children — potentially serious. Swelling and erythema of the cheek develop rapidly, usually unilateral.
- Perianal cellulitis — bright perianal erythema extending from the anal verge approximately 2 to 3 cm onto the surrounding perianal skin
- Pseudomonas cellulitis — may be a localized phenomenon or it may occur during pseudomonas septicemia
System(s) affected: Skin/Exocrine
Genetics: No known genetic pattern
Incidence/Prevalence in USA: Unknown
Predominant age:
- Perianal cellulitis — principally in children
- Facial cellulitis — in adults, usually older than 50 years. In children, between 6 months and three years.
Predominant sex: Male = Female (perianal cellulitis more common in boys)
Medical Symptoms and Signs of Disease
General
- Local tenderness
- Pain
- Erythema
- Malaise
- Fever, chills
- Involved area is red, hot, and swollen
- Borders of the area are not elevated and not demarcated
- Regional lymphadenopathy is common
Recurrent cellulitis
- Same as above
- Edema
- High fever, chills and toxicity
Dissecting cellulitis of the scalp
- Purulent drainage from burrowing interconnecting abscesses
Facial cellulitis in adults
- Malaise
- Anorexia
- Vomiting
- Itching
- Burning
- Dysplasia
- Anterior neck swelling
Facial cellulitis in children
- Irritability
- Upper respiratory tract infection symptoms
Perianal cellulitis
- Intense perianal erythema
- Pain on defecation
- Blood streaked stools
- Perianal pruritus
What Causes Disease?
By site
- Cellulitis of the extremities: Group A streptococcus, Staphylococcus aureus
- Recurrent cellulitis of the leg: Non-group A beta hemolytic Streptococci (group C,G,B)
- Dissecting cellulitis of the scalp: Staphylococcus aureus
- Facial cellulitis in adults: H. influenzae type B
- Facial cellulitis in children: H. influenzae type B, over 3 years with portal of entry:
- staphylococcal and streptococcal
- Synergetic necrotizing cellulitis: Mixed aerobic-anaerobic flora
- Intravenous drug use: Staphylococcus aureus. Streptococci, Enterobacteriaceae, Pseudomonas, Fungi
- Synergetic necrotizing cellulitis: Mixed aerobic-anaerobic flora
Specific diseases
- Diabetes mellitus: Staphylococcus aureus.
Streptococci, Enterobacteriaceae, Anaerobes
- Human bites: Eikenella corrodens
- Animal bites (cat and dog): Staphylococci, Pasteurella multocida
Patient groups
Oneonates: Group B streptococcus Olmmunocompromised
- Bacteria (Serratia, Proteus and other Enterobacteriaceae)
- Fungi (Cryptococcus neoformans)
- Atypical mycobacterium
- Children with nephrotic syndrome: E. coli
- Environmental and occupational exposures
- Erysipelothrix rhusiopathiae
Vibrio species
- Aeromonas hydrophilia
Rare causes
- Anaerobic
- Clostridium perfringens (gas forming cellulitis)
- Tuberculosis
- Syphilitic gumma
- Fungal: Mucormycosis, Aspergillosis
Risk Factors
General
- Previous trauma (laceration, puncture, human or animal bite)
- Underlying skin lesion (furuncle, ulcer)
- Surgical wound
- Recurrent cellulitis
- Post coronary artery bypass in patients whose saphenous veins have been removed
- Lower extremity lymphedema secondary to a) radical pelvic surgery b) radiation therapy c) neoplastic involvement of pelvic lymph nodes
- Mastectomy
- Diabetes mellitus
- Intravenous drug use
- Immunocompromised host
- Burns
- Environmental and occupational factors
Diagnosis of Disease
Differential Diagnosis
Perianal cellulitis OCandida intertrigo
- Psoriasis
- Pinworm infection
- Inflammatory bowel disease
- Behavioral problem
- Child abuse
Others
- Acute gout
- Fasciitis/myositis
- Mycotic aneurysm
- Ruptured Baker’s cyst
- Thrombophlebitis
- Osteomyelitis OHerpetic whitlow
- Cutaneous diphtheria
- Pseudogout
Laboratory
- Aspirates from the point of maximum inflammation. Yield a 45% positive culture rate as compared to a 5% from leading edge culture.
- Blood cultures — potential pathogens isolated in 25% of patients
- Mild leucocytosis with a left shift
- A mildly elevated sedimentation rate
- CBC
Drugs that may alter lab results: Previous antibiotic therapy may alter the results
Disorders that may alter lab results: N/A
Pathological Findings
Biopsy of skin shows marked infiltration of the dermis with eosinophils and inflammatory changes
Special Tests
- Serial serological testing with antistreptolysin 0, anti-deoxyribonuclease B, and anti-hyaluronidase tests may be successful in diagnosing cellulitis caused by group A, C, or G hemolytic streptococci
- Sinus drainage and culture of aspirate
Imaging
Gas forming cellulitis
- Plain x-rays show gas bubbles in the soft tissue
- CT shows gas and myonecrosis
Diagnostic Procedures
- Skin biopsy
- Lumbar puncture should be considered for all children with H. influenzae type B cellulitis
Treatment (Medical Therapy)
Appropriate Health Care
Outpatient for mild cases, inpatient for severe infections
General Measures
- Immobilization and elevation of the involved limb to reduce swelling may be needed in H. influenzae type B
- Sterile saline dressings to decrease local pain
- Moist heat to localize the infection
- Cool aluminum acetate (Burow’s solution) compresses for pain relief
Surgical Measures
- Debridement for gas/purulent collections
- Intubation or tracheotomy may be needed for cellulitis of the head or neck
- Hand infections — wide filleting incision in necrotizing cellulitis
Activity
Ambulatory in mild infection; bedrest in severe infection
Diet
Regular diet
Patient Education
- Good skin hygiene
- Avoid skin traumas
- Report early skin changes to physician
Medications (Drugs, Medicines)
Drug(s) of Choice
Treat 10-30 days. Guided by culture results whenever possible.
- Mild early suspected streptococcal etiology: Aqueous penicillin G, 600,000 U, then IM procaine penicillin at 600,000 Uq8-12hrs
- Staphylococcal infection or no clues to etiology: penicil-linase-resistant penicillin (e.g., oxacillin 0.5-1.0 g poq6 hrs)
- Severe infection: penicillinase-resistant penicillin (e.g. nafcillin 1.0-1.5 g IV q4 hrs)
- Gram negative bacillus as possible etiology: aminogly-coside (gentamicin) plus a semisynthetic penicillin
- Rapidly progressive cellulitis after a fresh water injury: penicillinase-resistant penicillin plus gentamicin or chloramphenicol
- Human bites: amoxicillin-clavulanate (Augmentin)
- Animal bites (cellulitis at the saphenous site): penicillin or nafcillin, in high dosage, IV for 7 days before switching to oral therapy
- Facial cellulitis in adults and children: (H. influenza B) cefotaxime IV
- Gas forming cellulitis: Aqueous penicillin G 10-20 million U/day IV
- Diabetes mellitus: Cefoxitin or if toxic, clindamycin and gentamicin
- Intravenous drug abuse: Vancomydn and gentamicin
- Compromised hosts: clindamycin and gentamicin
- Burn patients: vancomycin and gentamicin
Contraindications: Allergies to the antibiotic
Precautions: Renal failure, other organ failure
Significant possible interactions: Refer to manufacturer’s literature
Alternative Drugs
Mild infection
- Penicillin allergy: erythromycin, 500 mg po q6 hrs
Severe infection
- Vancomycin 1.0-1.5 g/day IV
- Human bite and animal bites: IV cefoxitin
Gas forming cellulitis
- Metronidazole 500 mg IV q6h
- Clindamycin 600 mg IV q8h
Fluoroquinolones (adults)
Patient Monitoring
- A blood culture at the end of treatment to ensure cure
- Repeat needle aspirate culture
- Repeat blood count if patient was toxic
- Repeat lumbar puncture in case of meningitis
Prevention / Avoidance
- Treatment of tinea pedis with antifungal (such as clotrimazole) will prevent recurrent cellulitis of the legs in patients who have had coronary bypass
- Avoid trauma
- Avoid swimming in fresh water or salt water in the presence of skin abrasion
- Avoid human or animal bite
- Support stocking with peripheral edema
- Good skin hygiene
- For recurrent cellulitis — prophylactic penicillin G (250-500 mg po bid)
- H. influenzae cellulitis — rifampin prophylaxis for entire family of index case or in day-care classroom in which one or two children exposed. Dosage: 20 mg/kg/day (maximum: 600 mg/day) for 4 days.
Possible Complications
- Bacteremia
- Local abscesses
- Super infection with gram negative organisms
- Lymphangitis especially in recurrent cellulitis
- Thrombophlebitis of lower extremities in older patients
- Dissecting cellulitis of the scalp — scarring; alopecia
- Facial cellulitis in children — meningitis in 8% of patients
- Gas forming cellulitis — gangrene; amputation; 25% mortality
Expected Course / Prognosis
With adequate antibiotic treatment, outlook is good
Miscellaneous
Associated Conditions
Facial cellulitis in children
- Upper respiratory tract infection
- Unilateral or bilateral otitis media in 68% of patients
- Meningitis in 8% of patients
Perianal cellulitis
- Pharyngitis may precede the infection
Frontal sinus in adult OSubacute bacterial endocarditis
- Scarlet fever
- Vaccinia
- Herpes simplex
- Herpes zoster
Age-Related Factors
Pediatric: N/A
Geriatric: In cellulitis of lower extremities, patients are more prone to develop thrombophlebitis
Pregnancy
N/A
International Classification of Diseases
682.9 Cellulitis and abscess at unspecified site
See Also
Cellulitis, periorbital & orbital Erysipelas Animal bites Thrombophlebitis, superficial



