Description of Medical Condition
Pre-invasive neoplastic epithelial changes in the transformation zone of the uterine cervix often associated with human papilloma virus infections
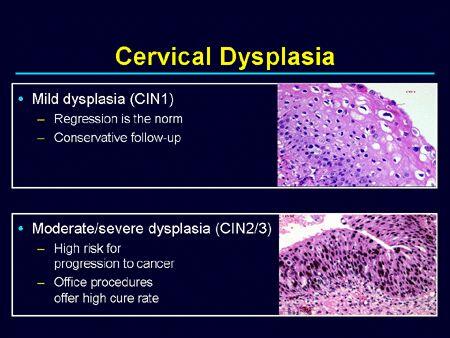
- Mild dysplasia (CIN I or SIL low grade) — cellular changes are limited to the lower one-third of the squamous epithelium
- Moderate dysplasia (CIN II or SIL high grade) — cellular changes are limited to the lower two-thirds of the squamous epithelium
- Severe dysplasia (CIN III or SIL high grade or carcinoma in situ) — cellular changes involves the full thickness of the squamous epithelium
System(s) affected: Reproductive
Genetics: N/A
Incidence/Prevalence in USA: Difficult to assess due to wide variability in false negative Papsmear reporting and uneven distribution of qualified colposcopy practitioners. Prevalence 3,600/100,000 at age 27-28.
Predominant age: The median age for carcinoma in situ is 28 years. Earlier lesions can be expected at younger ages
Predominant sex: Female only
Medical Symptoms and Signs of Disease
- Frequently none
- Occasionally associated with condyloma acuminata in the vulva, vagina, or anus
- Occasionally there are co-existing sexually transmitted diseases in the lower reproductive tract, e.g. chlamydia, gonorrhea
What Causes Disease?
Strong linkage with infections by human papilloma viruses types 16,18, 31, 33, and 35. Other types of the same virus have also been implicated.
Risk Factors
- Multiparity and pregnancy before age 20 years
- Multiple sexual partners
- Early age in first sexual intercourse
- Condyloma acuminatum infection elsewhere in the body
- Cigarette smoking
- Prostitution
- Lower socioeconomic status
Diagnosis of Disease
Differential Diagnosis
- Invasive carcinoma of the cervix
- Condyloma acuminatum
Laboratory
Pap smear
Drugs that may alter lab results:
Surgical lubricants e.g., K-Y Jelly
Disorders that may alter lab results: N/A
Pathological Findings
- Clumping of the nuclear chromatin material
- Reversal of the nuclear/cytoplasmic ratio
- Koilocytosis
- Hyperchromasia
Special Tests
- Viral DNA hybridization (Virapap) and others
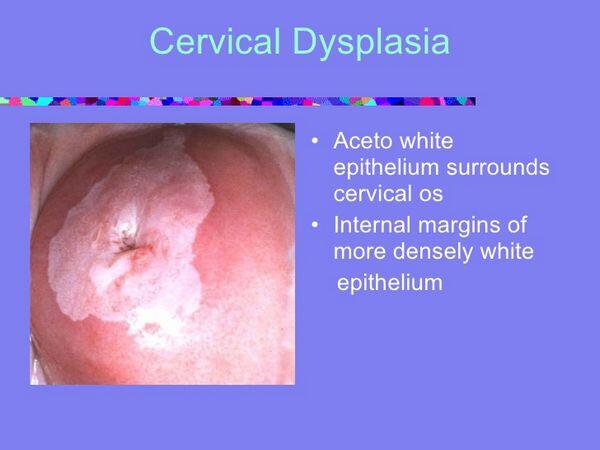
- Colposcopy
- PAPNET system to review negative Pap smears
- CYTYC 2000 thin prep Pap test (replacement of current Pap preparations)
Diagnostic Procedures
- Papanicolaou smear
- Colposcopy and directed cervical biopsies
- Cone biopsy (by cold knife, laser, or loop excision)
- Endocervical curettage
- Loop electrosurgical excision procedure (LEEP)
- Cervicography
- Speculum examination
- Use of HPV DNA typing to select certain cases with borderline abnormalities, e.g., atypical squamous cells of undetermined significance (ASCUS), for closer fol-lowup and colposcopy
Treatment (Medical Therapy)
Appropriate Health Care
Outpatient
General Measures
Office evaluation and observation
Surgical Measures
Outpatient surgery — cryotherapy, laser ablative or excisional cone, cold knife cone, electrosurgical loop excision of transformation zone
Activity
Four weeks of pelvic rest after cone biopsy
Diet
No restriction
Patient Education
See Followup section
Medications (Drugs, Medicines)
Drug(s) of Choice
- Treatment is primarily surgical
- Fluorouracil (Efudex) once or twice daily as 5% vaginal cream supplemental therapy
Contraindications: Hypersensitivity to 5-fluorouracil
Precautions:
- If hand is used in application of 5-fluorouracil, wash hand immediately afterwards
- Avoid contact of 5-fluorouracil with eyes, nose, or mouth
Significant possible interactions: N/A
Alternative Drugs
N/A
Patient Monitoring
Repeat Pap smears every 4 months during the first year after cone excision for severe dysplasia, every 6 months thereafter. For lesser lesions, repeat Pap smear yearly. Probe endocervical canal to assure patency.
Prevention / Avoidance
- Monogamy of both sexual partners
- Use of condom during coitus if unable to practice monogamy
- Abstain from smoking
- Emphasize importance of yearly Pap smears for patients
- Ability to obtain skilled colposcopy service as needed
- Patient education (individually or by community services) to emphasize the need for Pap smear
- Educate medical care providers to make patient referrals for the screening service unless they provide it themselves
Possible Complications
- Some severe dysplasia will progress to invasive carcinoma of the cervix
- Possible complications following cone biopsy of the cervix:
- Hemorrhage
- Infection
- Cervical stenosis
- Cervical incompetence
- Infertility
- Incomplete excision of dysplastic tissue
- Recurrence
Expected Course / Prognosis
- Generally excellent
- Persistence of dysplasia can occur due to incomplete excision
- Recurrence of dysplasia can occur due to inability to eradicate the human papilloma virus in the patient’s body or prevent new infections
Miscellaneous
Associated Conditions
- Condyloma acuminatum
- Carcinoma of the cervix
Age-Related Factors
Pediatric: Very rare
Geriatric: Less frequent
Others: This is usually a problem for the women in the reproductive age group. The median age is 28 years for severe dysplasia. For lesser lesions, the median ages tend to be much lower.
Pregnancy
- Dysplasia may progress during pregnancy
- It is important to determine the severity of dysplasia and to exclude the presence of invasive carcinoma during pregnancy
- Dysplasia does not require definitive treatment during pregnancy
- Dysplasia by itself is not an indication for cesarean section
International Classification of Diseases
622.1 Dysplasia of cervix (uteri)
See Also
Abnormal Pap smear Condyloma acuminata Cervical malignancy
Other Notes
Squamous intraepithelial lesion (SIL) is in reference to Pap smear only
Abbreviations
CIN = cervical intraepithelial neoplasia SIL = squamous intraepithelial lesion


